Sites of Drug Action
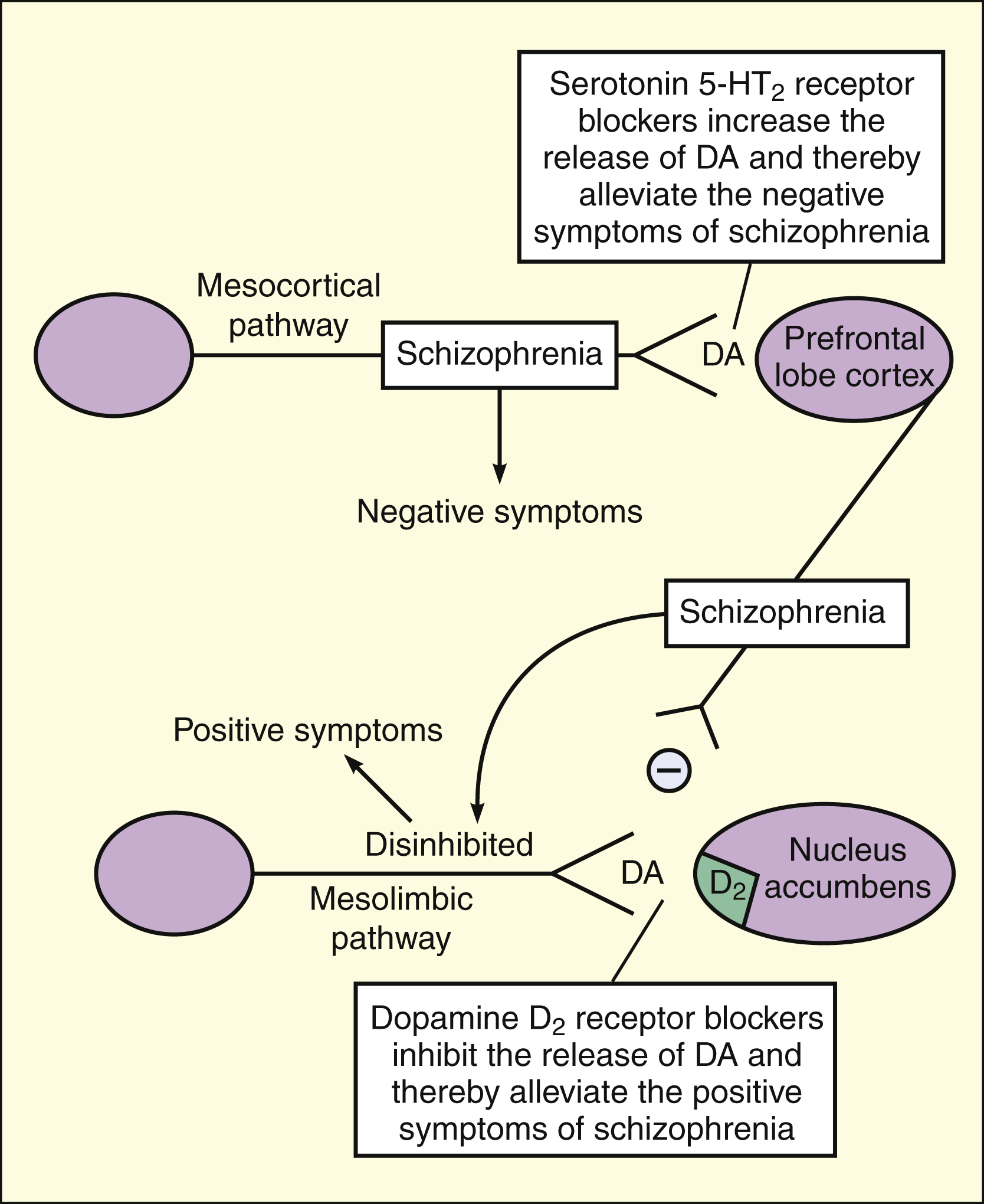
Some antipsychotic drugs (e.g., clozapine, olanzapine, and risperidone) block serotonin 5-HT2 receptors in the mesocortical pathway to the prefrontal lobe cortex. This increases the release of dopamine (DA) and thereby alleviates the negative symptoms of schizophrenia. Most antipsychotic drugs (including those listed above) block dopamine D2 receptors in the mesolimbic pathway to the nucleus accumbens, and this alleviates the positive symptoms of schizophrenia.
Several observations support the dopamine hypothesis. First, most antipsychotic drugs block dopamine D2 receptors, and an excellent correlation exists between the clinical potency of these drugs and their in vitro binding affinity for these receptors. Second, drugs that act by increasing the neuronal release of dopamine (amantadine) or by blocking the reuptake of dopamine (drugs such as amphetamines and cocaine) can induce psychotic behavior that resembles the behavior of schizophrenic patients.
Dopamine turnover in the brain, which reflects the neuronal release of dopamine, can be studied by measuring the concentration of the principal metabolite of dopamine, homovanillic acid, in the cerebrospinal fluid. Although elevated levels of homovanillic acid are not found in patients with chronic schizophrenia, they are found in some schizophrenic patients having acute psychotic episodes. Evidence also exists for a dopamine receptor defect in schizophrenic patients. Positive emission tomography scanning using D2 receptor ligands has revealed that schizophrenic patients have decreased D2 receptor densities in the prefrontal lobe cortex (but increased D2 receptor densities in the caudate nucleus). These findings lend overall support to the dopamine hypothesis, although it is clear from the clinical effectiveness of atypical antipsychotics that 5-hydroxytryptamine (5-HT2) and other types of dopamine receptors may be involved.
ANTIPSYCHOTIC DRUGS
Antipsychotic drugs are agents that reduce psychotic symptoms and improve the behavior of schizophrenic patients. Antipsychotic drugs were also called neuroleptic drugs because they suppress motor activity and emotional expression. The accidental discovery of the antipsychotic properties of chlorpromazine in the early 1950s began a new era in the treatment of schizophrenia and stimulated research concerning the neurobiology of mental illness and psychopharmacology. Nearly 40 years later, the introduction of clozapine had an equally important impact. Clozapine was the first agent to show greater activity against the negative symptoms of schizophrenia and to produce significantly fewer extrapyramidal side effects than the previous antipsychotic drugs. For this reason, the discovery of clozapine has stimulated the development of new antipsychotic drugs with improved pharmacologic properties.
Drug Properties
MECHANISM OF ACTION
The antipsychotic drugs interact with multiple neurotransmitter systems. Whereas the therapeutic effects of these drugs are believed to result from competitive blockade of dopamine receptors and serotonin (5-HT) receptors, the adverse effects are attributed to the blockade of a variety of receptors (Table 22–2).
TABLE 22–2 Mechanisms Responsible for the Therapeutic and Adverse Effects of Antipsychotic Drugs
| Mechanism | Therapeutic Effects | Adverse Effects |
|---|---|---|
| Blockade of α1-adrenoceptors | — | Dizziness, orthostatic hypotension, and reflex tachycardia |
| Blockade of dopamine D2 receptors | Alleviation of positive symptoms of schizophrenia | Extrapyramidal effects (akathisia, dystonia, and pseudoparkinsonism) and elevated serum prolactin levels |
| Blockade of dopamine D4 receptors | Alleviation of negative symptoms of schizophrenia and decrease in the incidence of extrapyramidal side effects | — |
| Blockade of histamine H1 receptors | —(sedation)∗ | Drowsiness and increase in appetite and weight |
| Blockade of muscarinic receptors | — | Blurred vision, constipation, dry mouth, and urinary retention |
| Blockade of serotonin 5-HT2 receptors | Alleviation of negative symptoms of schizophrenia and decrease in the incidence of extrapyramidal side effects | Anxiety and insomnia |
∗ Sedation may be considered a therapeutic effect with a typical antipsychotic administered for acute psychosis.
Typical antipsychotic drugs have an equal or greater affinity for D2 receptors than for 5-HT2 receptors. As shown in Figure 22–1, an excellent correlation exists between the clinical potency of these drugs and their in vitro affinity for D2 receptors. Whereas antagonism of D2 receptors in mesolimbic pathways is thought to repress the positive symptoms of schizophrenia, blockade of D2 receptors in the basal ganglia is believed to be responsible for the parkinsonian and other extrapyramidal side effects that sometimes occur in patients taking antipsychotic drugs.
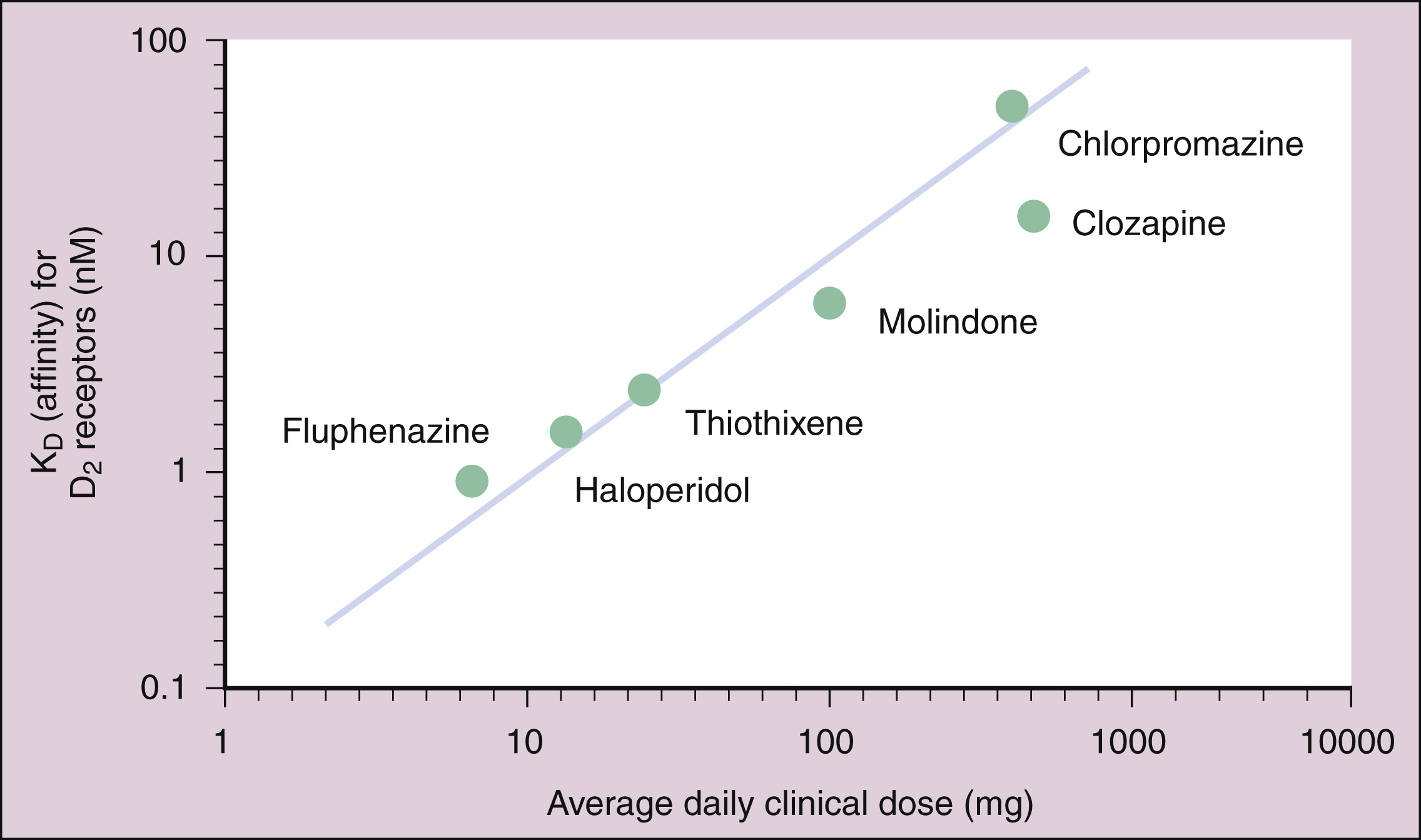
Figure 22–1 Correlation of antipsychotic drug potency and dopamine D2 receptor binding. The clinical potency of the typical antipsychotic drugs is highly correlated with their in vitro affinity for D2 (but not D1) receptors.
Atypical antipsychotic drugs (e.g., clozapine) have a greater affinity for 5-HT receptors than for D2 receptors, and some atypical drugs have increased the affinity for D3 or D4 receptors.
PHARMACOLOGIC EFFECTS
The mechanisms by which the blockade of dopamine and serotonin receptors alleviates the symptoms of schizophrenia are not completely understood. Whereas these receptors are blocked immediately when antipsychotic drugs are first administered, the therapeutic effects of the drugs usually require several weeks to fully develop. This is because antipsychotic drugs produce three time-dependent changes in dopamine neurotransmission. When first administered, the drugs cause an increase in dopamine synthesis, release, and metabolism. This probably represents a compensatory response to the acute blockade of postsynaptic dopamine receptors produced by antipsychotic drugs. Over time, continued dopamine receptor blockade leads to inactivation of dopaminergic neurons and produces what has been called depolarization blockade. Depolarization blockade results in reduced dopamine release from mesolimbic and nigrostriatal neurons. This action is believed to alleviate the positive symptoms of schizophrenia while causing extrapyramidal side effects. Eventually, the reduction in dopamine release caused by depolarization blockade leads to dopamine receptor up-regulation and supersensitivity to dopamine agonists. This supersensitivity may contribute to the development of a delayed type of extrapyramidal side effect called tardive dyskinesia (see below).
BOX 22–2 THE CASE OF THE PARANOID POLICEMAN
CASE PRESENTATION
A 24-year-old male employed as a policeman locks himself in an interrogation room, waving his handgun, and yelling incoherent statements like “They aren’t going to take me alive” and “Get out of my head.” His partner tells the police chief that he has been acting strangely, talking about a conspiracy against him by the other policemen, and arriving for work in dirty clothes and unshaven. He was overheard talking and arguing with himself in the locker room that morning, and the partner says they almost got into a fight just minutes ago because the partner wouldn’t agree to shoot him when he insisted that he “wouldn’t be hurt and was immortal.” A medical emergency team arrives on the scene and at a moment when he is sitting in the corner cowering in fear, they forcibly enter the room, disarm him, and inject haloperidol into his thigh. He is transported to the locked ward of a psychiatric hospital and diagnosed with paranoid schizophrenia.
CASE DISCUSSION
Schizophrenia afflicts about 1 in 100 males and can be one of the most dangerous of all mental disorders as it causes its victims to lose touch with reality. They often show signs of confusion, inability to make decisions, auditory hallucinations, delusions, neglect of personal hygiene, strange statements or behavior, and changes in eating or sleeping habits, energy level, or weight. In the paranoid form of this disorder, schizophrenics develop delusions of persecution or personal grandeur. The first sign of paranoid schizophrenia usually surfaces between the ages of 15 and 30, and schizophrenia is much more common in males than females. There is no cure, but the disorder can be controlled with antipsychotic medications like haloperidol. Haloperidol is a good choice for acute psychotic episodes as it is rapidly absorbed and has a high bioavailability after intramuscular injection, with plasma levels reaching their maximum within 20 minutes after injection.
In mesocortical and nigrostriatal pathways, 5-HT2 receptors mediate presynaptic inhibition of dopamine release. Blockade of these receptors by atypical antipsychotic drugs may increase dopamine release in these pathways. In the mesocortical pathway, this action may alleviate the negative symptoms of schizophrenia. In the nigrostriatal pathway, increased dopamine release counteracts the extrapyramidal side effects caused by D2 receptor blockade.
ADVERSE EFFECTS
In the peripheral autonomic nervous system, antipsychotic drugs also block muscarinic receptors and α1-adrenoceptors, thereby causing adverse effects described in Tables 22-2 and 22-3. Antagonism at α1-adrenoceptors produces dizziness, orthostatic hypotension, and reflex tachycardia. Muscarinic receptor antagonism produces blurred vision, dry mouth, constipation, and urinary retention. Antagonism of brain H1 receptors produces drowsiness and weight gain.
The most disturbing adverse effect is the development of motor abnormalities following the administration of high-potency, typical antipsychotics. These and other adverse effects specific to particular agents are discussed below.
Neuroleptic malignant syndrome is a severe form of drug toxicity that occurs in 0.5% to 1% of patients treated with antipsychotic drugs. It is a life-threatening condition characterized by muscle rigidity, elevated temperature (>38° C), altered consciousness, and autonomic dysfunction (tachycardia, diaphoresis, tachypnea, and urinary and fecal incontinence). The syndrome resembles malignant hyperthermia triggered by halogenated anesthetics in its rapid onset and mortality rate. Neuroleptic malignant syndrome is managed by immediately discontinuing treatment with the offending antipsychotic drug, administering dantrolene to prevent further muscle abnormality (see Chapter 21), and providing supportive care. If future antipsychotic therapy is required in patients who have experienced this syndrome, an atypical drug should be used because the atypical drugs are associated with a lower incidence of neuroleptic malignant syndrome.
INDICATIONS
Antipsychotic agents are primarily used to treat schizophrenia and other forms of psychosis, including drug-induced psychosis and psychosis associated with the manic phase of bipolar disorder. They are also used to treat severely agitated patients, including those with dementia and severe mental retardation. Because the phenothiazines have antiemetic activity, some of them are used in the management of nausea and vomiting (see Chapter 28).
Drug Classification
Antipsychotic drugs were traditionally classified on the basis of their chemical structure, but they are also classified according to whether they display typical or atypical pharmacologic properties. The typical antipsychotic drugs are also considered first-generation antipsychotic agents and the atypical antipsychotic drugs, second-generation antipsychotic agents.
Typical Antipsychotic Agents
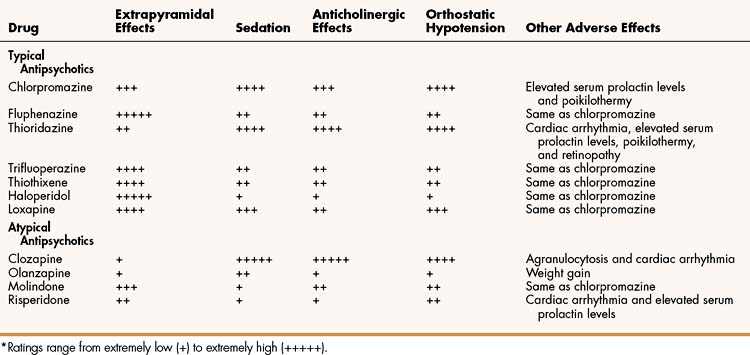
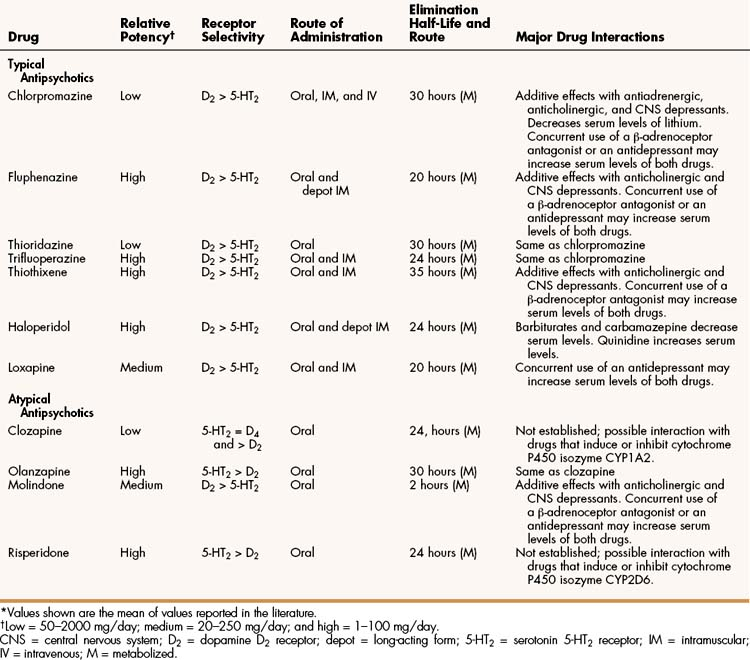
Numerous typical antipsychotics are available for the treatment of schizophrenia and related conditions. The four representative examples discussed in detail here are chlorpromazine, fluphenazine, thioridazine, and haloperidol. These drugs have similar therapeutic effects but differ in their relative potency (Table 22–4) and in their side effect profiles (see Table 22–3).
PHARMACOKINETICS
The typical antipsychotics are adequately absorbed from the gut after oral administration. Severalagents are also administered parenterally, including long-acting depot preparations for intramuscular injection. These agents are extensively metabolized to a large number of active and inactive metabolites before they are excreted in the urine, and they have elimination half-lives ranging from 20 to 30 hours (see Table 22–4).
MECHANISMS AND PHARMACOLOGIC EFFECTS
The typical antipsychotic drugs exert their therapeutic effects primarily due to D2 receptor antagonism. After therapy is initiated, the positive symptoms of schizophrenia usually subside in 1 to 3 weeks. Patients become less agitated and experience fewer auditory hallucinations. Grandiose or paranoid delusions subside and can disappear completely in some patients with continued treatment. At the same time, sleeping and eating patterns become normalized, and behavioral improvement occurs in the form of decreased hostility, combativeness, and aggression. Typical antipsychotic drugs can have some impact on negative symptoms, but it is usually less pronounced than the impact of atypical antipsychotic drugs.
Chlorpromazine and thioridazine are considered low-potency agents, fluphenazine has a slightly greater potency, and haloperidol is a high-potency antipsychotic agent.
ADVERSE EFFECTS
The most common adverse effects produced by typical antipsychotic drugs are summarized in Table 22–3.
Blockade of dopamine receptors in the striatum can cause several forms of extrapyramidal side effects, including akathisia, pseudoparkinsonism, and dystonias. Patients with akathisia, or “motor restlessness,” feel compelled to pace, shuffle their feet, or shift positions and are unable to sit quietly. Pseudoparkinsonism resembles idiopathic Parkinson’s disease and is characterized by rigidity, bradykinesia, and tremor. Dystonia is a state of abnormal muscle tension that often affects the neck and facial muscles, including the tongue, pharynx, larynx, and eyes. Patients with dystonia can experience severe reactions, such as oculogyric crisis (a condition in which the eyeballs become fixed in one position, usually upward), glossospasm, tongue protrusion, and torticollis (a contracted state of the cervical muscles, producing twisting of the neck and an unnatural position of the head). Such reactions can be frightening and painful, and pharyngolaryngeal dystonias can be life threatening. Young males who are given large doses of high-potency drugs are at great risk of developing dystonias.
Although akathisia, pseudoparkinsonism, and dystonias are acute extrapyramidal side effects that often occur early in the course of treatment with antipsychotic drugs, tardive dyskinesia is a disorder that usually develops after months or years of treatment. The disorder is characterized by abnormal oral and facial movements (e.g., tongue protrusion and lip smacking). In later stages, abnormal limb and truncal movements may also be observed. Investigators believe that tardive dyskinesia results from supersensitivity to dopamine, which develops during long-term dopamine receptor antagonism (see Chapter 18). This hypothesis is supported by the fact that the symptoms of tardive dyskinesia temporarily subside if dopamine receptor blockade is increased by giving larger doses of an antipsychotic drug. This approach, however, eventually leads to further receptor supersensitivity and worsening of the manifestations of tardive dyskinesia.
Typical antipsychotic agents can increase serum prolactin levels by blocking dopamine receptors in the tuberoinfundibular pathway (see Box 22–1) and thereby cause gynecomastia in men and menstrual irregularities in women. Via their effects on the hypothalamus, antipsychotic drugs sometimes impair thermoregulation and cause poikilothermy, a condition in which the body temperature tends to approach the ambient temperature. This can lead to hyperthermia (including heat stroke) or hypothermia. In addition, high doses of thioridazine can cause pigmentary retinopathy and cardiac toxicity.
TREATMENT OF ADVERSE EFFECTS
Acute extrapyramidal effects (akathisia, pseudoparkinsonism, and dystonias) that are caused by typical antipsychotic drugs can be managed by lowering the drug dosage, changing to an atypical antipsychotic drug, or administering an additional drug to counteract the adverse effects. Drugs that counteract the effects include benztropine, an anticholinergic drug; diphenhydramine, an antihistamine with significant anticholinergic activity; and amantadine, an agent that increases dopamine release in the basal ganglia and can be used in conjunction with an anticholinergic drug.
Tardive dyskinesia is not easily managed and does not necessarily subside if a causative drug is discontinued. Hence, prevention is important. To prevent tardive dyskinesia, antipsychotic drugs should be used in the lowest doses for the shortest period of time required to control symptoms of schizophrenia. The drugs should be discontinued periodically to assess the need for continued treatment and possibly to reduce the development of dopamine supersensitivity. Patients should be evaluated regularly for early signs of tardive dyskinesia, which are sometimes reversible. Tardive dyskinesia often becomes irreversible if it is not detected early or is allowed to persist.
Once detected, tardive dyskinesia is best managed by reducing the dosage of antipsychotic medication. This results in significant improvement in many patients. No drugs are approved for the treatment of tardive dyskinesia, but some success has been reported with the use of amantadine, dopamine receptor agonists, and clozapine. Other drugs that may be effective include physostigmine, an indirect-acting cholinergic agonist, and the benzodiazepines.
INTERACTIONS
The major drug interactions of antipsychotic agents are listed in Table 22–4. The interactions include additive effects on CNS depression when used with other CNS drugs and pharmacokinetic interactions caused by antipsychotics and other drugs existing as substrates for the same cytochrome P450 isozymes.
Chlorpromazine and Thioridazine
Chlorpromazine and thioridazine are low-potency phenothiazines with similar properties. Of the two agents, thioridazine produces greater anticholinergic effects, and this probably accounts for its tendency to cause fewer extrapyramidal side effects.
Fluphenazine
Fluphenazine is a relatively high-potency typical antipsychotic agent that produces fewer autonomic side effects but more extrapyramidal side effects than do low-potency antipsychotics. Fluphenazine is available in a long-acting depot preparation that is intended for intramuscular injection every 1 to 3 weeks and is useful for treating patients who are not compliant with oral medication or are unable to take oral drugs.
Haloperidol
The first of the high-potency agents and one of the most widely used typical antipsychotics agents is haloperidol. Haloperidol has properties similar to those of fluphenazine and can cause significant extrapyramidal side effects (see Tables 22-3 and 22-4). As with fluphenazine, haloperidol is available in a long-acting depot preparation for intramuscular administration. Haloperidol is extensively metabolized in the liver, and its metabolites are excreted in the urine and bile.
In addition to its use in treating psychoses (e.g., schizophrenia), haloperidol is used in the treatment of Tourette’s syndrome (Gilles de la Tourette’s syndrome). This syndrome is characterized by facial and vocal tics, coprolalia (compulsive use of obscene words, particularly those related to feces), and echolalia (repetition of another person’s words or phrases).
Atypical Antipsychotic Agents
Clozapine and olanzapine are atypical antipsychotics that produce fewer extrapyramidal side effects than do other antipsychotic drugs. Another member of this class, quetiapine, was recently approved for the treatment of schizophrenia and for acute manic episodes associated with bipolar disorder, as either monotherapy or adjunct therapy to lithium or valproate (see later text).
Clozapine
Clozapine has a unique profile of pharmacologic and clinical effects. It was the first of a new generation of atypical antipsychotic drugs that cause significantly fewer extrapyramidal side effects while exhibiting greater activity against the negative symptoms of schizophrenia.
Because clozapine is a potent antagonist of a large number of receptors, it has been difficult to attribute its effects to a particular mechanism of action. It seems likely that its therapeutic effects result from blockade of D4 receptors and 5-HT2 receptors. Both of these actions may contribute to its greater efficacy against the negative symptoms of schizophrenia and to its lower incidence of extrapyramidal side effects. The use of clozapine is associated with significant sedation and autonomic side effects. These adverse reactions are caused by antagonism of histamine, muscarinic, and α1-adrenoceptors. The use of clozapine is also associated with a 1.3% first-year incidence of potentially fatal agranulocytosis. For this reason, the U.S. Food and Drug Administration requires weekly monitoring of leukocyte counts during the first 6 months of therapy, the period during which the risk of agranulocytosis is greatest. After 6 months, biweekly monitoring of leukocyte counts is required.
Olanzapine
Olanzapine is a chemical analog of clozapine. Its pharmacologic properties are similar to those of clozapine, but olanzapine causes fewer autonomic side effects and has not been reported to cause agranulocytosis. As with clozapine, olanzapine causes few extrapyramidal side effects.
Olanzapine has about twice the affinity for 5-HT2 receptors as it does for D2 receptors, and it can block dopamine D3 and D4 receptors. Although it also blocks histamine, muscarinic, and α1-adrenoceptors, it does so to a lesser extent than does clozapine.
Clinical trials indicate that olanzapine is as effective as haloperidol in alleviating the positive symptoms of schizophrenia, is superior to haloperidol in alleviating the negative symptoms, and produces significantly fewer extrapyramidal side effects than does haloperidol. The most common adverse reactions to olanzapine are sedation and weight gain. At higher doses, olanzapine can cause akathisia, pseudoparkinsonism, and dystonias.
Risperidone
Risperidone is a newer atypical antipsychotic drug. Its pharmacologic properties are similar to those of olanzapine, but it appears to cause less sedation, more orthostatic hypotension, and a higher incidence of extrapyramidal side effects than does olanzapine. Its effects on treating both the positive and negative symptoms of schizophrenia are caused by antagonism at both D2 and serotonin (5-HT2A) receptors. In some patients, risperidone elevates levels of serum prolactin. It also lengthens the QT interval seen on the electrocardiogram and can predispose patients to cardiac arrhythmias, including torsades de pointes. Another agent sharing the pharmacologic profile of risperidone is ziprasidone. A newer agent, aripiprazole, differs slightly in that it is a partial agonist at dopamine receptors but a 5-HT receptor antagonist. Paliperidone is the major active metabolite of risperidone and shares its pharmacologic activity as an antagonist at both D2 and 5-HT2A receptors. Paliperidone is available in a once-a-day formulation using osmotic drug-release technology to deliver a controlled amount of drug throughout the 24-hour period.
Molindone
Molindone is an atypical antipsychotic with a unique spectrum of pharmacologic activities. It appears to cause a relatively low incidence of autonomic side effects and sedation. Although its incidence of extrapyramidal side effects also appears to be relatively low, it is probably higher than that of the newer atypical antipsychotic agents when they are given in equivalent doses. Molindone has a relatively short half-life but is metabolized to active and inactive compounds that have a longer half-life. Molindone is sometimes effective in patients who do not tolerate or respond to other drugs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree