DRUG CLASSES
Oxytocic drugs
Tocolytics
PHARMACOLOGY IN PRACTICE

Betty Peterson’s daughter has been admitted to the obstetric unit and is being induced. This is her daughter’s first child, and Betty is extremely anxious. After reading this chapter, think about the information that would be helpful to the family.
Drug therapy is beneficial for use in labor and delivery to promote the well-being of a woman and her fetus. Depending on the patient’s need, drugs may be used to stimulate, intensify, or inhibit uterine contractions. The two types of drugs discussed in this chapter for their effect on the uterus are the oxytocics and the tocolytics. Drugs acting on the uterus are listed in the Summary Drug Table: Uterine Drugs.
OXYTOCIC DRUGS
Oxytocic drugs are used antepartum (before birth of the neonate) to induce uterine contractions similar to those of normal labor. These drugs are desirable when vaginal delivery has not begun and when it is in the best interest of the woman and the fetus to initiate it. An oxytocic drug is one that stimulates the uterus.
Action and Uses
Oxytocin
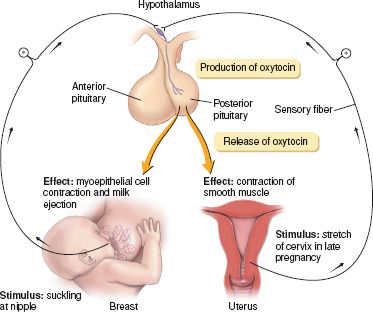
Oxytocin is an endogenous hormone produced by the posterior pituitary gland (Fig. 46.1). This hormone has uterus-stimulating properties, acting on the smooth muscle of the uterus, especially on the pregnant uterus. As pregnancy progresses, the sensitivity of the uterus to oxytocin increases, reaching a peak immediately before the birth of the infant. This sensitivity enables oxytocic drugs to exert their full therapeutic effect on the uterus and produce the desired results. Oxytocin also has antidiuretic and vasopressor effects.
Figure 46.1 Regulation and effect of the hormone oxytocin. (From Premkumar, K. [2004]. The massage connection: Anatomy and physiology. Baltimore: Lippincott Williams & Wilkins.)
Oxytocin is administered intravenously (IV) for starting or improving labor contractions. Drugs may be used to induce an early vaginal delivery when there are fetal or maternal problems, such as a woman with diabetes and a large fetus, Rh problems, premature rupture of the membranes, uterine inertia, and preeclampsia (also called pregnancy-induced hypertension). Preeclampsia is a condition of pregnancy characterized by hypertension, headache, albuminuria, and edema of the lower extremities occurring at, or near, term. The condition may progressively worsen until eclampsia (a serious condition occurring between the 20th week of pregnancy and the end of the first week postpartum and characterized by convulsive seizures and coma) occurs. Oxytocin may also be used in managing inevitable or incomplete abortion. Oxytocin can be given intramuscularly (IM) during the third stage of labor (period from the time the neonate is expelled until the placenta is expelled) to produce uterine contractions and control postpartum bleeding and hemorrhage. Some women find that when taken intranasally to stimulate the milk ejection (milk letdown) reflex they can breastfeed successfully. Although intranasal preparations are not commercially available, compounding pharmacies have made them for women.
Other Uterine Stimulants
Uterine stimulants increase the strength, duration, and frequency of uterine contractions and decrease the incidence of uterine bleeding. They are given after the delivery of the placenta and are used to prevent postpartum and postabortal hemorrhage caused by uterine atony (marked relaxation of the uterine muscle). These drugs include carboprost, methylergonovine, and misoprostol.
Adverse Reactions
Oxytocin
Administration of oxytocin may result in the following:
• Fetal bradycardia, uterine rupture, uterine hypertonicity
• Nausea, vomiting, cardiac arrhythmias, anaphylactic reactions
Oxytocin is similar to the hormone vasopressin and because of its antidiuretic effect, serious water intoxication (fluid overload, fluid volume excess) may occur, particularly when the drug is administered by continuous infusion and the patient is receiving fluids by mouth.
Other Uterine Stimulants
Adverse reactions associated with other uterine stimulants include the following:
• Nausea, vomiting, diarrhea
• Elevated blood pressure, temporary chest pain
• Dizziness, water intoxication, headache
Allergic reactions may also occur. In some instances hypertension associated with seizure or headache may occur.
Contraindications, Precautions, and Interactions
Oxytocin is contraindicated in patients with known hypersensitivity to the drug, cephalopelvic disproportion, and unfavorable fetal position or presentation. It is also contraindicated in obstetric emergencies, situations of fetal distress when delivery is not imminent, severe preeclampsia, eclampsia, and hypertonic uterus, as well as during pregnancy when there is total placenta previa. It is contraindicated as an agent to induce labor when vaginal delivery is contraindicated. Oxytocin is not expected to be a risk to the fetus when administered as indicated. When oxytocin is administered with vasopressors, however, severe maternal hypertension may occur.
Methylergonovine is not used before delivery of the placenta. It is contraindicated in those with known hypersensitivity to the drug or hypertension. This drug is used cautiously in patients with heart disease, vascular disease with narrowed vessels, and renal or hepatic disease, and during lactation. When methylergonovine is administered concurrently with vasopressors or to patients who are heavy cigarette smokers, excessive vasoconstriction may occur.
PATIENT TEACHING FOR MEDICATION INFORMATION
ASSESSMENT
Preadministration Assessment
Before starting an IV infusion of oxytocin to induce labor, obtain an obstetric history (e.g., parity, gravidity, previous obstetric problems, type of labor, stillbirths, abortions, live-birth infant abnormalities) and a general health history.
Keep a record of the activity of the uterus (strength, duration, and frequency of contractions, if any). Monitoring uterine contractions for strength and length of the contractions can be done with an external monitor or by an internal uterine catheter with an electronic monitor. A fetal monitor is placed to assess the fetal heart rate (FHR). Immediately before starting the IV infusion of oxytocin, assess and document the FHR and the patient’s blood pressure, pulse, and respiratory rate.
The other uterine stimulants may be given orally or IM during the postpartum period to reduce the possibility of postpartum hemorrhage and to prevent relaxation of the uterus. When the patient is to receive any of these drugs after delivery, it is important to take the blood pressure, pulse, and respiratory rate before administration.
Ongoing Assessment
After injecting an oxytocic drug, both the mother’s contractions and the fetal heart rate are monitored continuously. Three to four firm uterine contractions should occur every 10 minutes, followed by a palpable relaxation of the uterus. Hyperstimulation of the uterus during labor may lead to uterine tetany with marked impairment of the uteroplacental blood flow, uterine rupture, cervical rupture, amniotic fluid embolism, and trauma to the infant. Overstimulation of the uterus is dangerous to both the fetus and the mother and may occur even when the drug is administered properly in a uterus that is hypersensitive to oxytocin.
 NURSING ALERT
NURSING ALERT
All patients receiving IV oxytocin must be under constant observation to identify complications. In addition, the health care provider attending the delivery should be immediately available at all times.
When monitoring uterine contractions, notify the health care provider attending the delivery immediately if any of the following occurs:
 A significant change in the FHR or rhythm
A significant change in the FHR or rhythm
 A marked change in the frequency, rate, or rhythm of uterine contractions; uterine contractions lasting more than 60 seconds; or contractions occurring more frequently than every 2 to 3 minutes, or no palpable relaxation of the uterus
A marked change in the frequency, rate, or rhythm of uterine contractions; uterine contractions lasting more than 60 seconds; or contractions occurring more frequently than every 2 to 3 minutes, or no palpable relaxation of the uterus
 A marked increase or decrease in the patient’s blood pressure or pulse or any significant change in the patient’s general condition (vital signs are typically obtained every 15 to 30 minutes in active labor)
A marked increase or decrease in the patient’s blood pressure or pulse or any significant change in the patient’s general condition (vital signs are typically obtained every 15 to 30 minutes in active labor)
If any of these conditions are noted, immediately discontinue the oxytocin infusion and run the primary IV line at the rate prescribed by the health care provider attending the delivery until the patient is examined.
Report any signs of water intoxication or fluid overload (e.g., drowsiness, confusion, headache, listlessness, and wheezing, coughing, or rapid breathing) to the health care provider attending the delivery.
Oxytocin may be given IM after delivery of the placenta. After administering the drug, continue to take vital signs every 5 to 10 minutes. Palpate the patient’s uterine fundus for firmness and position. Report immediately any excess bleeding to the health care provider attending the delivery.
When administering methylergonovine after delivery, monitor vital signs every 4 hours and also note the character and amount of vaginal bleeding. The patient may report abdominal cramping with the administration of these drugs. If cramping is moderately severe to severe, contact the health care provider attending the delivery because it may be necessary to discontinue use of the drug.
NURSING DIAGNOSES
Drug-specific nursing diagnoses include the following:
 Anxiety related to fears associated with the process of labor and delivery
Anxiety related to fears associated with the process of labor and delivery
 Risk for Injury (fetal) related to adverse drug effects of oxytocin on the fetus (fetal bradycardia)
Risk for Injury (fetal) related to adverse drug effects of oxytocin on the fetus (fetal bradycardia)
 Excess Fluid Volume related to administration of IV fluids and the antidiuretic effects associated with oxytocin
Excess Fluid Volume related to administration of IV fluids and the antidiuretic effects associated with oxytocin
 Acute Pain related to adverse reactions (abdominal cramping, nausea, headache)
Acute Pain related to adverse reactions (abdominal cramping, nausea, headache)
Nursing diagnoses related to drug administration are discussed in Chapter 4.
PLANNING
The expected patient outcomes may include an optimal response to drug therapy (e.g., initiation of the normal labor process), adverse reactions (e.g., absence of a fluid volume excess with oxytocin administration) identified and reported to the health care provider attending the delivery, and confidence in an understanding of the medication regimen.
IMPLEMENTATION
Promoting an Optimal Response to Therapy
OXYTOCIN. When oxytocin is prescribed, the drug may come in a premixed solution such as 10 units in 1,000 mL of solution (0.01 units/1 mL). By using premixed solutions, errors are prevented because all patients are using the same dilution in a solution. An electronic infusion device is used to control the infusion rate. Frequently, health care providers attending deliveries establish protocol guidelines for administering the oxytocin solution and for increasing or decreasing the flow rate or discontinuing the administration of oxytocin. The flow rate is usually increased every 20 to 30 minutes, but this may vary according to the patient’s response. The strength, frequency, and duration of contractions and the FHR are monitored closely.
METHYLERGONOVINE. Administer methylergonovine at the direction of the health care provider attending the delivery. Methylergonovine is usually given IM at the time of the delivery of the anterior shoulder or after the delivery of the placenta. The drug is not given routinely IV because it may produce sudden hypertension and stroke. If the drug is ordered IV, administer it slowly over a period of 1 minute or more with close monitoring of the patient’s blood pressure. Although you may try to explain the purpose of the drug, which is to improve the tone of the uterus and help the uterus to return to its (near) normal size, the excitement of a new baby may interfere with the mother’s understanding. You may need to repeat this should she wonder about the uterine sensations.
Misoprostol tablets are administered vaginally to induce or augment uterine contractions. Care should be taken that hyperstimulation of the uterus causing uterine tetany does not occur.
Monitoring and Managing Patient Needs
ANXIETY. When given to induce or stimulate contractions, oxytocin is given IV. The patient receiving oxytocin may have concern over the use of the drug to produce contractions. This may be contrary to the birth plan of the mother. By explaining the purpose of the IV infusion and the expected results to the patient, you can be supportive of her desires for a successful birth. Because the patient receiving oxytocin must be closely supervised, use the time with the patient to offer encouragement and reassurance to help reduce anxiety.
RISK FOR INJURY (FETAL). When oxytocin is administered, some adverse reactions must be tolerated or treated symptomatically until therapy is discontinued. For example, if the patient is nauseated, provide an emesis basin and perhaps a cool towel for the forehead. If vomiting occurs, provide rinsing solutions to freshen the mouth.
If contractions are frequent, prolonged, or excessive, the infusion is stopped to prevent fetal anoxia or trauma to the uterus. Excessive stimulation of the uterus can cause uterine hypertonicity and possible uterine rupture. Place the patient on her left side and provide supplemental oxygen. The effects of the drug diminish rapidly, because oxytocin is a short- acting drug.
EXCESS FLUID VOLUME. Track fluid intake and output; when oxytocin is administered IV, there is a danger of an excessive fluid volume (water intoxication), because oxytocin has an antidiuretic effect. In some instances, hourly measurements of output are necessary. Observe the patient for signs of fluid overload (see Chapter 54). If any of these signs or symptoms is noted, immediately discontinue the oxytocin infusion but let the primary IV line run at the rate ordered until the patient is examined.
ACUTE PAIN. When methylergonovine is administered for uterine atony and hemorrhage, abdominal cramping can occur and is usually an indication of drug effectiveness. The uterus is palpated in the lower abdomen as small, firm, and round. However, report persistent or severe cramping to the primary health care provider.
Educating the Patient and Family
The treatment regimen is explained to the patient and family (when appropriate). Answer any questions the patient may have regarding treatment and instruct the patient to report any adverse reactions. Also inform the patient and family about the therapeutic response during administration of the drug, and if nasal spray is to be used, teach the patient the proper technique.
EVALUATION
 Therapeutic effect is achieved and normal labor is initiated.
Therapeutic effect is achieved and normal labor is initiated.
 Adverse reactions are identified, reported to the primary health care provider, and managed successfully through appropriate nursing interventions:
Adverse reactions are identified, reported to the primary health care provider, and managed successfully through appropriate nursing interventions:
• Anxiety is managed successfully.
• No evidence of injury is seen.
• Fluid volume balance is maintained.
• Patient is free of pain.
 Patient expresses confidence and demonstrates an understanding of the drug regimen.
Patient expresses confidence and demonstrates an understanding of the drug regimen.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree