OVERVIEW
Endoparasitic infections are extremely common in many parts of the world, particularly in areas where the climate is warm and moist, the sanitation is poor, and insects and other vectors of disease are prevalent. In fact, billions of people in tropical and subtropical regions are infected with protozoa (single-cell organisms that dwell in the lumen, tissue, or blood) and helminths (worms, including nematodes, trematodes, and cestodes). Factors, such as immigration, an increase in the number of international travelers, and an increase in the number of individuals who have acquired immunodeficiency syndrome (AIDS) and are therefore at greater risk for opportunistic infections, have all increased the probability that physicians will see endoparasitic infections that were rarely found in their usual patient population.
Since 1960, the introduction of new drugs has enabled remarkable advances in the chemotherapy of some endoparasitic infections. Albendazole and mebendazole have significantly improved the treatment of several intestinal nematode infections, whereas praziquantel has revolutionized the treatment of trematode and cestode infections. At the same time, metronidazole and tinidazole have provided more-effective and less-toxic drugs for the treatment of amebiasis, giardiasis, and trichomoniasis. The sites and mechanisms of action of selected antiparasitic drugs are depicted in Figure 44–1.
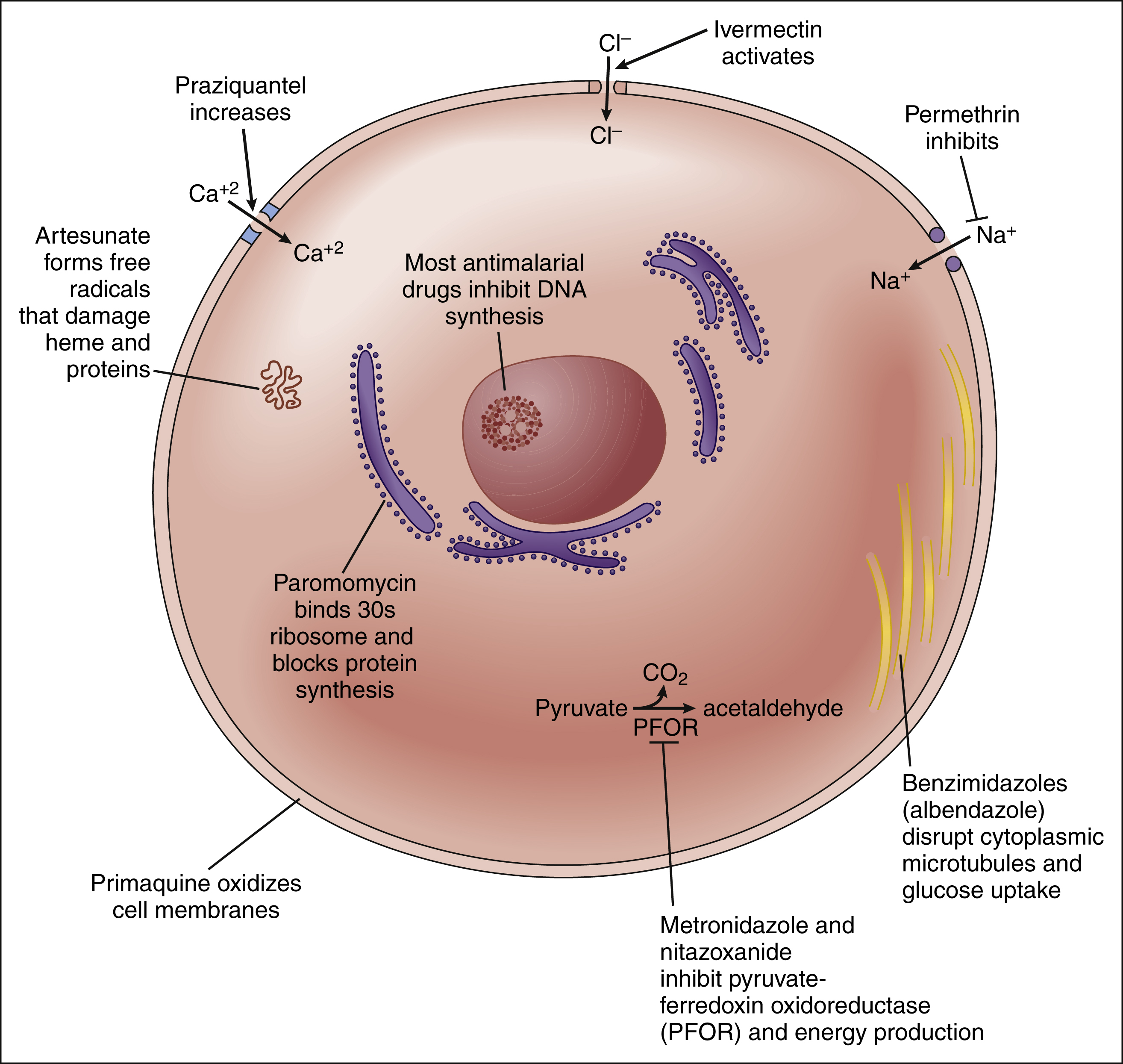
Figure 44–1 Sites of action and mechanisms of antiparasitic drugs. The sites and mechanisms of antiparasitic agents include cell membranes and ion channels, energy metabolism enzymes, cytoplasmic microtubules, DNA synthesis, ribosomal protein synthesis, and free radical damage.
Unlike endoparasitic infections, ectoparasitic infestations are caused by organisms that live on the skin or hair shafts of patients. The most common examples are the lice and mites that cause pediculosis and scabies, respectively.
Table 44–1 provides information about the causes and treatment of numerous protozoan infections, helminthic infections, and ectoparasitic infestations. The antiparasitic agents that are commonly used or represent pharmacologic advances are discussed in this chapter. In some cases, an antibacterial or antifungal agent (e.g., tetracycline or amphotericin B) is listed as either a preferred or alternative drug; these agents are discussed in earlier chapters. A detailed discussion of other agents listed in the table is beyond the scope of this chapter.
DRUGS FOR INFECTIONS CAUSED BY LUMEN- AND TISSUE-DWELLING PROTOZOA
Amebiasis, balantidiasis, cryptosporidiosis, giardiasis, and trichomoniasis are examples of infections caused by protozoan parasites that dwell in the lumen and tissues of their human hosts. Among the agents used to treat these infections are metronidazole, tinidazole, iodoquinol, and paromomycin (see Table 44–1).
Metronidazole
Drug Properties
CHEMISTRY AND PHARMACOKINETICS
Metronidazole is a nitroimidazole compound. It is well absorbed from the gut and is widely distributed to tissues and fluids throughout the body, including the liver and central nervous system (CNS). The drug is extensively metabolized before undergoing renal excretion. Metronidazole is usually administered orally, although an intravenous preparation is available for use in patients with severe infections.
SPECTRUM AND MECHANISMS
Metronidazole is active against several anaerobic protozoa that commonly cause infection. These include Entamoeba histolytica (the agent of amebiasis); Giardia intestinalis (G. lamblia); Trichomonas vaginalis (trichomoniasis); and Balantidium coli (balantidiasis). Metronidazole is also active against anaerobic bacteria, including Bacteroides fragilis, Helicobacter pylori, and Clostridium difficile.
A number of anaerobic organisms express pyruvate-ferredoxin oxidoreductase, an enzyme not found in mammalian cells, which is involved in energy production, carbon recycling, and other metabolic functions. In susceptible anaerobic protozoa, this enzyme transfers electrons to the nitro group of metronidazole to form free nitro-radicals that attack DNA and proteins and thereby produce a cytotoxic effect.
INDICATIONS
Metronidazole, the drug of choice for amebiasis, giardiasis, and trichomoniasis, is also used as an alternative drug in the treatment of balantidiasis.
Patients with amebiasis can suffer from intestinal infection, with or without dysentery, hepatic abscesses, or other extraintestinal manifestations of disease. Metronidazole acts primarily as a tissue amebicide and is usually given in combination with a luminal amebicide (e.g., iodoquinol) to eradicate intestinal amebas.
Giardiasis causes abdominal discomfort and diarrhea in persons infected with the cyst form of Giardia. In the western United States, Giardia cysts are sometimes present in contaminated streams and ponds and are ingested by campers. The administration of metronidazole for 5 days usually cures the infection.
Trichomoniasis is a sexually transmitted disease that produces vaginitis in women but is usually asymptomatic in men. To prevent reinfection, it is important to treat patients and their sexual partners. Treatment can consist either of a single large dose of metronidazole or of smaller doses taken over a 7-day period.
Metronidazole is also used in the management of several disorders that are not caused by protozoa. For example, it is sometimes used in the treatment of patients with dracunculiasis (guinea worm infection). This infection is caused by Dracunculus medinensis, a nematode found in India, Pakistan, and parts of Africa. Although metronidazole is not curative, it reduces inflammation and facilitates manual removal of the worm. Metronidazole is considered the drug of choice for enterocolitis caused by C. difficile, and it is occasionally used to treat infections caused by other anaerobic bacteria. Metronidazole is available in gel or cream form for the topical treatment of rosacea (acne rosacea), a skin condition characterized by persistent erythema of the middle third of the face and other areas of the body.
ADVERSE EFFECTS AND INTERACTIONS
Metronidazole is usually well tolerated, but it causes considerable gastrointestinal discomfort in some persons. Other adverse effects include nausea, vomiting, a metallic taste, and transient leukopenia or thrombocytopenia. To reduce the gastrointestinal side effects, patients should take metronidazole with food.
Metronidazole increases the anticoagulant effect of warfarin, so the dosage of warfarin should be adjusted as necessary. Metronidazole also causes a disulfiram-like reaction with ethanol, so patients should avoid drinking alcohol while they are undergoing treatment.
Metronidazole has been shown to be mutagenic in bacteria and mammalian cell cultures. Although retrospective studies of women who took the drug during pregnancy failed to reveal an increased incidence of birth defects or cancer, it appears prudent to avoid prescribing the drug to women during their first trimester of pregnancy whenever possible.
Tinidazole
Tinidazole is a second-generation nitroimidazole similar to metronidazole but active against metronidazole-resistant strains of Trichomonas vaginalis. As with metronidazole it is indicated for the treatment of trichomoniasis, giardiasis, intestinal amebiasis, and amebic liver abscess. It is also active against Helicobacter pylori and anaerobic bacteria, including Bacteroides fragilis, and it is approved for treating bacterial vaginosis due to Gardnerella vaginalis.
In clinical trials, a single dose of tinidazole cured 93% of patients with giardiasis. In persons with symptomatic intestinal amebiasis, a 3-day course of tinidazole resulted in a cure rate of 86% to 93%, and 2 to 5 days of tinidazole cured 81% to 100% of those with amebic liver abscess. In general, tinidazole produced a higher cure rate in a shorter time period than did metronidazole.
Tinidazole is completely absorbed and widely distributed after oral administration. Its plasma half-life of about 13 hours is considerably longer than that of metronidazole (8 hours). Because it is metabolized by cytochrome P450 3A4, its serum concentrations can be affected by other drugs that inhibit or induce this enzyme. As with metronidazole, tinidazole can cause anorexia, nausea, and vomiting, as well as a bitter taste in the mouth, and it is contraindicated in the first trimester of pregnancy.
Iodoquinol, Paromomycin, Diloxanide, and Nitazoxanide
Iodoquinol, paromomycin, and diloxanide furoate act as luminal amebicides but not tissue amebicides. A luminal amebicide can be used alone to treat asymptomatic carriers of E. histolytica, but it must be used in combination with a tissue amebicide to treat patients with amebic dysentery or liver abscess. The preferred combination is usually tinidazole or metronidazole followed by paromomycin or iodoquinol (see Table 44–1). Iodoquinol can also be used to treat infections with Dientamoeba fragilis, a lumen-dwelling protozoan parasite that causes diarrhea and abdominal pain.
Cryptosporidiosis is a diarrheal illness that may cause chronic diarrhea in immunocompromised persons and has been reported in up to 50% of patients with AIDS. Nitazoxanide is a new drug with broad-spectrum activity against many intestinal protozoa, including Cryptosporidium parvus. The drug is a noncompetitive inhibitor of pyruvate-ferredoxin oxidoreductase and is approved for treatment of cryptosporidiosis and giardiasis in immunocompetent persons. Further studies of nitazoxanide are needed in persons with AIDS. The drug is well tolerated, and a short course of treatment is usually effective. Antidiarrheal medications may also be helpful for these conditions.
DRUGS FOR INFECTIONS CAUSED BY BLOOD- AND TISSUE-DWELLING PROTOZOA
Babesiosis, leishmaniasis, malaria, toxoplasmosis, and trypanosomiasis are examples of infections caused by protozoan parasites that dwell in the blood and tissues of their human hosts.
Drugs for Malaria
Malaria, one of the most common infectious diseases in the world today, is believed to be responsible for more deaths than any other infectious disease. Four species of Plasmodium cause malaria: Plasmodium falciparum, P. malariae, P. ovale, and P. vivax. Most cases of malaria are caused by P. falciparum or P. vivax. The disease is spread via the bites of female Anopheles mosquitoes and is primarily found in tropical and subtropical areas. Malaria has largely been eliminated from industrialized countries in temperate regions, so most infections that are diagnosed in people residing in the United States are infections that were acquired during travel in other countries. Nevertheless, periodic outbreaks of mosquito-borne malaria still occur in the United States.
Malaria is transmitted when infected mosquitoes inject Plasmodium sporozoites into the blood of the human host (Figure 44–2). The sporozoites invade the liver, where they undergo schizogony (asexual multiplication) to form tissue schizonts. The multinucleated schizonts divide their cytoplasm to form thousands of merozoites in a process called exoerythrocytic schizogony. The merozoites are then released from the liver into the blood, where they infect erythrocytes and undergo erythrocytic schizogony. Additional merozoites are subsequently released into the blood by hemolysis.
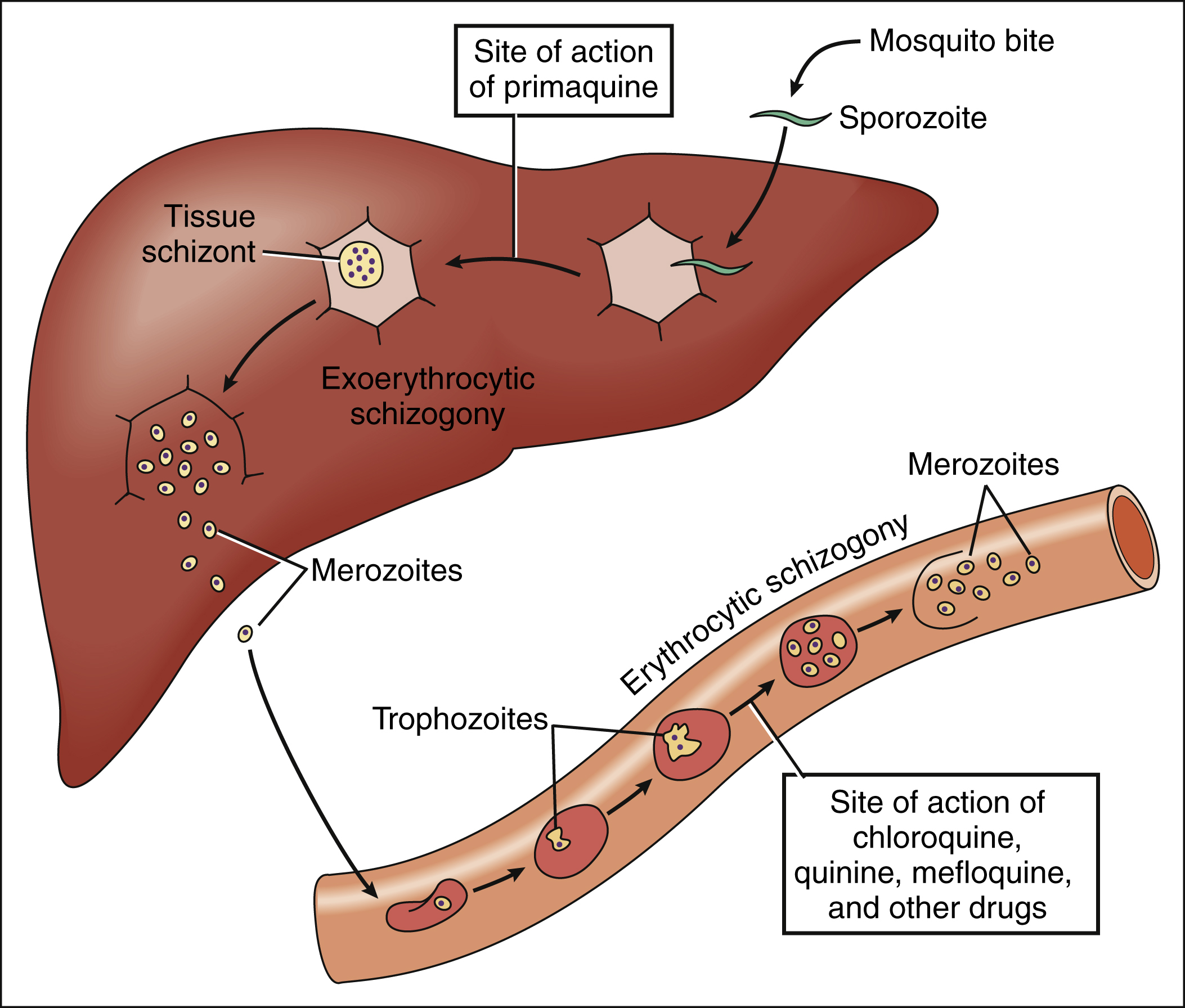
Figure 44–2 Sites of action of drugs for malaria. When a person is bitten by an infected mosquito, Plasmodium sporozoites enter the liver, form tissue schizonts, and undergo exoerythrocytic schizogony to produce merozoites. The merozoites that are released from the liver invade erythrocytes and form trophozoites that undergo erythrocytic schizogony. Some trophozoites develop into male and female gametocytes, which must subsequently pass back into a mosquito before they can develop into sporozoites and repeat the infection cycle. Primaquine blocks exoerythrocytic schizogony, whereas other antimalarial drugs inhibit erythrocytic schizogony.
The synchronous release of merozoites is responsible for the episodic fever observed in patients with malaria. During an infection with P. falciparum or P. vivax, the fever spikes every other day. The disease produced by P. falciparum (malignant tertian malaria) is more severe than that produced by P. vivax (benign tertian malaria), partly because P. falciparum causes a higher level of parasitemia and produces a persistently higher temperature during the periods between fever spikes. Whereas both P. vivax and P. ovale have a persistent exoerythrocytic stage, P. falciparum and P. malariae do not. To eradicate this persistent stage and prevent the relapse of malaria, patients infected with P. vivax or P. ovale can be treated with primaquine.
Sites and Mechanisms of Action
Figure 44–2 shows the sites of action of drugs for malaria. Primaquine inhibits exoerythrocytic (hepatic) schizogony. In contrast, all of the other antimalarial agents inhibit erythrocytic schizogony.
The mode of action of primaquine is unclear, but the drug appears to act by forming quinoline-quinone intermediates that oxidize schizont membranes. These oxidizing intermediates may also be responsible for the hemolytic effect of the drug.
Chloroquine, mefloquine, and quinine are believed to inhibit nucleic acid synthesis or function during erythrocytic schizogony, although the exact mechanisms of action are unclear. Chloroquine may block the synthesis of nucleic acid, and it may also impair the ability of plasmodia to utilize hemoglobin. The selective toxicity of chloroquine can be partly explained by the drug’s greater accumulation in infected erythrocytes than in uninfected cells. Quinine appears to form a complex with plasmodial DNA, thereby preventing replication and transcription.
Sulfadoxine is a sulfonamide that acts synergistically with pyrimethamine to inhibit the synthesis of folic acid in plasmodia and thereby prevent the synthesis of nucleic acid. The sulfonamides inhibit dihydrofolate formation, whereas pyrimethamine prevents dihydrofolate reduction.
Other drugs used in the treatment of malaria include artesunate, atovaquone, and proguanil. Proguanil acts by inhibiting folate reductase, and artesunate forms free radicals that damage heme and proteins.
Chloroquine, Quinine, and Quinidine
Quinine, a drug that had been used for centuries to treat malaria, was supplanted by chloroquine after World War II. Until the 1980s, when resistance to chloroquine became widespread, chloroquine remained the drug of choice. Now that drug resistance has severely curtailed the effectiveness of chloroquine, quinine is once again being used to treat malaria in many regions of the world. In addition, other drugs have been introduced.
The only areas where most P. falciparum organisms are sensitive to chloroquine are the Caribbean islands, the part of Central America that is west of the Panama Canal, and parts of North and West Africa and the Middle East. In these chloroquine-sensitive areas, chloroquine is still the drug of choice for both the prevention and the treatment of all types of malaria, although it must be used in combination with primaquine (see “Primaquine”) to eradicate vivax or ovale malaria.
The most common adverse effects of chloroquine are gastrointestinal distress, nausea, and vomiting. Toxic doses can cause retinal damage and even blindness. In pregnant women, chloroquine should be used cautiously because fetal damage has been reported.
Patients with chloroquine-resistant malaria are usually treated with a combination of quinine sulfate plus either doxycycline or pyrimethamine-sulfadoxine. Alternatives include atovaquone-proguanil and artesunate plus mefloquine.
Mefloquine
Mefloquine is a newer antimalarial drug that has been used for both the prevention and the treatment of chloroquine-resistant malaria. Because cure rates with chloroquine have dropped from almost 100% in the 1980s to 40% by 1995, mefloquine is now primarily used to prevent malaria in areas where chloroquine-resistant strains are prevalent. The drug is given orally, undergoes hepatic metabolism, has a half-life of about 14 days, and is eliminated via the bile and feces.
Mefloquine can cause a severe neuropsychiatric syndrome characterized by hallucinations, anxiety, confusion, seizures, and coma. It can also cause leukopenia and thrombocytopenia.
For patients who cannot tolerate mefloquine, doxycycline (see Chapter 39) can be used to prevent malaria in areas where chloroquine-resistant organisms are prevalent.
Primaquine
Primaquine is an 8-aminoquinoline derivative that is active against the exoerythrocytic stage of P. vivax and P. ovale. By eradicating tissue plasmodia, it prevents the reemergence of organisms from the liver and relapse of the infection. Primaquine must be used in combination with other drugs to treat infection with P. vivax or P. ovale, because primaquine is not active against the erythrocytic stage of these organisms.
Primaquine is converted to oxidizing quinoline-quinone intermediates in the body. These intermediates are believed to be responsible for the antimalarial effects and some of the toxic effects of the drug. In individuals who have hereditary glucose-6-phosphate dehydrogenase (G6PD) deficiency, the intermediates may oxidize erythrocyte membranes and thereby cause red cell hemolysis and hemolytic anemia. This anemia occurs because G6PD is unable to generate sufficient quantities of reduced nicotinamide adenine dinucleotide phosphate to maintain glutathione in its reduced form and thereby prevent oxidation of erythrocyte membranes. Individuals who experience this type of hemolytic anemia are said to have primaquine sensitivity. A number of other drugs with oxidizing properties, including sulfonamides and sulfones, can also cause this reaction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


