Figure 21–1 Structures of selected local anesthetics.
Local anesthetics are formulated as hydrochloride salts with a pH less than 7, as the ionized molecule is more soluble and stable than the free base. Once injected, the local anesthetic solution is quickly buffered to the pH of the tissue.
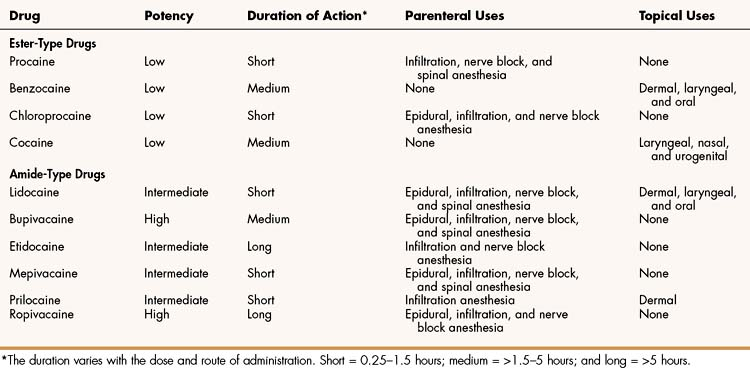
The duration of action of local anesthetics can be short, medium, or long (Table 21–1). Because local anesthetics act directly at the site of administration, their duration of action is determined primarily by the rate of diffusion and absorption away from the site of administration. Diffusion and absorption, in turn, depend on the chemical properties of the anesthetics and on such factors as local pH and blood flow. In some formulations, epinephrine is added to prolong a local anesthetic’s duration of action by producing vasoconstriction and slowing its rate of absorption. Because of the risk of ischemia and necrosis, however, local anesthetics with epinephrine are not used to anesthetize tissues with end arteries, such as tissues of the fingers, toes, ears, nose, and penis.
Following systemic absorption, ester-type local anesthetics are metabolized in the plasma by butyrylcholinesterases to p-aminobenzoic acid (PABA) derivatives. Amide-type local anesthetics undergo metabolism by hepatic P450 enzymes to yield polar metabolites. In both cases, the metabolites are excreted in the urine.
Mechanism of Action
Local anesthetics cause a reversible inhibition of action potential conduction by binding to the sodium channel and decreasing the nerve membrane permeability to sodium. The nonpolar, lipophilic form of the anesthetic molecule passes through the neuronal membrane and switches to the polar, hydrophilic form in the cytoplasm of the neuron. This cationic form of the anesthetic binds to the cytoplasmic side of the sodium channel protein and prolongs the inactivation state of the sodium channel (Fig. 21–2). With sodium channels blocked, action potentials cannot propagate along the neuronal fiber and sensory input is lost.
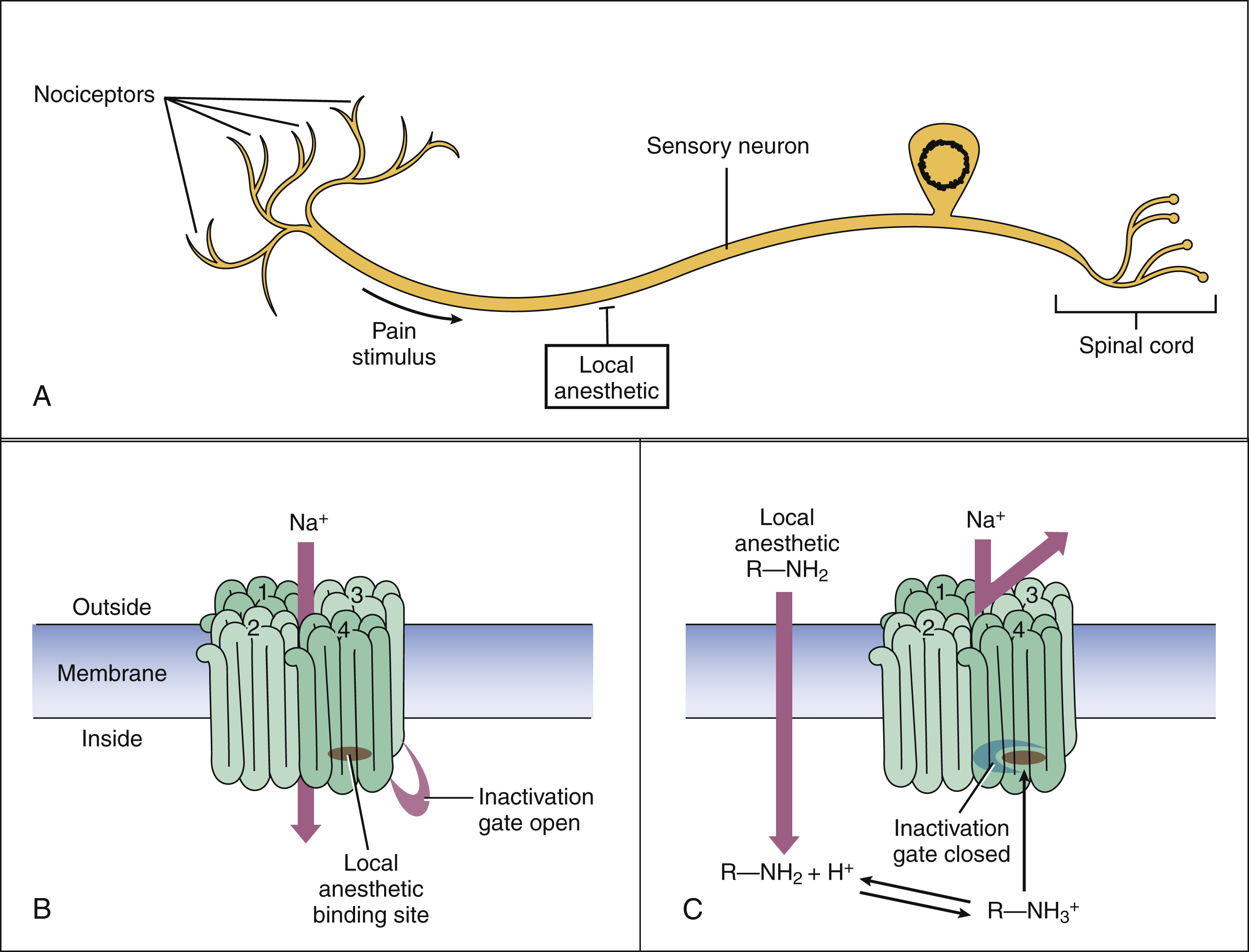
Figure 21–2 Mechanisms of action of local anesthetics. (A) The local anesthetic binds to sodium channels and blocks the generation and conduction of action potentials in peripheral neurons. (B) The sodium channel includes four large transmembrane domains, each with six transmembrane spanning regions. The inactivation gate is a short, intracellular loop between domains 3 and 4. The local anesthetic binds to amino acid residues located on domain 4. (C) The non-ionized form of the local anesthetic (R—NH2) penetrates the axonal membrane and is then converted to the ionized form (R—NH3+). The ionized form binds to the sodium channel in the open state, and this prolongs the sodium channel inactivation state. Sodium entry is blocked during the inactivation state.
Pharmacologic Effects
Local anesthetics have a greater affinity for sodium channels that are in the depolarized (open) configuration than for channels that are closed. Nerve fibers that are firing, therefore, are more susceptible to sodium channel blockade. This use-dependent blockade causes a selective inhibition of nerve fibers that are stimulated by the surgical procedure, such as pain fibers during suturing. Size-dependent blockade refers to the finding that small diameter fibers are blocked more easily than are larger fibers. Small unmyelinated C and lightly myelinated Aδ pain fibers, therefore, are more easily anesthetized than are large myelinated touch fibers. Autonomic and sensory nerves are blocked more easily than are motor nerves. Nerves recover from blockade in the reverse order.
Adverse Effects and Interactions
The adverse effects of local anesthetics are primarily caused by their absorption into the systemic circulation and subsequent alteration of central nervous system (CNS), cardiovascular, and other organ system functions.
Local anesthetics often produce CNS stimulation (restlessness, tremor, and euphoria) followed by inhibition (drowsiness and sedation). Other symptoms of local anesthetic toxicity include headache, paresthesias, and nausea. Higher concentrations can cause seizures followed by coma. Death is usually caused by respiratory failure.
Adverse cardiovascular effects include hypotension and cardiac depression. Most local anesthetics are vasodilators, and they also block vasoconstriction induced by the sympathetic nervous system. Most local anesthetics have antiarrhythmic activity, but toxic levels of local anesthetics suppress cardiac conduction and can cause tachyarrhythmia characterized by a wide QRS complex.
Local anesthetic blockade of autonomic ganglia and neuromuscular transmission can lead to loss of visceral and skeletal muscle tone. For this reason, local anesthetics potentiate the effect of neuromuscular blocking drugs (e.g., tubocurarine) and must be used with great caution in patients with myasthenia gravis.
Allergic reactions to local anesthetics are fairly common. Patients who have repeated applications of topical anesthetics are particularly susceptible to sensitization. The ester-type anesthetics cause hypersensitivity reactions more frequently than do the amide-type anesthetics. This is because ester-type anesthetics (e.g., procaine) are metabolized to PABA. PABA causes allergic reactions in a small percentage of individuals. Patients who are allergic to an ester-type anesthetic will usually tolerate an amide-type anesthetic.
Indications
Local anesthetics are usually administered parenterally but are sometimes applied topically. The route of administration depends on factors such as the site of anesthesia.
TOPICAL ANESTHESIA
The topical application of local anesthetics is used to anesthetize the skin, mucous membranes, or cornea. A local anesthetic can be applied to the skin to treat pruritus (itching) caused by poison ivy, insect bites, eczema, or cutaneous manifestations of systemic diseases such as chickenpox (varicella). A eutectic mixture of local anesthetics (EMLA), consisting of two or more solid compounds that form a liquid when they are combined, is sometimes used to anesthetize the skin before venipuncture or minor surgery. The topical application of a local anesthetic to mucous membranes can relieve pain caused by oral, nasal, laryngeal, rectal disorders, or surgery. For example, an anesthetic ointment is used to relieve the discomfort of hemorrhoids. The topical ocular administration of local anesthetics is used to anesthetize the cornea before diagnostic or surgical procedures (e.g., radial keratotomy), the removal of foreign bodies, and cataract surgery.
INFILTRATION ANESTHESIA
Infiltration is probably the most common route used to administer local anesthetics. The process involves injecting an anesthetic directly into subcutaneous tissue just under the skin. Infiltration is used primarily for minor surgical procedures (e.g., suturing a wound) or for the removal of foreign bodies. It is also frequently used for dental procedures. When a local anesthetic is to be administered by infiltration, epinephrine can be added to it to decrease its dosage and prolong its duration of action. As mentioned earlier, however, epinephrine should not be used to anesthetize fingers, toes, and other tissues with end arteries.
IONTOPHORESIS
Local anesthetics can also be administered by iontophoresis. This technique uses a small electric current to force molecules of the anesthetic into the tissue. Iontophoresis is used primarily in dentistry. It eliminates the need to inject the anesthetic and is used by some dentists for this reason. A new, needle-free device with the trade name of Zingo delivers powdered lidocaine by rapid gas pressure to reduce the pain of subsequent peripheral injections or blood draws. It is approved for use in children.
NERVE BLOCK AND FIELD BLOCK ANESTHESIA
Nerve block and field block anesthesia are forms of regional anesthesia, the goal of which is to anesthetize an area of the body by blocking the conductivity of sensory nerves from that area. In nerve block anesthesia, a local anesthetic is injected into or adjacent to a peripheral nerve or nerve plexus. For example, a radial nerve block can be used to anesthetize the structures innervated by the radial nerve, including portions of the forearm and hand. Intraorbital block is often used for ocular surgery. Other examples of nerve block anesthesia are brachial plexus and cervical plexus blocks. In field block anesthesia, a local anesthetic is administered in a series of injections to form a wall of anesthesia encircling the operative field.
SPINAL INTRATHECAL ANESTHESIA
Spinal anesthesia is used to block somatic sensory and motor fibers during procedures such as surgery on the lower limb or pelvic structures. A local anesthetic is injected into the subarachnoid, intrathecal space below the level at which the spinal cord terminates. The spread of the anesthetic along the neuraxis is controlled by the horizontal tilt of the patient and by the specific gravity (baricity) of the local anesthetic solution. Hyperbaric solutions of local anesthetics are available for this purpose, and these spread along the neuraxis for about 15 minutes. By this time, they have mixed with cerebrospinal fluid to become isobaric and are said to be “fixed” at a certain level of the spinal cord. Spinal anesthesia can cause headaches associated with cerebrospinal fluid leakage from the lumbar puncture, and respiratory depression can occur if the anesthetic ascends too high up the spinal cord. Entry into the CNS by spinal injection also carries a small risk of infection or meningitis.
EPIDURAL ANESTHESIA
Epidural anesthesia is produced by injecting a local anesthetic into the lumbar or caudal epidural (extradural) space. A local anesthetic, such as bupivacaine, is often administered by this route to provide anesthesia during labor and delivery. After epidural administration, the local anesthetic is absorbed into the systemic circulation. Therefore, doses must be carefully monitored to prevent cardiac depression and neurotoxicity in the mother and neonate.
SPECIFIC AGENTS
Ester-Type Local Anesthetics
Cocaine, a naturally occurring plant alkaloid, was the first local anesthetic to be discovered. It has both local anesthetic and CNS stimulant properties, and it is the only local anesthetic that causes significant vasoconstriction as a result of its sympathomimetic effect. Because of its CNS effects and potential for abuse (see Chapter 25), cocaine is seldom used as a local anesthetic. It is occasionally used, however, to anesthetize the internal structures of the nose, where its vasoconstrictive action helps prevent bleeding after nasal surgery. A cocaine solution is applied to gauze and inserted into the nose for this purpose.
Procaine, the first synthetic local anesthetic drug to be prepared after the discovery of cocaine, became the standard of comparison for many years. Procaine and chloroprocaine have a low potency and a relatively short duration of action. They are not effective after topical administration and must be administered parenterally. Both drugs are metabolized to PABA. For this reason, they are more likely to cause allergic reactions than are the amide-type local anesthetics. Tetracaine is another ester-type local anesthetic with a longer duration of action than procaine. It is used for infiltration anesthesia. It is also available in a topical spray and gel formulation in combination with butamben (butyl aminobenzoate) and benzocaine in a preparation called Cetacaine.
Benzocaine, a frequently used topical anesthetic, is available in a number of nonprescription products for the treatment of sunburn, pruritus, and other skin conditions. In some patients, the drug causes hypersensitivity reactions, which can exacerbate preexisting dermatitis. Benzocaine is also used to anesthetize mucous membranes and is available in cough lozenges and sprays to relieve coughing.
Proparacaine is available in a 0.5% solution for instillation during eye surgery and other ophthalmic procedures. Dibucaine is formulated in an ointment used to relieve the pain and itching of hemorrhoids (piles) and other problems in the rectal area.
Amide-Type Local Anesthetics
Lidocaine produces local anesthesia after topical or parenteral administration. The most widely used local anesthetic, it is available in a number of formulations. These include topical solutions and ointments, oral sprays, viscous gels for oral and laryngeal application, and various parenteral formulations. A eutectic mixture of lidocaine and prilocaine is available as a cream to anesthetize intact skin to a depth of 5 mm. In pediatric patients, EMLA cream has been used for local anesthesia before venipuncture, intravenous cannulation, or circumcision. Lidocaine is also used for infiltration, nerve block, epidural, and spinal anesthesia.
Etidocaine has properties similar to those of lidocaine, but its duration of action is considerably longer. It is primarily used for infiltration and nerve block anesthesia.
Bupivacaine, mepivacaine, and ropivacaine have similar clinical uses but differ in their duration of action, as shown in Table 21–1. Bupivacaine has been the most widely used local anesthetic for obstetrical anesthesia, but it causes cardiac depression more frequently than do many other local anesthetics. Ropivacaine is a newer drug that may cause fewer cases of cardiac toxicity. Levobupivacaine is the isolated S(-)-stereoisomer of racemic bupivacaine, which is the active form of the chiral drug mixture. It is used in epidural anesthesia for labor and delivery.
Prilocaine is a congener of lidocaine. It is converted to O-toluidine, a toxic metabolite that can cause methemoglobinemia if it is allowed to accumulate. For this reason, prilocaine use is limited to topical and infiltration anesthesia.
GENERAL ANESTHETICS
The first demonstration of general anesthesia for surgery was performed by William Morton at Massachusetts General Hospital in 1846. The anesthetic that Morton used was diethyl ether, and his demonstration had a profound impact on the field of surgery. Before that time, surgery was limited to rapid procedures such as limb amputations. General anesthesia and the subsequent development of aseptic techniques permitted the evolution of surgical procedures to the sophisticated level achieved today.
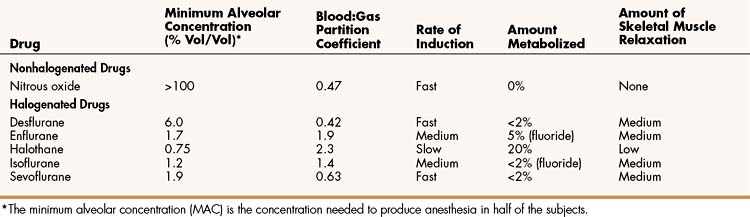
Diethyl ether is no longer used in developed countries, because it has a slow rate of induction, causes considerable postoperative nausea and vomiting, and is highly flammable. Use of another anesthetic gas, cyclopropane, has also been abandoned, because of its explosive nature and its tendency to cause cardiac arrhythmias. A variety of anesthetics are currently available for inhalational use, however. These include nitrous oxide and a growing number of halogenated hydrocarbons. The pharmacologic properties and adverse effects of these drugs are listed in Tables 21–2 and 21–3, respectively.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree