Figure 28–1 Physiology of gastric acid secretion and sites of drug action. Gastric acid is secreted by the proton pump (H+,K+-ATPase) located in the luminal membrane of parietal cells. H+,K+-ATPase is stimulated by histamine, acetylcholine, and gastrin, and it is irreversibly blocked by the proton pump inhibitors (lansoprazole and omeprazole). The effect of histamine is blocked by H2 receptor antagonists (cimetidine, famotidine, and ranitidine). Prostaglandins (e.g., misoprostol) inhibit gastric acid secretion and stimulate secretion of mucus and bicarbonate by epithelial cells. Sucralfate binds to proteins of the ulcer crater and exerts a cytoprotective effect, whereas antacids (aluminum and magnesium hydroxides and calcium carbonate) neutralize acid in the gastric lumen. cAMP = cyclic adenosine monophosphate; G = gastrin receptor; H2 = histamine H2 receptor; M3 = muscarinic M3 receptor; PG = prostaglandin receptor.
The principal physiologic stimulants of gastric acid secretion are gastrin, acetylcholine, and histamine. Gastrin is a hormone secreted by G cells in the gastric antrum, whereas acetylcholine is released from vagus nerve terminals. Gastrin and acetylcholine directly stimulate acid secretion by parietal cells, and they also stimulate the release of histamine from paracrine (enterochromaffin-like) cells. Histamine stimulates H2 receptors located on parietal cells and provokes acid secretion via cyclic adenosine monophosphate (cAMP) stimulation of the proton pump (H+,K+-ATPase).
The vagus nerve mediates the cephalic phase of gastric acid secretion evoked by the smell, taste, and thought of food. Gastrin mediates the gastric phase of acid secretion evoked by the presence of food in the stomach. Histamine contributes to the cephalic and gastric phases of acid secretion, and it also mediates basal acid secretion in the fasting state.
The level of gastric acidity can be reduced either by neutralizing gastric acid with antacids or by inhibiting gastric acid secretion with a histamine H2 receptor antagonist or a proton pump inhibitor.
Histamine H2 Receptor Antagonists
The H2 receptor antagonists, or H2 blockers, include cimetidine, famotidine, and ranitidine.
CHEMISTRY, MECHANISMS, AND EFFECTS
The structure of H2 blockers is similar to that of histamine (Fig. 28–2), and this enables the drugs to compete with histamine for binding to H2 receptors on gastric parietal cells (see Fig. 28–1). The H2 blockers have been shown to be potent inhibitors of both meal-stimulated secretion and basal secretion of gastric acid. When they reduce the volume and concentration of gastric acid, they produce a proportionate decrease in the production of pepsin because gastric acid catalyzes the conversion of inactive pepsinogen to pepsin. The H2 blockers also reduce the secretion of intrinsic factor, but not enough to significantly reduce vitamin B12 absorption. They have no effect on gastric emptying time, esophageal sphincter pressure, or pancreatic enzyme secretion.
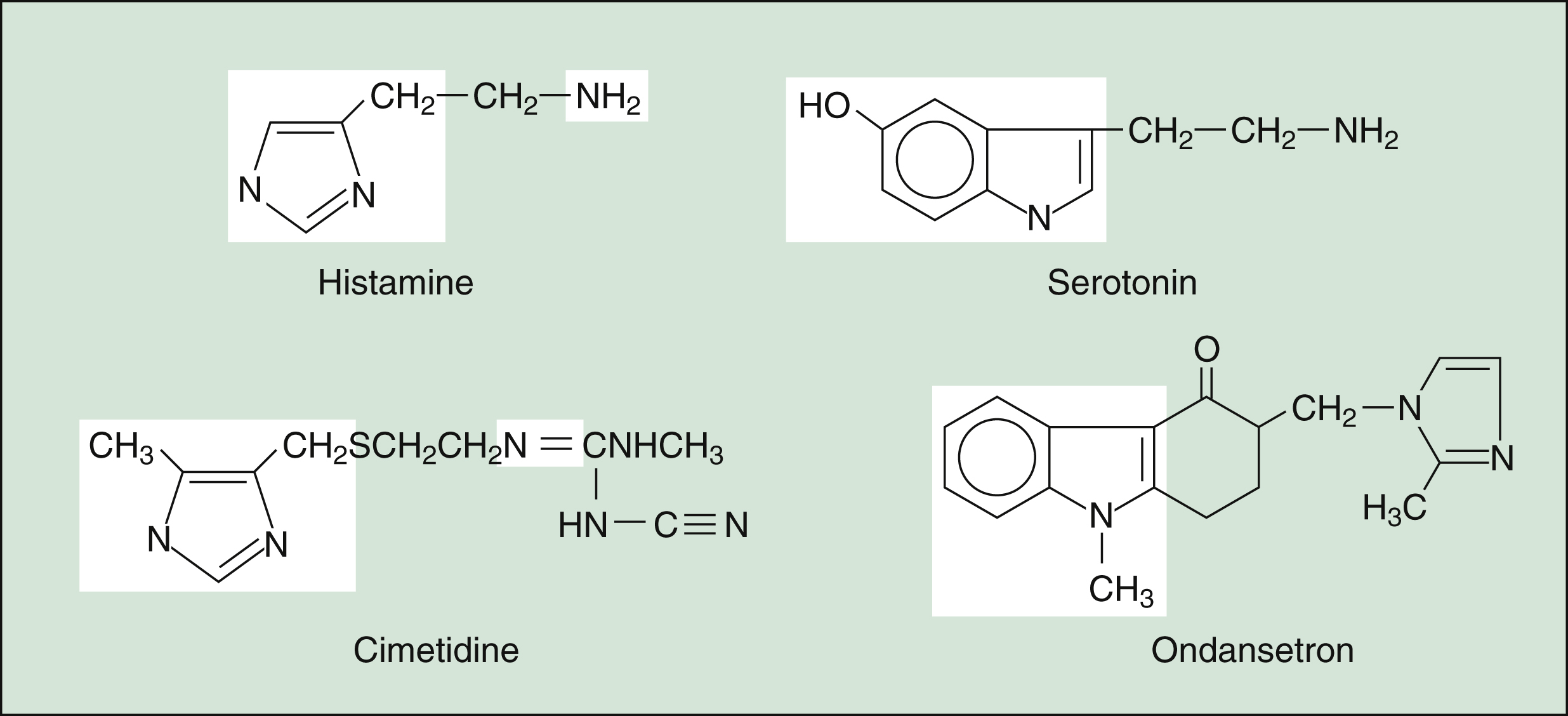
Figure 28–2 Structures of histamine and serotonin and their antagonists. Cimetidine is a histamine H2 receptor antagonist whose structure is similar to that of histamine. Ondansetron is a serotonin 5-HT3 receptor antagonist whose structure is similar to that of serotonin. The parts of the structures that are similar are unshaded.
PHARMACOKINETICS
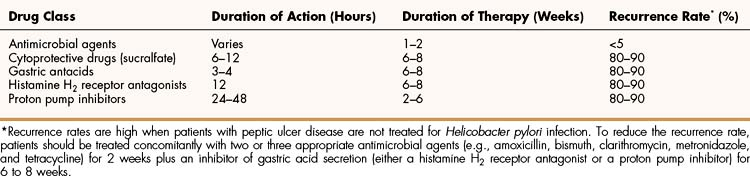
The H2 blockers are well absorbed from the gut and undergo varying degrees of hepatic inactivation before being excreted in the urine. Although the half-life of most H2 blockers is only 2 to 3 hours, their duration of action is considerably longer (Table 28–1), and these drugs are usually administered once or twice daily.
INDICATIONS
The H2 blockers are used to treat conditions associated with excessive acid production, including dyspepsia, peptic ulcer disease, and gastroesophageal reflux disease (GERD). An H2 blocker is also occasionally used in combination with an H1 blocker for the treatment of allergic reactions that do not respond when an H1 blocker is used alone.
Dyspepsia, or heartburn, is characterized by epigastric discomfort following meals. It is often associated with impaired digestion and excessive stomach acidity. Several low-dose formulations of H2 receptor antagonists are available as nonprescription drugs for the prevention and treatment of dyspepsia. These formulations are most effective when taken 30 minutes before ingestion of a dyspepsia-provoking meal.
For the treatment of peptic ulcer disease, H2 blockers are administered once or twice daily at doses that raise the gastric pH above 4 for at least 13 hours a day. Most authorities recommend giving a single daily dose at bedtime to ensure that acid secretion is suppressed all night. Proton pump inhibitors are usually preferred for treating peptic ulcer disease because they heal 80% to 100% of ulcers in 4 weeks, whereas H2 blockers require 6 to 8 weeks to achieve this level of efficacy.
ADVERSE EFFECTS AND INTERACTIONS
Cimetidine has weak antiandrogenic activity and can cause gynecomastia in elderly men, but this reaction is uncommon with other H2 blockers. The fact that the H2 blockers have proved remarkably nontoxic has led to their approval as nonprescription drugs.
Cimetidine is a well-known inhibitor of cytochrome P450 isozymes CYP2C9, CYP2D6, and CYP3A4. These isozymes are involved in the metabolism of numerous drugs, including alprazolam, carbamazepine, cisapride, disopyramide, felodipine, lovastatin, phenytoin, saquinavir, triazolam, and warfarin. The dosage of these drugs may need to be reduced in patients taking cimetidine. Other H2 blockers do not inhibit P450 enzymes significantly and are preferred for patients receiving concomitant drug therapy.
Proton Pump Inhibitors
The proton pump inhibitors include esomeprazole, omeprazole, pantoprazole, and rabeprazole.
CHEMISTRY AND PHARMACOKINETICS
The proton pump inhibitors are acid-labile prodrugs that are administered orally as sustained-release, enteric-coated preparations. After they are absorbed from the gut, the drugs are distributed to the secretory canaliculi in the gastric mucosa and converted to active metabolites that bind to the proton pump. These drugs are eventually metabolized to inactive compounds in the liver, primarily by cytochrome P450 CYP2C19, and these compounds are excreted in the urine and feces. Persons with the CYP2C19 extensive metabolizer phenotype may require higher doses of proton pump inhibitors to cure peptic ulcer.
MECHANISMS AND EFFECTS
The active metabolites of proton pump inhibitors form a covalent disulfide link with a cysteinyl residue in the proton pump (H+,K+-ATPase) located in the luminal membrane of gastric parietal cells (see Fig. 28–1). The drugs irreversibly inhibit the proton pump and to prevent the secretion of gastric acid for an extended period of time. The drugs can produce a dose-dependent inhibition of up to 95% of gastric acid secretion, and a single dose can inhibit acid secretion for 1 to 2 days. Hence, the proton pump inhibitors are more efficacious than the H2 blockers for most conditions (see Table 28–1).
INDICATIONS
Proton pump inhibitors (PPIs) are highly effective in treating peptic ulcer disease. They typically heal 80% to 100% of peptic ulcers in 4 weeks when used in combination with antibiotics, whereas H2-blocker combinations heal 70% to 80% in 4 weeks.
PPIs are the drugs of choice for patients with Zollinger-Ellison syndrome, a condition characterized by severe ulcers resulting from gastrin-secreting tumors (gastrinomas). Higher doses are required for treating patients with this condition than for treating patients with typical peptic ulcer disease.
PPIs are also the most effective drugs for treating GERD. Omeprazole is available in a nonprescription product for the treatment of dyspepsia and heartburn. Finally, PPIs can be used to prevent peptic ulcers and bleeding in persons receiving high-dose or long-term therapy with NSAIDs such as diclofenac.
ADVERSE EFFECTS
Proton pump inhibitors are usually well tolerated. Minor gastrointestinal and central nervous system (CNS) side effects have occurred in some patients, and skin rash and elevated hepatic enzyme levels have also been reported. Many patients with GERD have been treated for several years without significant side effects.
Gastric Antacids
Gastric antacids chemically neutralize stomach acid. This raises the gastrointestinal pH sufficiently to relieve the pain of dyspepsia and acid indigestion and to enable peptic ulcers to heal. The most commonly used antacids are aluminum and magnesium hydroxides and calcium carbonate. These substances are available in chewable tablets and in liquid suspensions. When used alone, aluminum hydroxide can cause constipation, whereas magnesium hydroxide often causes diarrhea. For this reason, the combination of aluminum and magnesium hydroxides usually has a relatively neutral effect on gastrointestinal motility. Calcium carbonate can also cause constipation, and large doses of calcium carbonate can lead to a rebound in acid secretion.
Antacids are available without a prescription and are commonly used to treat acid indigestion and dyspepsia. Nonprescription products containing a low dose of a histamine H2 antagonist and an antacid are also available for this purpose. Antacids were formerly used to treat peptic ulcers, but they must be taken in large doses at frequent intervals for this purpose, and nocturnal acid secretion is particularly difficult to control with antacids. Hence, they are seldom used in treating peptic ulcer today.
CYTOPROTECTIVE DRUGS
Sucralfate and misoprostol both protect the gastrointestinal mucosa, but they do so by different means (see Fig. 28–1).
Sucralfate
CHEMISTRY, MECHANISMS, AND EFFECTS
Sucralfate is a viscous polymer of sucrose octasulfate and aluminum hydroxide. This sulfated polysaccharide adheres to ulcer craters and epithelial cells, and it inhibits pepsin-catalyzed hydrolysis of mucosal proteins. Sucralfate also stimulates prostaglandin synthesis in mucosal cells. These actions contribute to the formation of a protective barrier to acid and pepsin and thereby facilitate the healing of ulcers.
PHARMACOKINETICS
Sucralfate is administered orally as a tablet or suspension. The drug is not absorbed significantly from the gut, and it is primarily excreted in the feces. Patients absorb a small amount of aluminum from the drug, so sucralfate should be used cautiously in patients with renal impairment.
INDICATIONS
In the management of peptic ulcer disease, sucralfate can be used to treat active ulcers or to suppress the recurrence of ulcers. Because it is somewhat less effective than drugs that inhibit gastric acid secretion, it is primarily used in patients who cannot tolerate H2 blockers or proton pump inhibitors.
ADVERSE EFFECTS AND INTERACTIONS
Although sucralfate causes very few systemic adverse effects, constipation and other gastrointestinal disturbances and laryngospasm have been reported occasionally. The use of sucralfate can impair the absorption of other drugs (e.g., digoxin, fluoroquinolones, ketoconazole, and phenytoin). To prevent this problem, sucralfate should be ingested 2 hours before or after these other drugs are taken.
Misoprostol
As discussed in Chapter 26, misoprostol is a prostaglandin E1 analogue. The drug exerts a cytoprotective effect by inhibiting gastric acid secretion and promoting the secretion of mucus and bicarbonate. It is primarily indicated for the prevention of gastric and duodenal ulcers in patients who are taking NSAIDs on a long-term basis for the treatment of arthritis and other conditions. Because misoprostol is expensive, it is usually reserved for patients at high risk of NSAID-induced ulcers, including the elderly and those with a history of peptic ulcer disease.
Misoprostol is administered orally 4 times daily with food for the duration of NSAID therapy. Diarrhea and intestinal cramping are the most common adverse effects, but other gastrointestinal reactions can also occur.
Misoprostol can stimulate uterine contractions and induce labor in pregnant women, so its use is contraindicated during pregnancy.
Muscarinic Receptor Antagonists
Historically, atropine was used to treat peptic ulcer disease, but large doses of the drug are required to inhibit gastric acid secretion, and these doses caused numerous side effects such as blurred vision, urinary retention, and many others. Pirenzepine is a selective muscarinic M1 receptor antagonist that inhibits histamine release from gastric paracrine cells and causes fewer side effects than atropine. It is available in Canada but not in the United States for treating peptic ulcer disease.
Atropine, hyoscyamine, dicyclomine, and other muscarinic blockers are used as antispasmodic agents to temporarily relieve intestinal cramping and pain and other symptoms of intestinal hyperactivity.
DRUGS FOR HELICOBACTER PYLORI INFECTION
Studies show that 80% to 90% of patients who undergo monotherapy with a gastric acid inhibitor have an ulcer recurrence within 1 year after discontinuing this therapy. In contrast, less than 5% of patients who undergo therapy with both a gastric acid inhibitor and an agent to eliminate H. pylori have an ulcer recurrence. Hence, combination therapy is now the standard of care.
The currently recommended treatments for peptic ulcer disease consist of a gastric acid secretion inhibitor (usually a proton pump inhibitor) and two or more of the following agents: amoxicillin, bismuth, clarithromycin, metronidazole, tetracycline, or levofloxacin.
Short-course treatments of 10 to 14 days duration (and possibly 7 days or less) consist of twice daily omeprazole or lansoprazole plus amoxicillin and clarithromycin. Metronidazole may be substituted for amoxicillin in persons allergic to penicillins. Alternative short-course regimens include twice daily ranitidine bismuth citrate (a single drug), plus clarithromycin and tetracycline. Another regimen consists of pantoprazole plus amoxicillin and levofloxacin. These regimens eradicate H. pylori in 80% to 90% of cases of duodenal ulcers (see Box 28–1).
BOX 28–1 A CASE OF BURNING EPIGASTRIC PAIN
CASE PRESENTATION
A 50-year-old man complains to his physician of a burning epigastric pain that has awakened him at night for the past 3 weeks. The pain often begins in the late morning and is relieved by food or antacids, but reappears about 3 hours after a meal and during sleep. He has been otherwise healthy and his vital signs and physical exam are normal. Blood samples are taken for routine chemistries and blood cell counts. A rapid urease test for H. pylori is positive, and he is scheduled for gastrointestinal endoscopy, which reveals an inflamed ulcer in the wall of the duodenal bulb. A gastric mucosal biopsy confirms the presence of H. pylori. The patient denies any drug allergies and is placed on triple therapy with 40 mg/day of omeprazole, 2 g/day of amoxicillin, and 1000 mg/day of clarithromycin, all of which are divided into 2 daily doses and given for 2 weeks. His symptoms improve markedly after several days of therapy and endoscopy confirms ulcer healing after completion of his treatment.
CASE DISCUSSION
Helicobacter pylori infec-tion is responsible for most cases of duodenal ulcer. Epigastric pain is the most common symptom, which is usually relieved by food but often awakens a patient at night. Several tests for H. pylori are available, including the rapid urease test. Endoscopy is a valuable tool for determining the type and location of a peptic ulcer and enables biopsy to distinguish simple gastric ulcers from stomach cancer. It can also identify a bleeding ulcer and permit laser probe coagulation to stop bleeding. The treatment of ulcers caused by H. pylori has been continuously improved and 1- or 2-week treatments using a proton pump inhibitor and two antibiotics are highly effective. Amoxicillin and clarithromycin are the antibiotics of choice for this indication.
Four-week treatments for duodenal peptic ulcer consist of a once-daily proton pump inhibitor plus antimicrobial agents. Histamine H2 blockers or sucralfate may also be effective in 4 weeks or longer when given in combination with antibiotics. Longer (8 weeks) treatments are usually required for treating gastric ulcers.
The properties of antimicrobial agents are discussed in the chapters of Section VII.
DRUGS FOR INFLAMMATORY BOWEL DISEASES
The two most common inflammatory bowel diseases are ulcerative colitis and Crohn’s disease. In ulcerative colitis, inflammation of the gastrointestinal mucosa is limited to the colon and rectum. In Crohn’s disease, inflammation is transmural and can occur in any part of the gastrointestinal tract.
Abdominal cramping and diarrhea are the most common complaints of patients with inflammatory bowel disease. Many patients experience acute exacerbations separated by periods of remission, but prolonged illness can occur in persons with severe disease. Ulcerative colitis and Crohn’s disease are generally treated with glucocorticoids, mesalamine, and infliximab.
Glucocorticoids
Hydrocortisone and other glucocorticoids (see Chapter 33) have been extensively used for the treatment of both ulcerative colitis and Crohn’s disease. In cases of mild ulcerative colitis, they may be effectively administered as rectal enemas. In cases of Crohn’s disease and more severe ulcerative colitis, they are usually administered orally or parenterally.
Glucocorticoids are often able to induce the remission of ulcerative colitis or Crohn’s disease, but they have proved less valuable in maintaining remission, particularly without causing significant toxicity.
Aminosalicylates
Sulfasalazine and its active metabolite, mesalamine, are used to induce and maintain the remission of ulcerative colitis, but they are less effective in maintaining remission of Crohn’s disease.
Sulfasalazine is a modified sulfonamide compound that is not well absorbed from the gut. In the gastrointestinal tract, bacteria convert sulfasalazine to 5-aminosalicylic acid (5-ASA, or mesalamine) and sulfapyridine. Although 5-ASA is believed to mediate the anti-inflammatory effects of sulfasalazine, the exact mechanism is uncertain. Some investigators hypothesize that 5-ASA acts by inhibiting prostaglandin synthesis or by inhibiting the migration of inflammatory cells into the bowel wall. Others hypothesize that 5-ASA is a superoxide-free radical scavenger.
Mesalamine can be administered as a rectal suppository, rectal suspension, or delayed-release oral tablet. It acts primarily in the gut, but about 15% of the drug is absorbed into the circulation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree