DRUG CLASSES
Active immunity agents
• Vaccines, bacterial and viral
• Toxoids
Passive immunity agents
• Immune globulins
• Antivenins
PHARMACOLOGY IN PRACTICE

Betty Peterson’s niece has been staying with Betty since the niece was laid off from her job. She received health insurance from her previous employer; now without it, she has to make choices about when to go to the clinic. She cannot always find the money to pay for the visit. Jimmy is Betty’s 4-month-old grandnephew; determine where he is in the immunization schedules assuming he is up-to-date with these.
Immunity refers to the ability of the body to identify and resist microorganisms that are potentially harmful. This ability enables the body to fight or prevent infectious disease and inhibit tissue and organ damage. The immune system is not confined to any one part of the body. Immune stem cells, formed in the bone marrow, may remain in the bone marrow until maturation, or they may migrate to different body sites for maturation. After maturation, most immune cells circulate in the body and exert specific effects. The immune system has two distinct, but overlapping, mechanisms with which to fight invading organisms:
• Cell-mediated defenses (cell-mediated immunity)
• Antibody-mediated defenses (humoral immunity)
Cell-Mediated Immunity (T Cells)
Cell-mediated immunity (CMI) results from the activity of many leukocyte actions, reactions, and interactions that range from simple to complex. This type of immunity depends on the actions of the T lymphocytes, which are responsible for a delayed type of immune response. The T lymphocytes defend against viral infections, fungal infections, and some bacterial infections as follows.
• The T lymphocyte becomes sensitized by its first contact with a specific antigen.
• Subsequent exposure to an antigen stimulates multiple reactions aimed at destroying or inactivating the offending antigen.
• T lymphocytes and macrophages (large cells that surround, engulf, and digest microorganisms and cellular debris) work together in CMI to destroy the antigen.
• T lymphocytes attack the antigens directly, rather than produce antibodies (as is done in humoral immunity). Cellular reactions may also occur without macrophages.
If CMI is reduced, as in the case of acquired immunodeficiency syndrome (AIDS), the body is unable to protect itself against many viral, bacterial, and fungal infections.
Humoral Immunity (B Cells)
Humoral immunity protects the body against bacterial and viral infections. Special lymphocytes (white blood cells), called B lymphocytes, produce circulating antibodies to act against a foreign substance. This type of immunity is based on the antigen–antibody response. An antigen is a substance, usually a protein, that stimulates the body to produce antibodies. An antibody is a globulin (protein) produced by the B lymphocytes as a defense against an antigen.
Specific antibodies are formed for specific antigens—for example, chickenpox antibodies are formed when the person is exposed to the chickenpox virus (the antigen). Once manufactured, antibodies circulate in the bloodstream, sometimes only for a short time, but in other cases for the lifetime of the person. When an antigen enters the body, specific antibodies neutralize the invading antigen; this condition is called immunity. Thus, the individual with specific circulating antibodies is immune (or has immunity) to a specific antigen. Immunity is the resistance that an individual has against disease.
Cell-mediated and humoral immunity are interdependent; CMI influences the function of the B lymphocytes, and humoral immunity influences the function of the T lymphocytes.
Active and Passive Immunity
Active and passive immunity involve the use of agents that stimulate antibody formation (active immunity) or the injection of ready-made antibodies found in the serum of immune individuals or animals (passive immunity). See Figure 49.1.
Active Immunity
When a person is exposed to certain infectious microorganisms (the source of antigens), the body actively builds an immunity (forms antibodies) to the invading microorganism. This is called active immunity. There are two types of active immunity: (1) naturally acquired active immunity and (2) artificially acquired active immunity. The Summary Drug Table: Immunization Agents identifies agents that produce active immunity.
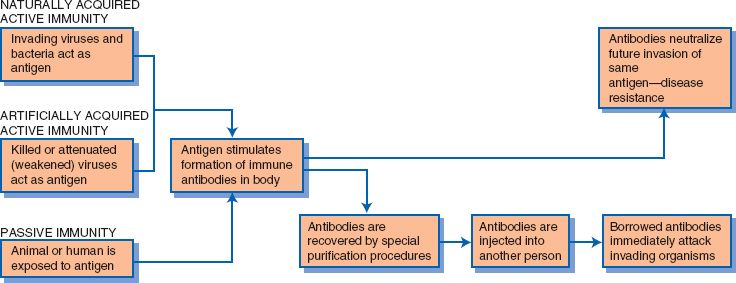
Figure 49.1 Active and passive immunity.
Display 49.1 Example of Naturally Acquired Active Immunity
Naturally acquired active immunity is exemplified by an individual who is exposed to chickenpox for the first time and who has no immunity to the disease. The body immediately begins to manufacture antibodies against the chickenpox virus. However, the production of a sufficient quantity of antibodies takes time, and the individual gets the disease. At the time of exposure and while the individual still has chickenpox, the body continues to manufacture antibodies. These antibodies circulate in the individual’s bloodstream for life. In the future, any exposure to the chickenpox virus results in the antibodies mobilizing to destroy the invading antigen.
Naturally Acquired Active Immunity
Naturally acquired active immunity occurs when the person is exposed to and experiences a disease, and the body manufactures antibodies to provide future immunity to the disease. This is called active immunity because the antibodies are produced by the person who had the disease (see Fig. 49.1). Thus, having the disease produces immunity. Display 49.1 describes an example of naturally acquired active immunity.
Artificially Acquired Active Immunity
Artificially acquired active immunity occurs when an individual is given a killed or weakened antigen, which stimulates the formation of antibodies against the antigen. The antigen does not cause the disease, but the individual still manufactures specific antibodies against the disease. When a vaccine containing an attenuated (weakened) antigen is given, the individual may experience a few minor symptoms of the disease or even a mild form of the disease, but the symptoms are almost always milder than the disease itself and usually last for a short time.
The decision to use an attenuated rather than a killed virus as a vaccine to provide immunity is based on research in the laboratory to see what form is effective on the virus. Many antigens, when killed, produce a poor antibody response, whereas when the antigen is merely weakened, a good antibody response occurs. Immunization against a specific disease provides artificially acquired active immunity. Display 49.2 gives an example of artificially acquired active immunity.
Artificially acquired immunity against some diseases may require periodic booster injections to keep an adequate antibody level (or antibody titer) circulating in the blood. A booster injection is the administration of an additional dose of the vaccine to boost the production of antibodies to a level that will maintain the desired immunity. The booster is given months or years after the initial vaccine and may be needed because the life of some antibodies is short.
Immunization is a form of artificial active immunity and an important method of controlling some of the infectious diseases that are capable of causing serious and sometimes fatal consequences. The immunization schedule for children and adults is provided in Appendix C. Changes can be made frequently to these schedules. It is best to check the most current immunization schedules for this and other age groups and late start schedules, all of which can be obtained at the Centers for Disease Control and Prevention (CDC) website at http://www.cdc.gov/vaccines/. Currently, many infectious diseases may be prevented by vaccine (artificial active immunity). Examples of some of these diseases can be found in Display 49.3.
Display 49.2 Example of Artificially Acquired Active Immunity
Although chickenpox may seem like a minor illness, it can cause herpes zoster (shingles) later in life, which is a painful condition. An example of the use of an attenuated virus is the administration of the varicella virus vaccine to an individual who has not had chickenpox. The varicella (chickenpox) vaccine contains the live, attenuated varicella virus. The individual receiving the vaccine develops a mild or modified chickenpox infection, which then produces immunity against the varicella virus. The varicella vaccine protects the recipient for several years or, for some individuals, for life. An example of a killed virus used for immunization is the yearly influenza vaccine. These vaccines protect those who receive the vaccine for about 3 to 6 months. This is why they are given yearly.
Display 49.3 Examples of Diseases Preventable by Vaccination
Diseases Prevented by Routine Vaccination
• Haemophilus influenzae type B
• Hepatitis A
• Hepatitis B
• Human papillomavirus
• Influenza
• Mumps
• Measles
• Pertussis
• Pneumococcal disease
• Poliomyelitis
• Rubella
• Tetanus
• Varicella
Diseases Preventable by Vaccination Before Travel to Endemic Areas
• Cholera
• Diphtheria
• Japanese encephalitis
• Lyme disease
• Smallpox
• Typhoid
• Yellow fever
Display 49.4 Example of Passive Immunity
An example of passive immunity is the administration of immune globulins to prevent organ rejection in patients after organ transplantation surgery.
Passive Immunity
Passive immunity occurs when immune globulins or antivenins are administered. This type of immunity provides the individual with ready-made antibodies from another human or an animal (see Fig. 49.1). Passive immunity provides immediate immunity to the invading antigen, but lasts for only a short time. Display 49.4 provides an example of passive immunity.
IMMUNOLOGIC AGENTS
Some immunologic agents capitalize on the body’s natural defenses by stimulating the immune response, thereby creating protection against a specific disease within the body. Other immunologic agents supply ready-made antibodies to provide passive immunity. Examples of immunologic agents include vaccines, toxoids, and immune globulins.
Actions and Uses
Vaccines and Toxoids
Antibody-producing tissues cannot distinguish between an antigen that is capable of causing disease (a live antigen), an attenuated antigen, or a killed antigen. Because of this phenomenon, vaccines, which contain either an attenuated or a killed antigen, have been developed to create immunity to certain diseases. The live antigens are either killed or weakened during the manufacturing process. The weakened or killed antigens contained in the vaccine do not have sufficient strength to cause disease. Although it is a rare occurrence, vaccination with any vaccine may not result in a protective antibody response in all individuals given the vaccine.
A toxin is a poisonous substance produced by a bacterium (such as Clostridium tetani, the bacterium that causes tetanus). A toxin is capable of stimulating the body to produce antitoxins, which are substances that act in the same manner as antibodies. Toxins are powerful substances and, like other antigens, they can be attenuated. A toxin that is attenuated (or weakened) but still capable of stimulating the formation of antitoxins is called a toxoid.
Both vaccines and toxoids are administered to stimulate the body’s immune response to specific antigens or toxins. These agents must be administered before exposure to the disease-causing organism. The initiation of the immune response, in turn, produces resistance to a specific infectious disease. The immunity produced in this manner is active immunity.
Vaccines and toxoids are used for the following:
• Routine immunization of infants and children
• Immunization of adults against tetanus
• Immunization of adults at high risk for certain diseases (e.g., pneumococcal and influenza vaccines)
• Immunization of children or adults at risk for exposure to a particular disease (e.g., hepatitis A for those going to endemic areas)
• Immunization of prepubertal girls or nonpregnant women of childbearing age against rubella
Immune Globulins and Antivenins
Globulins are proteins present in blood serum or plasma that contain antibodies. Immune globulins are solutions obtained from human or animal blood containing antibodies that have been formed by the body to specific antigens. Because they contain ready-made antibodies, they are given for passive immunity against disease. The immune globulins are administered to provide passive immunization to one or more infectious diseases. Those receiving immune globulins receive antibodies only to the diseases to which the donor blood is immune. The onset of protection is rapid but of short duration (1 to 3 months).
Antivenins are used for passive, transient protection from the toxic effects of bites by spiders (black widow and similar spiders) and snakes (rattlesnakes, copperhead and cottonmouth, and coral). The most effective response is obtained when the drug is administered within 4 hours after exposure.
Adverse Reactions
Vaccines and Toxoids
Adverse reactions from the administration of vaccines or toxoids are usually mild. Chills, fever, muscular aches and pains, rash, and lethargy may be present. Pain and tenderness at the injection site may also occur. Although rare, a hypersensitivity reaction may occur. The Summary Drug Table: Immunization Agents provides a listing of the typical adverse reactions.
Immune Globulins and Antivenins
Adverse reactions to immune globulins are rare. However, local tenderness and pain at the injection site may occur. The most common adverse reactions include urticaria, angioedema, erythema, malaise, nausea, diarrhea, headache, chills, and fever. Adverse reactions, if they occur, may last for several hours. Systemic reactions are extremely rare, with the exception of immune globulins given to prevent posttransplantation rejection. These immune globulins are made from equine (horse) or rabbit serum and can produce anaphylactic reactions. They should be administered only under the direction of a physician specializing in transplantation medicine.
The antivenins may cause various reactions, with hypersensitivity being the most severe. Some antivenins are prepared from equine serum, and if a patient is sensitive to equine serum, serious reactions or death may result. The immediate reactions usually occur within 30 minutes after administration of the antivenin. Symptoms include apprehension; flushing; itching; urticaria; edema of the face, tongue, and throat; cough; dyspnea; vomiting; cyanosis; and collapse. Other adverse reactions are included in the Summary Drug Table: Immunization Agents.
Contraindications and Precautions
Vaccines and Toxoids
Immunologic agents are contraindicated in patients with known hypersensitivity to the agent or any component of it. Allergy to eggs is a concern with some vaccines. It is recommended to see a primary health care provider familiar with egg allergies for vaccination if an allergy is suspected. Some people with “hive-only” reactions are able to tolerate vaccines without problem (ACIP, 2012). The measles, mumps, rubella, and varicella vaccines are contraindicated in patients who have had an allergic reaction to gelatin, neomycin, or a previous dose of one of the vaccines. The measles, mumps, rubella, and varicella vaccines are contraindicated during pregnancy, especially during the first trimester, because of the danger of birth defects. Women are instructed to avoid becoming pregnant at least 3 months after receiving these vaccines. Vaccines and toxoids are contraindicated during acute febrile illnesses, leukemia, lymphoma, immunosuppressive illness or drug therapy, and nonlocalized cancer. Always ask about allergy history before preparing a vaccine for administration. See Display 49.5 for additional information on the contraindications to immunologic agents.
Immunologic agents are used with extreme caution in individuals with a history of allergies. Sensitivity testing may be performed in individuals with a history of allergies. Because of potential harm to a fetus no adequate studies have been conducted in pregnant women, and it is also not known whether these agents are excreted in breast milk. Thus, the immunologic agents (pregnancy category C) are used with caution in pregnant women and during lactation.
Immune Globulins and Antivenins
The immune globulins are contraindicated in patients with a history of allergic reactions after administration of human immunoglobulin preparations and in individuals with isolated immunoglobulin A (IgA) deficiency (individuals could have an anaphylactic reaction to subsequent administration of blood products that contain IgA).
 CHRONIC CARE CONSIDERATIONS
CHRONIC CARE CONSIDERATIONS
Human immune globulin intravenous (IGIV) products have been associated with renal impairment, acute renal failure, osmotic nephrosis, and death. Individuals with a predisposition to acute renal failure (e.g., those with pre-existing renal disease), those with diabetes mellitus, individuals older than 65 years of age, or patients receiving nephrotoxic drugs should not be given human IGIV products.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


