Autacoids regulate certain aspects of gastrointestinal, uterine, and renal function, and they are involved in pain, fever, inflammation, allergic reactions, asthma, thromboembolic disorders, and other pathologic conditions. Drugs that inhibit autacoid synthesis or block autacoid receptors are helpful in treating these conditions, whereas drugs that activate autacoid receptors are useful for inducing labor, alleviating migraine headaches, counteracting drug-induced peptic ulcers, and other purposes.
Autacoids include monoamines, such as histamine and serotonin, as well as fatty acid derivatives, including prostaglandins and leukotrienes. Autacoids activate specific membrane receptors in target tissues, mostly of the G protein–coupled receptor type. Their effects are usually restricted to the tissue in which they are formed, but under pathologic conditions, extraordinarily large amounts of autacoids can be released into the systemic circulation. These disorders include carcinoid tumor and anaphylactic shock, which cause the release of copious amounts of serotonin and histamine, respectively, and exert systemic effects including CNS effects. Most autacoids are rapidly metabolized to inactive compounds, as seen with prostaglandins, and some autacoids undergo tissue reuptake, as evidenced by 5-hydroxytryptamine (5-HT) reuptake transporter proteins in neurons and peripheral cells.
This chapter provides basic information about autacoids and reviews the many types of drugs that influence their effects. Some autacoid drugs are covered completely here, whereas other chapters provide more details on other agents.
HISTAMINE AND RELATED DRUGS
Histamine Biosynthesis and Release
Histamine is a biogenic amine produced primarily by mast cells and basophils, which are particularly abundant in the skin, gastrointestinal tract, and respiratory tract. Histamine is also produced by paracrine cells in the gastric fundus, where it stimulates acid secretion by parietal cells. Histamine also functions as a neurotransmitter in the CNS (see Chapter 18).
Histamine is formed when the amino acid histidine is decarboxylated in a reaction catalyzed by the enzyme, l-histidine decarboxylase. Histamine is stored in granules (vesicles) in mast cells and basophils until it is released. It is released from mast cells when membrane-bound immunoglobulin E (IgE) interacts with an IgE antigen to cause mast cell degranulation. This process can be blocked by cromolyn sodium and related respiratory drugs, as described in Chapter 27. A number of other stimuli can also cause the release of histamine from mast cells (Fig. 26–1). Stimuli that increase cyclic guanosine monophosphate increase histamine release, whereas those that increase cyclic adenosine monophosphate oppose this action.
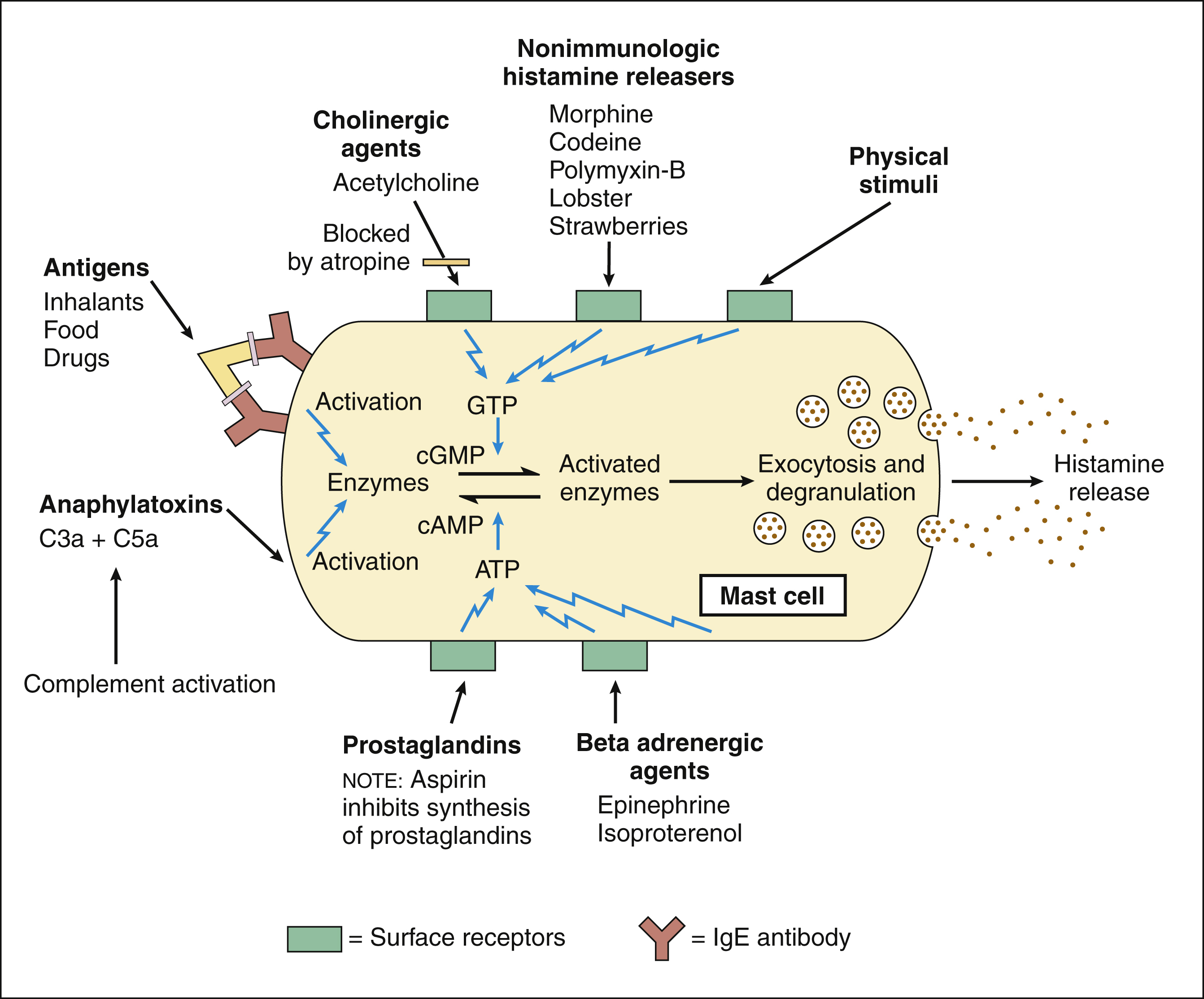
Figure 26–1 Release of histamine from mast cells. Numerous chemical and physical stimuli activate histamine release from mast cells. Complement activation from serum sickness or bacterial endotoxins produces the anaphylactic peptides C3a and C5a, allergic antigens bind to IgE antibodies, and chemicals and other substances increase guanosine triphosphate (GTP) and cyclic guanosine monophosphate (cGMP) to activate enzymes causing increased intracellular calcium and release of histamine granules. β-Adrenoceptor agents and some prostaglandins increase adenosine triphosphate (ATP) and cyclic adenosine monophosphate (cAMP) and reduce activated enzymes.
Mast cell degranulation can also be triggered by bacterial toxins and by drugs such as morphine and tubocurarine. Some of these stimuli result in the formation of inositol triphosphate (IP3) and diacylglycerol (DAG). As with neurons, this causes the release of intracellular calcium and the fusion of granule membranes with the plasma membrane, thereby releasing histamine and other compounds. The release of histamine that can occur with morphine administration does not appear to be mediated by opioid receptors because the opioid antagonist, naloxone, does not inhibit morphine-induced histamine release from mast cells.
Histamine is inactivated by methylation and oxidation reactions that are catalyzed by a methyltransferase enzyme and diamine oxidase, respectively.
Histamine Receptors and Effects
Histamine receptors have been classified as H1, H2, and H3. All three types are typical, seven-transmembrane G protein–coupled receptor proteins.
H1 receptors are involved in allergic reactions that cause dermatitis, rhinitis, conjunctivitis, and other forms of allergy. Activation of H1 receptors in the skin and mucous membranes causes vasodilation; increases vascular permeability; and leads to erythema (heat and redness), congestion, edema, and inflammation. Stimulation of H1 receptors on mucocutaneous nerve endings can cause pruritus (itching), and in the lungs, it initiates the cough reflex. If sufficient histamine is released into the circulation, total peripheral resistance and blood pressure fall and the individual may progress to anaphylactic shock. Activation of H1 receptors also causes bronchoconstriction and contraction of most gastrointestinal smooth muscles.
H2 receptors are most noted for increasing gastric acid secretion, but they are also involved in allergic reactions. For this reason, H2 receptor antagonists are sometimes used in combination with H1 receptor antagonists in the treatment of allergies. Activation of H2 receptors in the heart increases the heart rate and contractility, but the cardiac effects of histamine are not prominent under most conditions.
H3 receptors are located in various tissues in the periphery and on nerve terminals. Activation of these presynaptic receptors in the brain inhibits the release of histamine and other neurotransmitters.
ANTIHISTAMINE DRUGS
Antihistamines, or histamine receptor antagonists, have been categorized on the basis of their receptor selectivity as H1 receptor antagonists or H2 receptor antagonists.
Histamine H1 Receptor Antagonists
Classification
The following discussion focuses on the properties and uses of four groups of H1 receptor antagonists. Chlorpheniramine, clemastine, dimenhydrinate, diphenhydramine, hydroxyzine, meclizine, and promethazine are examples of first-generation drugs. Cetirizine, fexofenadine, loratadine, and desloratadine are examples of second-generation drugs. Drugs in these two groups are administered orally or parenterally. A major difference in the two groups is that the first-generation antihistamines are distributed to the CNS and can cause sedation, whereas the second-generation antihistamines do not cross the blood-brain barrier significantly. Azelastine is an example of an intranasal antihistamine, and levocabastine, ketotifen, epinastine, and olopatadine are used for ophthalmic treatment.
MECHANISMS AND PHARMACOKINETICS
The H1 antihistamines contain an alkylamine group that resembles the side chain of histamine and permits them to bind to the H1 receptor and act as competitive receptor antagonists. The drugs can block most of the effects of histamine on vascular smooth muscles and nerves and thereby prevent or counteract allergic reactions.
When antihistamines are administered orally, they are rapidly absorbed and are widely distributed to tissues. Many of them are extensively metabolized in the liver by cytochrome P450 enzymes. Hydroxyzine has an active metabolite that is also available as the drug, cetirizine, and this drug is excreted unchanged in the urine and feces.
Azelastine is an H1 antihistamine that is marketed as a nasal spray for the treatment of allergic rhinitis. It blocks H1 receptors and inhibits the release of histamine from mast cells, and it is much more potent than either sodium cromoglycate or theophylline in its inhibition. The systemic bioavailability of azelastine following intranasal administration is about 40%, and the plasma half-life is about 22 hours. Azelastine is metabolized by cytochrome P450 enzymes to an active metabolite, desmethylazelastine, a substance whose plasma concentrations are 20% to 30% of azelastine concentrations. Azelastine and its principal metabolite are both H1 receptor antagonists. The unchanged drug and its active metabolite are excreted primarily in the feces.
PHARMACOLOGIC EFFECTS AND INDICATIONS
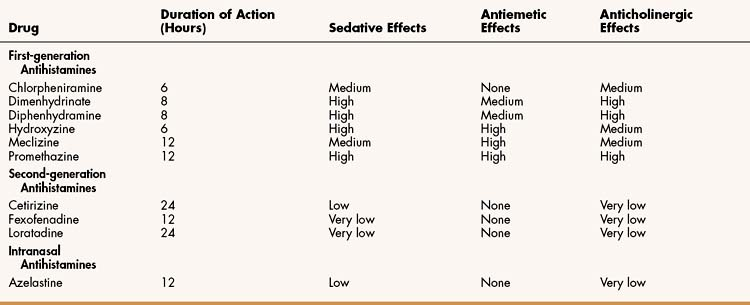
The H1 antihistamines are all equally effective in treating allergies, but they differ markedly in their sedative, antiemetic, and anticholinergic properties (Table 26–2). The second-generation antihistamines cause little or no sedation, so they are often preferred for the treatment of allergies. Antihistamines are usually more effective when administered before exposure to an allergen than afterward. Hence, persons with seasonal allergies, such as allergic rhinitis (see Chapter 27), should take them on a regular basis throughout the allergy season.
First-Generation Antihistamines
Because the first-generation antihistamines have sedative effects, they are occasionally used to produce sedation. They are also used to treat nausea and vomiting, to prevent motion sickness in persons traveling by plane or boat, or to treat vertigo (an illusory sense that the environment or one’s own body is revolving).
The most sedating drugs are diphenhydramine, hydroxyzine, and promethazine. These drugs have been used to induce sleep or for preoperative sedation. Their sedating properties can also be useful in relieving distress caused by the severe pruritus associated with some allergic reactions. Persons taking these drugs should be cautioned against driving or operating machinery.
Pheniramine drugs (e.g., chlorpheniramine), are less sedating than other first-generation drugs and are used primarily in the treatment of allergic reactions to pollen, mold spores, and other environmental allergens.
Meclizine, diphenhydramine, hydroxyzine, and promethazine have higher antiemetic activity than other antihistamines. Meclizine is less sedating than diphenhydramine, hydroxyzine, and promethazine, so it is frequently used to prevent motion sickness or treat vertigo. Dimenhydrinate is a mixture of diphenhydramine and 8-chlorotheophylline and is also used for these purposes. Promethazine suppositories are often used to relieve nausea and vomiting associated with various conditions (see Chapter 28).
Second-Generation Antihistamines
The second-generation drugs lack antiemetic activity, so their use is limited to the treatment of allergies. None of these drugs causes substantial sedation; however, cetirizine is more likely than astemizole, fexofenadine, or loratadine to cause some sedation. Because fexofenadine has a shorter half-life, it must be taken twice a day, whereas the other second-generation drugs are taken once a day. Fexofenadine and cetirizine are eliminated primarily as the unchanged drug in the feces and urine, respectively. Loratadine and desloratadine are metabolized to active metabolites, which are excreted in the urine and feces.
Intranasal Antihistamines
Azelastine is indicated for the treatment of symptoms of allergic rhinitis, including sneezing, nasal itching, and nasal discharge. It is administered as two sprays per nostril twice daily. The drug can cause drowsiness so should be used cautiously when patients are driving or operating machinery.
Opthalmic Antihistamines
Currently, four antihistamine eyedrop formulations are available. Levocabastine, epinastine, and olopatadine are selective H1 antagonists for topical ophthalmic use. They are indicated for the temporary relief of the signs and symptoms of seasonal allergic conjunctivitis. Ketotifen is a selective, noncompetitive H1 antagonist and mast cell stabilizer. The action of ketotifen occurs rapidly with an effect seen within minutes after administration and, because of the noncompetitive nature of the receptor antagonism, it has a longer duration of action than the other agents. It is indicated for the temporary prevention of itching of the eye caused by allergic conjunctivitis.
FIRST-GENERATION ANTIHISTAMINES
Sedation is the most common side effect of the first-generation antihistamines. Paradoxically, however, the drugs can produce excitement in infants and children and should be used with caution in these patients.
Diphenhydramine and promethazine have the highest anticholinergic activity (see Table 26–2), but other first-generation drugs also block cholinergic muscarinic receptors. As a result, the drugs can cause dry mouth, blurred vision, tachycardia, urinary retention, and other atropine-like side effects.
Anticholinergic toxicity is the principal manifestation of an overdose of first-generation antihistamines. Administration of physostigmine, a cholinesterase inhibitor that crosses the blood-brain barrier, may be required to counteract the anticholinergic effects of antihistamines in the CNS.
SECOND-GENERATION ANTIHISTAMINES
Astemizole (Hismanal) also caused prolongation of the QT interval and was removed from the market. Fexofenadine, is the active metabolite of terfenadine (Seldane). Terfenadine was the first nonsedating H1 blocker, but was withdrawn from the market by the U.S. Food and Drug Administration because it prolonged the QT interval on the electrocardiogram, leading to a type of cardiac arrhythmia called torsades de pointes. Fexofenadine does not appear to cause cardiac abnormalities. Cetirizine and loratadine also lack cardiac effects (Box 26–1).
BOX 26–1 THE CASE OF THE SNEEZING STOCKBROKER
CASE PRESENTATION
A 35-year-old male working as a stockbroker complains to his physician that he is constantly sneezing and has a runny nose and itchy, watery eyes whenever he is at his home in the country. He tells his physician that he tried an over-the-counter allergy medicine but that it made him drowsy and feel “like he was living in a fog.” His doctor tells him that he suffers from allergic rhinitis, or “hay fever,” and prescribes a nasal spray containing azelastine.
CASE DISCUSSION
The most common symptom of seasonal allergies is allergic rhinitis, otherwise known as hay fever. Symptoms of allergic rhinitis closely mimic those of the common cold, but with a cold, nasal discharge may be thick and yellow. With allergies, it is generally thin and clear. An allergy is also often accompanied by itchy, watery eyes. Most over-the-counter medications include diphenhydramine, a first-generation antihistamine, but these preparations are known to cause drowsiness. The newer, second-generation antihistamines are fexofenadine and loratadine, which do not cause drowsiness, as they do not readily gain access into the CNS. Among the different types of nose sprays, there is azelastine, an antihistamine, and those that contain steroids, such as beclomethasone, fluticasone, or triamcinolone. The drawback to steroid medications is that they may take a week or so to be maximally effective. There is also a nasal spray containing cromolyn sodium, a mast cell stabilizer, available without a prescription.
INTRANASAL ANTIHISTAMINES
Adverse effects of azelastine are rare and include dizziness, fatigue, headache, nasal irritation, dry mouth, and weight gain.
Histamine H2 and H3 Receptor Antagonists
Chapter 28 outlines the properties of H2 receptor antagonists, which are used primarily to treat peptic ulcer disease. There are presently no approved H3 receptor agents, although clinical trials are under way (see Selected Readings).
SEROTONIN AND RELATED DRUGS
Serotonin Biosynthesis and Release
Serotonin, or 5-hydroxytryptamine (5-HT), is an autacoid and a neurotransmitter that is produced primarily by platelets, enterochromaffin cells in the gut, and neurons. The greatest concentration of serotonin is in the enterochromaffin cells of the gastrointestinal tract. As illustrated in Figure 18–3C, serotonin is synthesized from the amino acid tryptophan and is converted to 5-hydroxyindoleacetic acid (5-HIAA) by monoamine oxidase and aldehyde dehydrogenase. 5-HIAA is then excreted in the urine. Serotonin is concentrated in vesicles within the cell and released by calcium-mediated exocytosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree