Figure 16–1 Normal hemostasis. (1) When a small blood vessel is injured, vasospasm reduces blood flow and facilitates platelet aggregation and coagulation. (2) The platelets, which adhere to extravascular collagen, are activated to release mediators that cause platelet aggregation and the formation of a platelet plug to arrest bleeding. (3) Exposure of the blood to tissue factors also activates coagulation and leads to the formation of a fibrin clot, which arrests bleeding until the vessel is repaired. (4) After the vessel is repaired, the clot is removed by the process of fibrinolysis.
Vasospasm reduces bleeding and blood flow and thereby facilitates platelet adhesion and coagulation. Exposure of the blood to extravascular collagen causes adherence of platelets to the injured vessel wall and initiates the sequential activation of numerous coagulation factors, or blood clotting factors. These factors and their synonyms are listed in Table 16–1, and the coagulation pathways are illustrated in Figure 16–2. The intrinsic pathway may be activated by surface contact with a foreign body or extravascular tissue, whereas the extrinsic pathway is activated by a complex tissue factor. The pathways converge with the activation of factor X, which is the major rate-limiting step in the coagulation cascade. The activation of factor X leads to the formation of thrombin, and thrombin, in turn, catalyzes the conversion of fibrinogen to fibrin. The fibrin meshwork traps erythrocytes and platelets to complete the formation of a hemostatic thrombus (clot).
TABLE 16–1 Coagulation Factors
| Factor∗ | Common Synonym | Dependent on Vitamin K† |
|---|---|---|
| I | Fibrinogen | No |
| II | Prothrombin | Yes |
| III | Tissue thromboplastin | No |
| IV | Calcium | No |
| V | Proaccelerin | No |
| VII | Proconvertin | Yes |
| VIII | Antihemophilic factor | No |
| IX | Plasma thromboplastin component | Yes |
| X | Stuart factor | Yes |
| XI | Plasma thromboplastin antecedent | No |
| XII | Hageman factor | No |
| XIII | Fibrin stabilizing factor | No |
∗ Factor VI is no longer considered to be a coagulation factor.
† Proteins C and S, which are endogenous anticoagulants that inactivate factors Va and VIIIa and promote fibrinolysis, are also dependent on vitamin K.
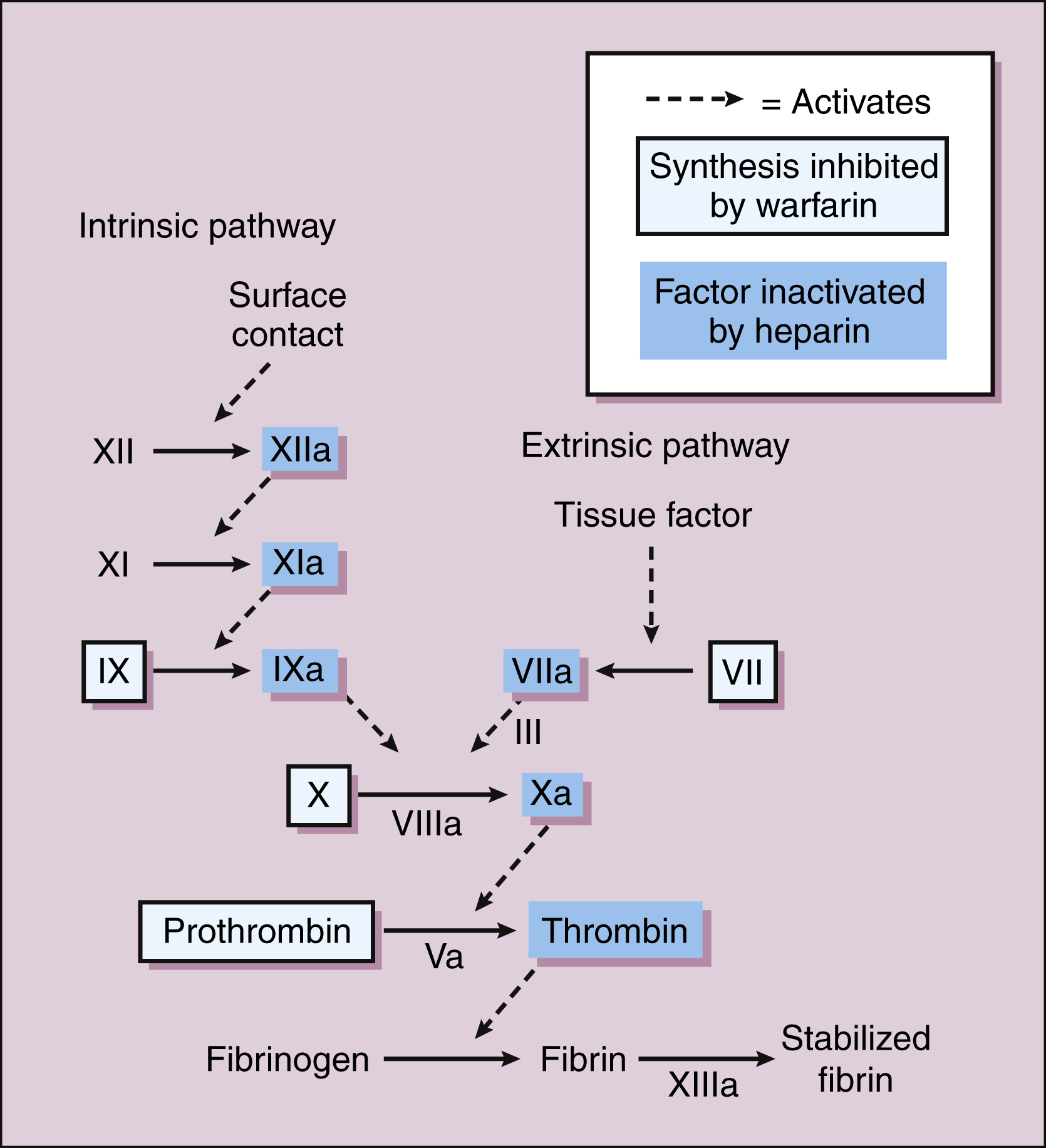
Figure 16–2 Blood coagulation and sites of drug action. Blood coagulation involves the sequential activation of proteolytic clotting factors. The intrinsic pathway can be activated by surface contact with a foreign body, whereas the extrinsic pathway is activated by tissue factor. The pathways converge with the activation of factor X, which leads to the formation of thrombin and fibrin. Warfarin and other oral anticoagulants inhibit the synthesis of the vitamin K–dependent clotting factors. Heparin inactivates various clotting factors.
Pathologic Thrombus Formation
The processes leading to thrombosis and embolism are complex and not completely understood.
Atherosclerosis and other abnormalities affecting the vascular endothelium can serve as a stimulus for platelet aggregation and blood coagulation in arteries. Venous pooling, sluggish blood flow, and inflammation of veins may permit inappropriate platelet adhesion and coagulation in vessels. Platelet aggregation appears to have a larger role in the formation of arterial thrombi (white thrombi), whereas coagulation predominates in the formation of venous thrombi (red thrombi). Platelet aggregation followed by coagulation, however, occurs both in arteries and in veins, and the processes differ only in the degree of contribution by platelets or coagulation to the thrombus.
An arterial or venous thrombus can become dislodged from the vessel wall and form an embolus that travels through the circulation and eventually occludes a smaller vessel in the lungs or brain, thereby causing pulmonary embolism or a cerebrovascular accident (stroke), respectively.
ANTICOAGULANT DRUGS
Oral Anticoagulants
Anticoagulants are drugs that retard coagulation and thereby prevent the occurrence or enlargement of a thrombus. Table 16–2 compares the properties of oral anticoagulants (e.g., warfarin) with those of parenteral anticoagulants (e.g., heparin).
TABLE 16–2 Comparison of the Pharmacologic Properties of Warfarin and Heparin Anticoagulants
| Property | Warfarin Anticoagulants | Heparin Anticoagulants |
|---|---|---|
| Active in vitro | No | Yes |
| Routes of administration | Oral | Parenteral |
| Onset of action | Delayed | Immediate |
| Mechanism of action | Inhibit synthesis of clotting factors | Inactivate clotting factors |
| Safe to take during pregnancy | No | Yes |
| Antidote | Phytonadione (vitamin K1) | Protamine sulfate |
Drug Properties
CHEMISTRY AND MECHANISMS
Coumarin compounds were originally discovered in spoiled clover hay and identified as substances that caused hemorrhage in cattle. Coumarin derivatives (e.g., warfarin and dicumarol) were subsequently developed as anticoagulants.
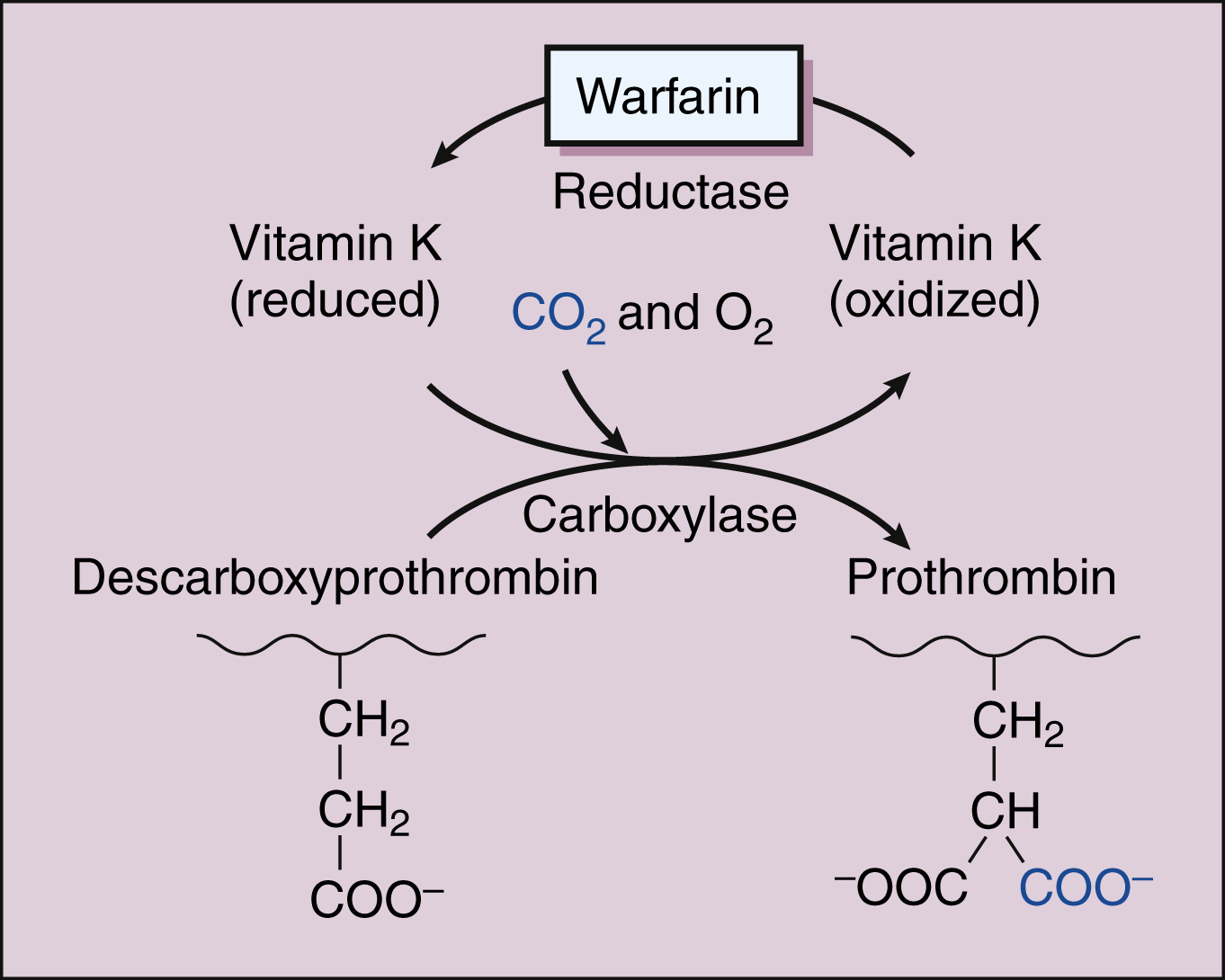
Warfarin and other coumarin derivatives are structurally related to vitamin K. These drugs work by inhibiting the synthesis of clotting factors II (prothrombin), VII, IX, and X, whose carboxylation is dependent on a reduced form of vitamin K. As shown in Figure 16–3, warfarin blocks the reduction of oxidized vitamin K and thereby prevents the post-translational carboxylation of these four factors. Oral anticoagulants also inhibit the synthesis of proteins C and S, which are endogenous anticoagulants that inactivate factors V and VIII and promote fibrinolysis. It is possible that the inhibition of proteins C and S contributes to a transient procoagulant effect of the oral anticoagulants when they are first administered.
PHARMACOKINETIC AND PHARMACOLOGIC EFFECTS
Coumarin anticoagulants, which are absorbed from the gut, are extensively metabolized before being excreted in the urine. Unlike heparin and related anticoagulants, the coumarins cross the placenta and can cause fetal hemorrhage and malformations.
The vitamin K antagonists have a delayed onset of action, owing to the time required to deplete the pool of circulating clotting factors after synthesis of new factors is inhibited. The half-life of circulating factors II, VII, IX, and X ranges from 6 hours (factor VII) to 50 hours (factor II). Therefore, the maximal effect of oral anticoagulants is not observed until 3 to 5 days after starting therapy with these drugs. Patients with acute thromboembolism are usually treated with a low-molecular-weight heparin (LMWH) and warfarin, and the LMWH is then withdrawn after warfarin becomes effective. A period of several days is also required for coagulation factor levels to return to normal after coumarin anticoagulants are discontinued. The recovery of clotting factors can be accelerated by administration of phytonadione (vitamin K1), as described later.
ADVERSE EFFECTS AND INTERACTIONS
The most common adverse effect of coumarin anticoagulants is bleeding (Table 16–3), which can range in severity from mild nosebleed to life-threatening hemorrhage. Patients should be instructed to report any signs of bleeding, including hematuria and bleeding into the skin (ecchymoses).
TABLE 16–3 Adverse Effects and Drug Interactions of Anticoagulant, Antiplatelet, and Fibrinolytic Drugs
| Drug | Common Adverse Effects | Common Drug Interactions |
|---|---|---|
| Oral Anticoagulants | ||
| Warfarin | Birth defects and bleeding | Serum levels altered by drugs that induce or inhibit cytochrome P450, by drugs that inhibit gut absorption, and by drugs that directly increase or decrease the anticoagulant effect (see text) |
| Parenteral Anticoagulants | ||
| Dalteparin | Bleeding and thrombocytopenia | Risk of bleeding increased by salicylates |
| Enoxaparin heparin | Same as dalteparin | Same as dalteparin |
| Bleeding, hyperkalemia, and thrombocytopenia | Same as dalteparin | |
| Hirudin and related drugs | Bleeding | Same as dalteparin |
| Antiplatelet Drugs | ||
| Abciximab | Bleeding, bradycardia, hypotension, and thrombocytopenia | Unknown |
| Aspirin | Gastrointestinal irritation and bleeding, hypersensitivity reactions, and tinnitus | Increases hypoglycemic effect of sulfonylureas. Increases risk of gastrointestinal bleeding and ulceration associated with methotrexate, valproate, and other drugs. Inhibits uricosuric effect of probenecid |
| Dipyridamole | Gastrointestinal distress, headache, mild and transient dizziness, and rash | Decreases metabolism of adenosine. Increases risk of bradycardia associated with β-adrenergic receptor antagonists |
| Clopidogrel | Bleeding, diarrhea, gastrointestinal pain, increased cholesterol and triglyceride levels, nausea, and neutropenia | Increases levels of drugs metabolized by liver microsomal enzymes |
| Fibrinolytic Drugs | Bleeding, hypersensitivity reactions, and reperfusion arrhythmias | Increases risk of bleeding associated with anticoagulant and antiplatelet drugs |
The coumarin anticoagulants are contraindicated in pregnancy because of their potential to cause fetal hemorrhage and various structural malformations referred to as the fetal warfarin syndrome. These malformations are caused partly by antagonism of vitamin K–dependent maturation of bone proteins during a process in which certain proteins undergo carboxylation in the same manner as the nascent clotting factors. Warfarin and other oral anticoagulants block the process and can cause bone deformities and various birth defects that are listed in Table 4–6.
Most drug interactions with warfarin and other coumarin anticoagulants are caused by induction or inhibition of cytochrome P450 (CYP) enzymes, but a few are caused by the antagonism or potentiation of the anticoagulant effect. The most serious interactions are with drugs that increase the anticoagulant effect and place the patient at risk for hemorrhage. Because the number of drugs that interact with warfarin is large, patients who are taking this drug should be instructed to consult their physician before starting or discontinuing any other medication.
Treatment with high doses of salicylates or with some third-generation cephalosporins has a direct hypoprothrombinemic effect and thereby increases the anticoagulant effect of warfarin and related drugs. In contrast, treatment with rifampin or barbiturates induces CYP enzymes and thereby decreases the anticoagulant effect of warfarin. Cholestyramine inhibits the absorption of warfarin from the gut. Amiodarone, cimetidine, erythromycin, fluconazole, gemfibrozil, isoniazid, metronidazole, sulfinpyrazone, and other drugs inhibit the metabolism of warfarin and increase the risk of bleeding. The prothrombin time (PT) should be monitored when adding or deleting drugs with persons taking coumarin anticoagulants.
Phytonadione directly antagonizes the effect of coumarin anticoagulants on clotting factor synthesis and is used to treat hemorrhage caused by anticoagulant activity.
INDICATIONS
Warfarin and related anticoagulants are primarily used in the long-term treatment of patients who have a thromboembolic disorder such as deep vein thrombosis or atrial fibrillation and patients who have an artificial heart valve (Table 16–4). They are also used in conjunction with a heparin-type anticoagulant for the treatment of myocardial infarction. The goal of anticoagulant use is to inhibit embolization and thereby prevent the serious and potentially fatal sequelae of thrombosis. Anticoagulants can keep an established thrombus from extending, but they cannot dissolve one.
TABLE 16–4 Clinical Uses of Antithrombotic Agents
| Clinical Use | Primary Drugs |
|---|---|
| Venous Thromboembolism | |
| Acute | LMWH |
| Surgical prophylaxis | LMWH or fondaparinux |
| Long-term prophylaxis | Warfarin or LMWH |
| Pulmonary embolism | Heparin, fibrinolytic drug |
| Acute Coronary Syndromes | |
| Unstable angina and non-STE ACS | Aspirin ± clopidogrel; eptifibatide or tirofiban; LMWH |
| STEMI | Fibrinolytic drug and aspirin ± heparin |
| Percutaneous coronary interventions∗ | Aspirin ± clopidogrel; abciximab or eptifibatide (alternative: bivalirudin) |
| Stroke, thrombotic | |
| Acute | Fibrinolytic drug or aspirin |
| Prophylaxis, including transient ischemic attacks | Aspirin and dipyridamole combined; clopidogrel or prasugrel |
| Atrial fibrillation | Heparin followed by warfarin |
| Artificial heart valve | Warfarin, aspirin |
LMWH = low-molecular-weight heparin; non-STE ACS = non–ST segment elevation acute coronary syndrome; STEMI = ST segment elevation myocardial infarction.
∗ Coronary angioplasty and stent placement.
The dosage of oral anticoagulants to be given is based on the patient’s PT. This measurement is determined by drawing a blood sample, adding a tissue thromboplastin preparation to initiate coagulation in it, and comparing the in vitro clotting time in the sample with that in a standardized control preparation. As a general rule, the dosage of warfarin to be given should prolong the PT of the patient so that it is 1.3 to 1.5 times the PT of the control.
When the international reference thromboplastin preparation is used as the standardized control preparation, the ratio is expressed as the international normalized ratio (INR) and is calculated as follows:
where the PTobserved and PTcontrol are the prothrombin times of the patient and control, respectively, and the ISI is the international sensitivity index of the thromboplastin reagent being used. For most indications, an INR of 2 to 3 is recommended. For patients with mechanical prosthetic heart valves and for those with recurrent systemic embolization, an INR of 3 to 4.5 is recommended.
The patient’s PT should be monitored daily during the initiation of warfarin therapy and whenever another drug is added to or withdrawn from the treatment regimen. Concurrent heparin therapy can cause an increase of 10% to 20% in the patient’s PT, so the target PT and INR levels should be increased by the same amount. Once the patient’s PT has stabilized, it should be monitored every 4 to 6 weeks.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree