DRUG CLASSES
HMG-CoA reductase inhibitors (statins)
Bile acid resins
Fibric acid derivatives
PHARMACOLOGY IN PRACTICE

Lillian Chase is taking cholestyramine for hyperlipidemia. The primary health care provider has prescribed therapeutic life changes for the patient, who is on a low-fat diet and walks short distances daily for exercise. Her major complaint at this visit is constipation, which is very bothersome to her. She feels depressed and has started smoking again. She tells you the medicine isn’t working and wants to stop taking it. As you read about medications in this chapter, think about Lillian’s concerns.
Atherosclerosis is a disorder in which lipid (fat or fat-like substance) deposits accumulate on the lining of the blood vessels, eventually producing degenerative changes and obstructing blood flow. Atherosclerosis is considered to be a major contributor in the development of heart disease. Cholesterol and the triglycerides are the two lipids in our blood. Elevation of one or both of these lipids occurs in hyperlipidemia. Hyperlipidemia is an increase (hyper) in the lipids in the blood (emia). Serum cholesterol levels above 240 mg/dL and triglyceride levels above 150 mg/dL are associated with atherosclerosis.
Triglycerides and cholesterol are insoluble in water and must be bound to a lipid-containing protein (lipoprotein) for transportation throughout the body (Fig. 34.1). Although several lipoproteins are found in the blood, this chapter focuses on the low-density lipoproteins, the high-density lipoproteins (HDLs), and cholesterol.
Lipoproteins
Low-density lipoproteins (LDLs) transport cholesterol to the peripheral cells. When the cells have all the cholesterol they need, the excess cholesterol is discarded into the blood (see Fig. 34.1). This excess penetrates the walls of the arteries, resulting in atherosclerotic plaque formation. Elevation of the LDL level increases the risk for heart disease. On the other hand, high-density lipoproteins (HDLs) take cholesterol from the peripheral cells and transport it to the liver, where it is metabolized and excreted; the higher the HDL level, the lower the risk for development of atherosclerosis. Therefore, it is desirable to see an increase in the HDL (the “good” lipoprotein) level, because of the protective nature of its properties against the development of atherosclerosis, and a decrease in the LDL level. A laboratory examination of blood lipids, called a lipoprotein profile, provides valuable information on the important cholesterol levels, such as:
• Total cholesterol
• LDL (the harmful lipoprotein)
• HDL (the protective lipoprotein)
• Triglycerides
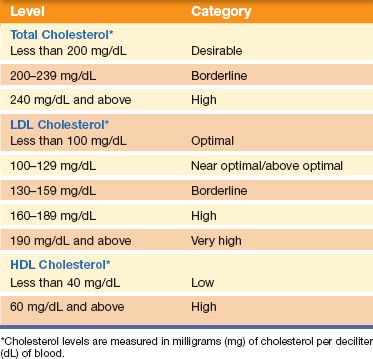
Table 34.1 provides an analysis of cholesterol levels.
Cholesterol Levels
High-density lipoprotein cholesterol protects against heart disease, so the higher its numbers (i.e., blood level), the better. An HDL level less than 40 mg/dL is low and considered a major risk factor for heart disease. Triglyceride levels that are borderline (150 to 190 mg/dL) or high (above 190 mg/dL) may need treatment in some individuals.

Figure 34.1 Cholesterol transport in the blood. (Courtesy of Anatomical Chart Co.)
Table 34.1 Cholesterol Level Analysis
In general, the higher the LDL level and the more risk factors involved, the greater the risk for heart disease. Other risk factors, besides elevated cholesterol levels, that play a role in the development of hyperlipidemia are listed here. Uncontrollable risk factors include:
• Age (men older than 45 years and women older than 55 years)
• Gender (in women after menopause, LDL cholesterol levels increase)
• Family history of early heart disease (father/brother before age 55 years and mother/sister before age 65 years)
Those factors a person can control or modify include:
• Diet (saturated fat and cholesterol in food raise total and LDL cholesterol levels)
• Weight (overweight can make LDL cholesterol level go up and HDL level go down)
• Physical inactivity (increased physical activity helps to lower LDL cholesterol and raise HDL cholesterol levels)
The main goal of treatment in patients with hyperlipidemia is to lower the LDLs to a level that will reduce the risk of heart disease.
The primary health care provider may initially seek to control the cholesterol level by encouraging therapeutic life changes (TLCs). This includes a cholesterol-lowering diet (the TLC diet), physical activity, smoking cessation (if applicable), and weight management. The TLC diet is a low–saturated fat and low-cholesterol eating plan that includes less than 200 mg of dietary cholesterol per day. In addition, 30 minutes of physical activity each day is recommended for the TLC diet. Walking at a brisk pace for 30 minutes a day 5 to 7 days a week can help raise the HDL and lower the LDL levels. Added benefits of a healthy diet and exercise program include a reduction of body weight. If TLCs do not result in bringing blood lipids to therapeutic levels, the primary health care provider may add one of the antihyperlipidemic drugs to the treatment plan. TLCs are continued along with the drug regimen.
In addition to control of the dietary intake of fat, particularly saturated fatty acids, antihyperlipidemic drug therapy is used to lower serum levels of cholesterol and triglycerides. The primary health care provider may use one drug or, in some instances, more than one antihyperlipidemic drug for those with poor response to therapy with a single drug. Three classes of antihyperlipidemic drugs are currently in use, as well as miscellaneous antihyperlipidemic drugs (see Summary Drug Table: Antihyperlipidemic Drugs for a complete listing of the drugs).
The target LDL level for treatment is less than 130 mg/dL. If the response to drug treatment is adequate, lipid levels are monitored every 4 months. If the response is inadequate, another drug or a combination of two drugs is used. Antihyperlipidemic drugs decrease cholesterol and triglyceride levels in several ways. Although the end result is a lower lipid blood level, each has a slightly different action.
Actions
The antihyperlipidemic drugs, HMG-CoA reductase inhibitors, are typically referred to as statins. HMG-CoA (3-hydroxy-
3-methyglutaryl coenzyme A) reductase is an enzyme that is a catalyst (a substance that accelerates a chemical reaction without itself undergoing a change) in the manufacture of cholesterol. These drugs appear to have one of two activities, namely, inhibiting the manufacture of cholesterol or promoting the breakdown of cholesterol. Either drug activity lowers the blood levels of cholesterol, LDLs, and serum triglycerides. Examples of these drugs can be found in the Summary Drug Table: Antihyperlipidemic Drugs.
Uses
Statin drugs, along with a diet restricted in saturated fat and cholesterol, are used for the following:
- Treatment of hyperlipidemia
- Primary prevention of coronary events (in patients with hyperlipidemia without clinically evident coronary heart disease to reduce the risk of myocardial infarction and death from other cardiovascular events, including strokes, transient ischemic attacks, and cardiac revascularization procedures)
- Secondary prevention of cardiovascular events (in patients with hyperlipidemia with evident coronary heart disease to reduce the risk of coronary death, slow the progression of coronary atherosclerosis, and reduce risk of death from stroke/transient ischemic attack; and in those undergoing myocardial revascularization procedures)
Adverse Reactions
The statins are usually well tolerated. Adverse reactions, when they do occur, are often mild and transient and do not require discontinuing therapy. These reactions may include the following.
Central Nervous System Reactions
• Headache
• Dizziness
• Insomnia
• Memory and cognitive impairment
Gastrointestinal System Reactions
• Flatulence, abdominal pain, cramping
• Constipation, nausea
• Hyperglycemia in nondiabetic patients
Contraindications and Precautions
The statins are contraindicated in individuals with hypersensitivity to the drugs or serious liver disorders, and during pregnancy (pregnancy category X) and lactation.
These drugs are used cautiously in patients with a history of alcoholism, non-alcohol-related liver disease, acute infection, hypotension, trauma, endocrine disorders, visual disturbances, and myopathy.
 NURSING ALERT
NURSING ALERT
The drug rosuvastatin in higher doses is linked to risks for serious muscle toxicity (myopathy/rhabdomyolysis) in certain populations. These include patients taking cyclosporine, Asian patients, and patients with severe renal insufficiency. A 5-mg dose is available as a starting dose for those individuals who do not require aggressive cholesterol reductions or who have predisposing factors for myopathy.
Interactions
The following interactions may occur when the statin drugs are administered with another agent:
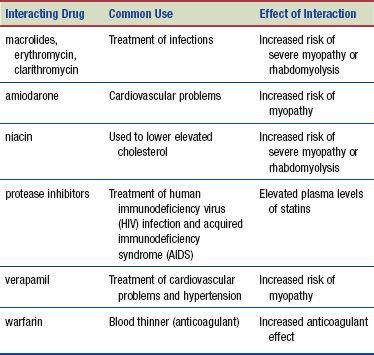
The statin drugs have an additive effect when used with the bile acid resins, which may provide an added benefit in treating hypercholesterolemia that does not respond to a single-drug regimen. Due to a specific enzyme reaction, grapefruit or its juice should not be taken if the patient is on the following drugs: lovastatin or simvastatin.
 HERBAL CONSIDERATIONS
HERBAL CONSIDERATIONS
Red yeast is a traditional Chinese medicine, currently sold as a supplement to lower cholesterol. It comes from an extract of fermented yeast (Monascus purpureus) grown on rice. Its use as an aid for gastric (indigestion, diarrhea, stomach, and spleen) ailments and blood circulation enhancement date back to 800 A.D. in China. It is also used as the red food coloring additive seen in Chinese meats and poultry dishes.
The red yeast naturally contains ingredients that help to control cholesterol levels; these include “healthy fats” and monacolin—the ingredient used in the drug lovastatin. Therefore, the supplement would have all the adverse reactions and drug interactions of the statin drugs. Taking this supplement with antihyperlipidemic drugs can cause serious reactions, notably liver or muscle damage (http://nccam.nih.gov/health/redyeastrice).
Patients may not volunteer information regarding their use of alternative or complementary remedies. You should always inquire about use of herbal products, especially niacin or red yeast purchased as a supplement. Be aware that a possible interaction with St. John’s wort, used to relieve depression, causes a decrease in statin effectiveness.
Actions
Bile, which is manufactured and secreted by the liver and stored in the gallbladder, emulsifies fat and lipids as these products pass through the intestine. Once emulsified, fats and lipids are readily absorbed in the intestine. The bile acid resins bind to bile acids to form an insoluble substance that cannot be absorbed by the intestine, so it is excreted in the feces. With increased loss of bile acids, the liver uses cholesterol to manufacture more bile. This is followed by a decrease in cholesterol levels.
Uses
The bile acid resins are used to treat the following:
• Hyperlipidemia (in patients who do not have an adequate response to a diet and exercise program)
• Pruritus associated with partial biliary obstruction (cholestyramine only)
Adverse Reactions
• Constipation (may be severe and occasionally result in fecal impaction), aggravation of hemorrhoids, abdominal cramps, flatulence, nausea
• Increased bleeding tendencies related to vitamin K malabsorption, and vitamin A and D deficiencies
Contraindications and Precautions
The bile acid resins are contraindicated in patients with known hypersensitivity to the drugs. Bile acid resins are also contraindicated in those with complete biliary obstruction.
These drugs are used cautiously in patients with liver and kidney disease; they are also used cautiously during pregnancy (pregnancy category C) and lactation (decreased absorption of vitamins may affect the infant).
Interactions
The following interactions may occur when the bile acid resins are administered with another agent:
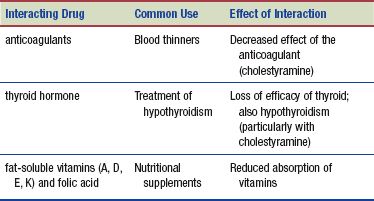
When administered with the bile acid resins, a decreased serum level or decreased gastrointestinal (GI) absorption of the following drugs may occur:
- nonsteroidal anti-inflammatory drugs (NSAIDs; used to treat pain)
- penicillin G and tetracycline (used to treat infection)
- niacin (used to treat elevated cholesterol levels)
- digitalis glycosides (used to treat heart failure)
- furosemide and thiazide diuretics (used to treat edema)
- glipizide (used to treat diabetes)
- hydrocortisone (used to treat inflammation)
- methyldopa and propranolol (used to treat hypertension and cardiovascular problems, respectively)
Because the bile acids resins, particularly cholestyramine, can decrease the absorption of numerous drugs, the bile acid resins should be administered alone and other drugs given at least 1 hour before or 4 hours after administration of the bile acid resins.
Actions
Fibric acid derivatives, also known as fibrates, are the third group of antihyperlipidemic drugs and work in a variety of ways. Fenofibrate acts by reducing very-low-density lipoproteins (VLDLs) and stimulating the catabolism of triglyceride-rich lipoproteins, resulting in a decrease in plasma triglycerides and cholesterol. Gemfibrozil increases the excretion of cholesterol in the feces and reduces the production of triglycerides by the liver, thus lowering serum lipid levels.
Uses
Although the fibric acid derivatives have antihyperlipidemic effects, their use varies depending on the drug. For example, gemfibrozil is used to treat individuals with very high serum triglyceride levels who are at risk for abdominal pain and pancreatitis and who do not experience a response to dietary modifications. Fenofibrate is used as adjunctive treatment for reducing LDLs, total cholesterol, and triglycerides in patients with hyperlipidemia.
Adverse Reactions
The adverse reactions associated with fibric acid derivatives include the following:
• Nausea, vomiting, and GI upset
• Diarrhea
• Cholelithiasis (stones in the gallbladder) or cholecystitis (inflammation of the gallbladder)
If cholelithiasis is found, the primary health care provider may discontinue the drug. See the Summary Drug Table: Antihyperlipidemic Drugs for additional adverse reactions.
Contraindications and Precautions
The fibric acid derivatives are contraindicated in patients with hypersensitivity to the drugs and in those with significant hepatic or renal dysfunction or primary biliary cirrhosis because these drugs may increase the already elevated cholesterol. The drugs are used cautiously during pregnancy (pregnancy category C) and not during lactation or in patients with peptic ulcer disease or diabetes.
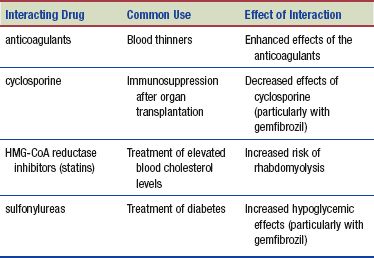
Interactions
The following interactions may occur when the fibric acid derivatives are administered with another agent:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


