DRUG CLASSES
Tetracycline
• Glycylcycline
Aminoglycosides
• Spectinomycin
Macrolides
• Ketolide
Lincosamides
Miscellaneous agents
• Oxazolidinone
PHARMACOLOGY IN PRACTICE

When taking the drug history of Mrs. Moore, an 85-year-old patient in the outpatient clinic, you note that she has been taking 0.25 mg digoxin, one baby aspirin, and the tetracycline minocycline (Minocin). As you read, think about possible drug interactions.
The drugs in this chapter are antibacterial agents that interfere with the development of protein (synthesis) in the bacterial cell. To make protein, a message is made by messenger RNA (mRNA) that tells the cell how to build amino acids. The message is translated by the ribosomes to make the string of amino acids that becomes a protein. These drugs act on different areas of the cell, interfering with the process of protein synthesis.
This chapter discusses four classes of broad-spectrum antibiotics: the tetracyclines, the aminoglycosides, the macrolides, and the lincosamides. There are a number of newer antibacterial drugs that are a single drug in a class, and these are grouped as miscellaneous drugs. The Summary Drug Table: Antibacterial Drugs That Interfere With Protein Synthesis describes the broad-spectrum antibiotics discussed in this chapter (Fig. 8.1).
TETRACYCLINES
The tetracyclines are a group of antibacterial drugs composed of natural and semisynthetic compounds. They are useful in select infections when the organism shows sensitivity (see Chapter 6) to the tetracyclines, such as cholera, Rocky Mountain spotted fever, and typhus. These drugs are also useful when a patient is allergic to the penicillins or cephalosporins.
Actions
The tetracyclines are bacteriostatic and exert their effect by inhibiting bacterial protein synthesis, which is a process necessary for reproduction of the microorganism. Growing resistance to the drugs is a problem with the tetracyclines. Tigecycline (Tygacil) is the first drug in the glycylcycline class of tetracycline-like drugs that is more bacteria resistant.
Uses
These antibiotics are effective in the treatment of infections caused by a wide range of gram-negative and gram-positive microorganisms. Tetracyclines are used as broad-spectrum antibiotics when penicillin is contraindicated, and also to treat the following infections:
• Rickettsial diseases (Rocky Mountain spotted fever, typhus fever, and tick fevers)
• Intestinal amebiasis
• Some skin and soft tissue infections
• Uncomplicated urethral, endocervical, or rectal infections caused by Chlamydia trachomatis
• Severe acne as an adjunctive treatment
• Infection with Helicobacter pylori in combination with metronidazole and bismuth subsalicylate
Adverse Reactions
Gastrointestinal System Reactions
• Nausea or vomiting
• Diarrhea
• Epigastric distress
• Stomatitis
• Sore throat
Other Reactions
• Skin rashes
• Photosensitivity reaction (demeclocycline seems to cause the most serious photosensitivity reaction, whereas minocycline is least likely to cause this type of reaction)
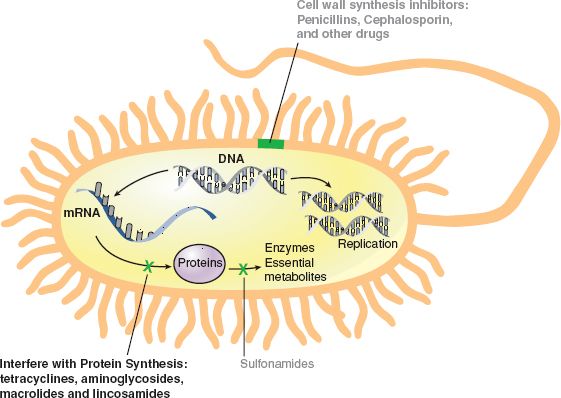
Figure 8.1 Action of bacterial protein synthesis inhibitors such as tetracycline, aminoglycosides, macrolides, and lincosamides.
Contraindications
Tetracyclines are contraindicated in the patient known to be hypersensitive to any of the tetracyclines; during pregnancy, because of the possibility of toxic effects to the developing fetus (pregnancy category D); during lactation; and in children younger than 9 years of age.
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Pediatric
Tetracyclines are not given to children younger than 9 years of age unless their use is absolutely necessary because these drugs may cause permanent yellow-gray-brown discoloration of the teeth. The use of tetracyclines, especially prolonged or repeated therapy, may result in overgrowth of nonsusceptible bacterial or fungal organisms.
Precautions
Tetracyclines should be used cautiously in patients with impaired renal function (when degradation of the tetracyclines occurs, the agents are highly toxic to the kidneys) and those with liver impairment (doses greater than 2 g/day can be extremely damaging to the liver).
 CHRONICCARE CONSIDERATIONS
CHRONICCARE CONSIDERATIONS
Tetracyclines may reduce insulin requirements in patients with diabetes. Blood glucose levels should be monitored frequently during tetracycline therapy.
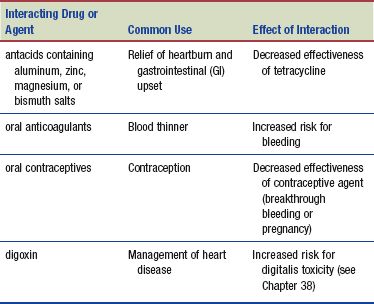
Interactions
The following interactions may occur when a tetracycline is administered with another agent:
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Women
Women of childbearing age should be assessed for oral contraception use whenever tetracyclines are prescribed. The contraception effectiveness is decreased and women should always be taught and feel confident in the use of other forms of birth control during and after tetracycline treatment.
AMINOGLYCOSIDES
The aminoglycosides include amikacin, gentamicin, kanamycin, neomycin, streptomycin, and tobramycin.
Actions
The aminoglycosides exert their bactericidal effect by blocking the ribosome from reading the mRNA, a step in protein synthesis necessary for bacterial multiplication.
Uses
Aminoglycosides are used primarily in the treatment of infections caused by gram-negative microorganisms. In addition, the drugs may be used to reduce bacteria (normal flora) in the bowel when patients are having abdominal surgery or when a patient is in a hepatic coma. Because the oral aminoglycosides are poorly absorbed, they are useful in suppressing GI bacteria. For example, kanamycin and neomycin are used before surgery to reduce intestinal bacteria. It is thought this reduces the possibility of abdominal infection that may occur after surgery on the bowel. This drug treatment protocol is referred to as a portion of the surgical bowel preparation (bowel prep). By destroying bacteria in the gut and washing it out with laxatives or enemas, the surgical area becomes as clean as possible before the operation.
Kanamycin, neomycin, and paromomycin are used orally in the management of hepatic coma. In this disorder, liver failure results in an elevation of blood ammonia levels. By reducing the number of ammonia-forming bacteria in the intestines, blood ammonia levels may be lowered, thereby temporarily reducing some of the symptoms associated with this disorder.
Adverse Reactions
General system reactions include the following:
• Nausea
• Vomiting
• Anorexia
• Rash
• Urticaria
More serious adverse reactions may lead to discontinuation of the drug. These reactions include:
• Nephrotoxicity
• Ototoxicity
• Neurotoxicity
Signs and symptoms of nephrotoxicity may include proteinuria (protein in the urine), hematuria (blood in the urine), an increase in the blood urea nitrogen (BUN) level, a decrease in urine output, and an increase in the serum creatinine concentration. Nephrotoxicity is usually reversible once the drug is discontinued.
Signs and symptoms of ototoxicity include tinnitus (ringing in the ears), dizziness, roaring in the ears, vertigo, and a mild to severe loss of hearing. If hearing loss occurs, it is usually permanent. Ototoxicity may occur during drug therapy or even after therapy is discontinued. The short-term administration of kanamycin and neomycin as a preparation for bowel surgery rarely causes these two adverse reactions.
Signs and symptoms of neurotoxicity include numbness, skin tingling, circumoral (around the mouth) paresthesia, peripheral paresthesia, tremors, muscle twitching, convulsions, muscle weakness, and neuromuscular blockade (acute muscular paralysis and apnea).
The administration of the aminoglycosides may result in a hypersensitivity reaction, which can range from mild to severe and, in some cases, be life-threatening. Mild hypersensitivity reactions may require only discontinuing the drug, whereas the more serious reactions require immediate treatment. When aminoglycosides are given, individual drug references, such as the package insert, should be consulted for more specific adverse reactions. As with other anti-infectives, bacterial or fungal superinfections and pseudomembranous colitis (see Chapter 9) may occur with the use of these drugs.
Contraindications
The aminoglycosides are contraindicated in patients with hypersensitivity to aminoglycosides, pre-existing hearing loss, myasthenia gravis, and parkinsonism. They are also contraindicated during lactation or pregnancy (pregnancy category C, except for neomycin, amikacin, gentamicin, kanamycin, and tobramycin, which are in pregnancy category D). Aminoglycosides are also contraindicated for long-term therapy, because of the potential for ototoxicity and nephrotoxicity.
Precautions
The aminoglycosides are used cautiously in older patients and patients with renal failure (dosage adjustments may be necessary) and neuromuscular disorders.
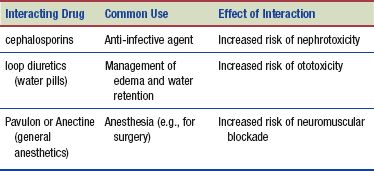
Interactions
The following interactions may occur when an aminoglycoside is administered with another agent:
MACROLIDES
The macrolides are effective against a variety of pathogenic organisms, particularly infections of the respiratory and genitourinary tract.
Actions
The macrolides are bacteriostatic or bactericidal in susceptible bacteria. The drugs act by causing changes in protein function and synthesis.
Uses
These antibiotics are effective as prophylaxis before dental or other procedures in patients allergic to penicillin and in the treatment of:
• A wide range of gram-negative and gram-positive infections
• Acne vulgaris and skin infections
• Upper respiratory infections caused by Haemophilus influenzae (with sulfonamides)
Adverse Reactions
GI reactions include the following:
• Nausea
• Vomiting
• Diarrhea
• Abdominal pain or cramping
As with almost all antibacterial drugs, pseudomembranous colitis may occur, ranging in severity from mild to life threatening. Visual disturbances (associated with telithromycin) may also occur.
Contraindications
These drugs are contraindicated in patients with hypersensitivity to the macrolides and in patients with pre-existing liver disease. Telithromycin (Ketek) should not be ordered if a patient is taking cisapride (Propulsid) or pimozide (Orap).
Precautions
Macrolides should be used cautiously in patients who have liver dysfunction or myasthenia gravis (a disease that affects the myoneural junction in nerves and is manifested by extreme weakness and exhaustion of the muscles) or who are pregnant or lactating (azithromycin and erythromycin are in pregnancy category B; clarithromycin and telithromycin are in pregnancy category C).
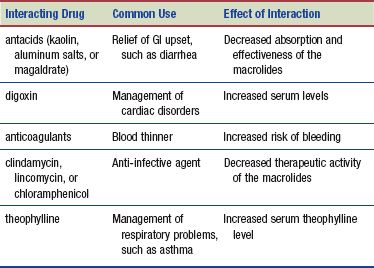
Interactions
The following interactions may occur when a macrolide is administered with another agent:
LINCOSAMIDES
The lincosamides, another group of antibacterial drugs with a high potential for toxicity, are usually used only for treating serious infections in which penicillin or erythromycin (a macrolide) is not effective.
Actions
The lincosamides act by inhibiting protein synthesis in susceptible bacteria, causing cell death. They disrupt the functional ability of the ribosomes (which assemble amino acids in the cell), causing cell death.
Uses
These antibiotics are effective in the treatment of infections caused by a range of gram-negative and gram-positive microorganisms. Lincosamides are used for the more serious infections and may be used in conjunction with other antibiotics.
Adverse Reactions
Gastrointestinal System Reactions
• Abdominal pain
• Esophagitis
• Nausea
• Vomiting
• Diarrhea
Other Reactions
• Skin rash
• Blood dyscrasias
These drugs also can cause pseudomembranous colitis, which may range from mild to very severe. Discontinuing the drug may relieve mild symptoms of pseudomembranous colitis.
Contraindications
The lincosamides are contraindicated in infants younger than 1 month of age and in patients:
• Hypersensitive to the lincosamides
• Taking cisapride (Propulsid) or the antipsychotic drug pimozide (Orap)
• With minor bacterial or viral infections
Precautions
These drugs should be used cautiously in patients with a history of GI disorders, renal disease, liver impairment, or myasthenia gravis (lincosamides have neuromuscular blocking action).
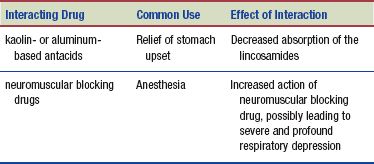
Interactions
The following interactions may occur when a lincosamide is administered with another agent:
MISCELLANEOUS DRUGS INHIBITING PROTEIN SYNTHESIS
Actions
These drugs are unique and individually in their own classes, yet they all interfere with protein synthesis in the bacterial cell. Daptomycin is a member of a new category of antibacterial agents called cyclic lipopeptides. Linezolid (Zyvox) is the first drug in a new drug class, the oxazolidinones. Spectinomycin (Trobicin) is chemically related to but different from the aminoglycosides. Quinupristin/dalfopristin has bactericidal action against both methicillin-susceptible and methicillin-resistant staphylococci.
Uses
Daptomycin is used to treat complicated skin and skin structure bacterial infections as well as Staphylococcus aureus infections of the blood. Linezolid is used in the treatment of vancomycin-resistant Enterococcus faecium (VREF), health care–and community-acquired pneumonias, and skin and skin structure infections, including those caused by methicillin-resistant S. aureus (MRSA). Spectinomycin is used for treating gonorrhea in patients who are allergic to penicillins, cephalosporins, or probenecid. Quinupristin/ dalfopristin is a bacteriostatic agent also used in the treatment of VREF.
Adverse Reactions
The most common adverse reactions include the following:
• Nausea
• Vomiting
• Diarrhea or constipation
• Headache and dizziness
• Insomnia
• Rash
• Chills
Less common adverse reactions include:
• Fatigue
• Depression
• Nervousness
• Photosensitivity
Pseudomembranous colitis and thrombocytopenia are the most serious adverse reactions caused by linezolid.
 NURSING ALERT
NURSING ALERT
Quinupristin/dalfopristin is irritating to the vein. After peripheral infusion, the vein should be flushed with 5% dextrose in water (D5W), because the drug is incompatible with saline or heparin flush solutions.
Contraindications and Precautions
Linezolid is contraindicated in patients who are allergic to the drug or who are pregnant (pregnancy category C) or lactating and in patients with phenylketonuria (PKU). Daptomycin, spectinomycin, and quinupristin/dalfopristin are contraindicated in patients with a known hypersensitivity to the drug, and it should not be used during pregnancy (pregnancy category B) or lactation.
Linezolid is used cautiously in patients with bone marrow depression, hepatic dysfunction, renal impairment, hypertension, and hyperthyroidism. If another sexually transmitted infection (STI) is present with gonorrhea, anti-infectives (in addition to spectinomycin) may be needed to eradicate the infectious processes. Because prolonged use of anti-infectives can disrupt normal flora, the patient should be monitored for secondary bacterial or fungal infections.
Interactions
The following interactions may occur when linezolid is administered with another agent:
• Antiplatelet drugs (aspirin or the nonsteroidal anti inflammatory drugs [NSAIDs])—increased risk of bleeding and thrombocytopenia
• Monamine oxidase inhibitor (MAOI) antidepressants—decreased effectiveness
• Large amounts of food containing tyramine (e.g., aged cheese, caffeinated beverages, yogurt, chocolate, red wine, beer, pepperoni)—risk of severe hypertension
Myopathy with elevated creatine phosphokinase (CPK) levels may occur if daptomycin is administered with statin drugs (cholesterol reduction). No significant drug or food interactions for spectinomycin are known. Daptomycin should be used cautiously in patients taking warfarin (Coumadin). When taking quinupristin/dalfopristin, the serum levels of the following drugs may increase: antiretrovirals, antineoplastic and immunosuppressant agents, calcium channel blockers, benzodiazepines, and cisapride.
NURSING PROCESS
PATIENT RECEIVING AN ANTIBACTERIAL INTERFERING WITH PROTEIN SYNTHESIS
ASSESSMENT
Preadministration Assessment
It is important to establish an accurate database before the administration of any antibiotic. Identify and record signs and symptoms of the infection. Signs and symptoms may vary and often depend on the organ or system involved and whether the infection is external or internal. Examples of some of the signs and symptoms of an infection in various areas of the body are pain, drainage, redness, changes in the appearance of sputum, general malaise, chills and fever, cough, and swelling.
Obtain a thorough allergy history, especially a history of drug allergies. Some antibiotics have a higher incidence of hypersensitivity reactions in those with a history of allergy to drugs or other substances. If the patient has a history of drug allergies and has not told the primary health care provider, do not administer the first dose of the drug; instead, immediately contact the primary health care provider to discuss the allergy history.
The primary health care provider may order culture and sensitivity tests, which should also be performed before the first dose of the drug is given. Other laboratory tests such as renal and hepatic function tests, complete blood count, and urinalysis may also be ordered by the primary health care provider. In persons with impaired hearing or at risk for hearing loss, a hearing test may be recommended.
When kanamycin or neomycin is given to a patient with altered consciousness for hepatic coma, evaluate the patient’s ability to follow directions and to swallow.
Ongoing Assessment
An ongoing assessment is important during therapy with antibacterials that interfere with protein synthesis. Take vital signs every 4 hours or as ordered by the primary health care provider. Notify the primary health care provider if there are changes in the vital signs, such as a significant drop in blood pressure, an increase in the pulse or respiratory rate, or a sudden increase in temperature. When an aminoglycoside is being administered, it is important to monitor the patient’s respiratory rate because neuromuscular blockade has been reported with the administration of these drugs. Report any changes in the respiratory rate or rhythm to the primary health care provider because immediate treatment may be necessary. When kanamycin or neomycin is given for hepatic coma, assess and record the patient’s general condition and changes in mentation daily.
Each day, compare current signs and symptoms of the infection against the initial signs and symptoms and record any specific findings in the patient’s chart.
When an antibiotic is ordered for prevention of a secondary infection (prophylaxis), observe the patient for signs and symptoms that may indicate the beginning of an infection despite the prophylactic use of the antibiotic. If signs and symptoms of an infection occur, report them to the primary health care provider.
NURSING DIAGNOSES
Drug-specific nursing diagnoses include the following:
 Impaired Comfort: Increased Fever related to ineffectiveness of anti-infective therapy
Impaired Comfort: Increased Fever related to ineffectiveness of anti-infective therapy
 Acute Confusion related to increased ammonia blood levels
Acute Confusion related to increased ammonia blood levels
 Ineffective Tissue Perfusion: Renal related to adverse drug reactions to aminoglycosides
Ineffective Tissue Perfusion: Renal related to adverse drug reactions to aminoglycosides
 Risk for Injury related to visual disturbances from telithromycin treatment, paresthesia secondary to neurotoxicity, or auditory damage from aminoglycosides
Risk for Injury related to visual disturbances from telithromycin treatment, paresthesia secondary to neurotoxicity, or auditory damage from aminoglycosides
 Diarrhea related to superinfection secondary to anti infective therapy, adverse drug reaction
Diarrhea related to superinfection secondary to anti infective therapy, adverse drug reaction
Nursing diagnoses related to drug administration are discussed in Chapter 4.
PLANNING
The expected outcomes for the patient may include an optimal response to therapy, which includes control of the infectious process or prophylaxis of bacterial infection, meeting of patient needs related to the management of adverse drug effects, and confidence in an understanding of the medication regimen.
IMPLEMENTATION
Promoting an Optimal Response to Therapy
These drugs are of no value in the treatment of infections caused by a virus or fungus. There may be times when a secondary bacterial infection has occurred or may occur when the patient has a fungal or viral infection. The primary health care provider may then order one of the broad-spectrum antibiotics, but its purpose is for preventing (prophylaxis) or treating a secondary bacterial infection that could potentially develop after the primary fungal or viral infection.
ORAL ADMINISTRATION. Adverse reactions to most anti-infective drugs include nausea, vomiting, or abdominal pain. Patients may want to eat foods when these drugs are administered to reduce GI problems. It is important for you to know how medications will be affected if taken with foods.
Tetracyclines. It is important to give tetracyclines on an empty stomach. The exceptions are minocycline (Minocin) and tigecycline (Tygacil), which may be taken with food. All tetracyclines should be given with a full glass of water (8 ounces).
 NURSING ALERT
NURSING ALERT
Do not give tetracyclines along with dairy products (milk or cheese), antacids, laxatives, or products containing iron. When the aforementioned drugs are prescribed, make sure they are given 2 hours before or after the administration of a tetracycline. Food or drugs containing calcium, magnesium, aluminum, or iron prevent the absorption of the tetracyclines if ingested concurrently.
Aminoglycosides. When kanamycin or neomycin is given to suppress intestinal bacteria before surgery, the primary health care provider’s orders regarding the timing of the administration of the drug are extremely important. Omission of a dose or failure to give the drug at the specified time may result in inadequate suppression of intestinal bacteria. When neomycin is given, enteric-coated erythromycin may be given at the same time as part of surgical bowel preparation. Enteric-coated tablets have a special coating that prevents the drug from being absorbed in the stomach. Absorption takes place lower in the GI tract after the coating has dissolved.
Macrolides. Clarithromycin, fidaxomicin, and telithromycin may be taken without regard to meals, and clarithromycin may be taken with milk if desired. Azithromycin is given 1 hour or more before a meal or 2 hours or more after a meal. Erythromycin is given on an empty stomach (1 hour before or 2 hours after meals) and with 180 to 240 mL of water.
Lincosamides. Food impairs the absorption of lincomycin. The patient should take nothing by mouth (except water) for 1 to 2 hours before and after taking lincomycin. Clindamycin may be taken with food or a full glass of water.
PARENTERAL ADMINISTRATION. When these drugs are given intramuscularly, inspect previous injection sites for signs of pain or tenderness, redness, and swelling. Some antibiotics may cause temporary local reactions, but persistence of a localized reaction should be reported to the primary health care provider. It is important to rotate injection sites and record the site used for injection in the patient’s chart.
When these drugs are given intravenously (IV), inspect the needle site and area around the needle site for signs of extravasation of the IV fluid or signs of tenderness, pain, and redness (which may indicate phlebitis or thrombophlebitis). If these symptoms are apparent, restart the IV in another vein and bring the problem to the attention of the primary health care provider.
Monitoring and Managing Patient Needs
Observe the patient at frequent intervals, especially during the first 48 hours of therapy. It is important to report to the primary health care provider the occurrence of any adverse reaction before the next dose of the drug is due.
 NURSING ALERT
NURSING ALERT
Always report serious adverse reactions, such as a severe hypersensitivity reaction, respiratory difficulty, severe diarrhea, or a decided drop in blood pressure, to the primary health care provider immediately, because a serious adverse reaction may require emergency intervention.
IMPAIRED COMFORT: INCREASED FEVER. Monitor the temperature at frequent intervals, usually every 4 hours unless the patient has an elevated temperature. When the patient has an elevated temperature, check the temperature, pulse, and respirations every hour until the temperature returns to normal, and administer an antipyretic medication if prescribed by the primary health care provider.
ACUTE CONFUSION: HEPATIC COMA. Exercise care when the aminoglycosides kanamycin and neomycin are administered orally as treatment for hepatic coma. During the early stages of this disorder, various changes in the level of consciousness may be seen. At times, the patient may appear lethargic and respond poorly to commands. Because of these changes in the level of consciousness, the patient may have difficulty swallowing, and a danger of aspiration is present. If the patient appears to have difficulty taking an oral drug, withhold the drug and contact the primary health care provider.
INEFFECTIVE TISSUE PERFUSION: RENAL. The patient taking an aminoglycoside is at risk for nephrotoxicity. Measure and record the intake and output and notify the primary health care provider if the output is less than 750 mL/day. It is important to keep a record of the fluid intake and output as well as the patient’s daily weight to assess hydration and renal function. Encourage fluid intake to 2000 mL/day (if the patient’s condition permits). Any changes in the intake–output ratio or in the appearance of the urine may indicate nephrotoxicity. Report these types of changes to the primary health care provider promptly. In turn, the primary health care provider may order daily laboratory tests (e.g., serum creatinine and BUN) to monitor renal function. Report elevations in the creatinine or BUN level to the primary health care provider because elevation may indicate renal dysfunction.
RISK FOR INJURY. Telithromycin (Ketek), a drug related to the macrolides, can cause the patient’s eyes to have difficulty focusing and accommodating to light. Patients should be cautioned regarding the potential for accidents and injury when driving, operating machinery, or engaging in other hazardous activities.
Be alert for symptoms such as numbness or tingling of the skin, circumoral paresthesia, peripheral paresthesia (numbness or tingling in the extremities), tremors, and muscle twitching or weakness. The nurse reports any symptom of neurotoxicity immediately to the primary health care provider. Convulsions can occur if the drug is not discontinued.
 NURSING ALERT
NURSING ALERT
Neuromuscular blockade or respiratory paralysis may occur after administration of the aminoglycosides. Therefore, it is extremely important that any symptoms of respiratory difficulty be reported immediately. If neuromuscular blockade occurs, it may be reversed by the administration of calcium salts, but mechanical ventilation may be required.
The patient taking a prolonged course of aminoglycosides is at risk for ototoxicity. Instruct the patient to report any ringing in the ears, difficulty hearing, or dizziness to the primary health care provider. Changes in hearing may not be noticed initially by the patient, but when changes occur they usually progress from difficulty in hearing high-pitched sounds to problems hearing low-pitched sounds. Auditory changes are irreversible, usually bilateral, and may be partial or total. The risk is greater in patients with renal impairment or those with pre-existing hearing loss.
 NURSING ALERT
NURSING ALERT
To detect ototoxicity, carefully evaluate the patient’s complaints or comments related to hearing, such as a ringing or buzzing in the ears. The patient may report a sensation of stuffiness in the ears or difficulty hearing. If hearing problems do occur, report this problem to the primary health care provider immediately. To monitor for damage to the eighth cranial nerve, an evaluation of hearing may be done by audiometry before and throughout the course of therapy.
DIARRHEA. Diarrhea may be an indication of a superinfection or pseudomembranous colitis, both of which can be serious. Inspect all stools for blood or mucus. If diarrhea is dark or there is mucus in the stool, save a sample and test for occult blood using a test such as Hemoccult. If the stool tests positive for blood, save a sample of the stool for possible further laboratory analysis.
Encourage the patient to drink fluids to replace those lost with the diarrhea. It is also important to maintain an accurate intake and output record to help determine fluid balance.
Observe the patient for other signs and symptoms of a bacterial or fungal superinfection, such as vaginal or anal itching, sores in the mouth, diarrhea, fever, chills, and sore throat. It is important to report any new signs and symptoms occurring during antibiotic therapy to the primary health care provider, who determines if these problems are part of the original infection or if a superinfection is occurring.
Educating the Patient and Family
The patient and family should feel confident in their understanding of the prescribed drug regimen. It is not uncommon for patients to stop taking a prescribed drug because they feel better. A detailed plan of teaching helps to reduce the incidence of this problem.
Use principles to support health literacy and easy-to-understand terms when teaching about the adverse reactions associated with the specific prescribed antibiotic. Advise the patient to contact the primary health care provider if any potentially serious adverse reactions, such as hypersensitivity reactions, moderate to severe diarrhea, sudden onset of chills and fever, sore throat, or sores in the mouth, occur.
Develop a teaching plan that includes the following information:
 Take the drug at the prescribed time intervals. These intervals are important because a certain amount of the drug must be in the body at all times for the infection to be controlled.
Take the drug at the prescribed time intervals. These intervals are important because a certain amount of the drug must be in the body at all times for the infection to be controlled.
 Do not increase or omit the dose unless advised to do so by the primary health care provider.
Do not increase or omit the dose unless advised to do so by the primary health care provider.
 Complete the entire course of treatment. Never stop the drug, except on the advice of a primary health care provider, before the course of treatment is completed even if symptoms improve or disappear. Failure to complete the prescribed course of treatment may result in a return of the infection.
Complete the entire course of treatment. Never stop the drug, except on the advice of a primary health care provider, before the course of treatment is completed even if symptoms improve or disappear. Failure to complete the prescribed course of treatment may result in a return of the infection.
 Take each dose with a full (8-ounce) glass of water. Follow the directions given by the clinical pharmacist regarding taking the drug on an empty stomach or with food (see Patient Teaching for Improved Patient Outcomes: Avoiding Drug–Food Interactions).
Take each dose with a full (8-ounce) glass of water. Follow the directions given by the clinical pharmacist regarding taking the drug on an empty stomach or with food (see Patient Teaching for Improved Patient Outcomes: Avoiding Drug–Food Interactions).
 Notify the primary health care provider if symptoms of the infection become worse or there is no improvement in the original symptoms after about 5 days.
Notify the primary health care provider if symptoms of the infection become worse or there is no improvement in the original symptoms after about 5 days.
 When a tetracycline has been prescribed, avoid exposure to the sun or any type of tanning lamp or bed. When exposure to direct sunlight is unavoidable, completely cover the arms and legs and wear a wide-brimmed hat to protect the face and neck. Application of a sunscreen may or may not be effective. Therefore, consult the primary health care provider before using a sunscreen to prevent a photosensitivity reaction.
When a tetracycline has been prescribed, avoid exposure to the sun or any type of tanning lamp or bed. When exposure to direct sunlight is unavoidable, completely cover the arms and legs and wear a wide-brimmed hat to protect the face and neck. Application of a sunscreen may or may not be effective. Therefore, consult the primary health care provider before using a sunscreen to prevent a photosensitivity reaction.
EVALUATION
 Therapeutic response is achieved, and there is no evidence of infection.
Therapeutic response is achieved, and there is no evidence of infection.
 Adverse reactions are identified, reported to the primary health care provider, and managed successfully with appropriate nursing interventions:
Adverse reactions are identified, reported to the primary health care provider, and managed successfully with appropriate nursing interventions:
• Patient reports comfort without fever.
• Orientation and mentation remain intact.
• Patient has adequate renal tissue perfusion.
• No evidence of injury is seen due to visual or auditory disturbances.
• Patient does not experience diarrhea.
 Patient and family express confidence and demonstrate an understanding of the drug regimen.
Patient and family express confidence and demonstrate an understanding of the drug regimen.
PHARMACOLOGY IN PRACTICE
THINKING CRITICALLY
 Based on your knowledge of the tetracyclines, determine whether there is any reason to be concerned about Mrs. Moore’s drug regimen. Given her confusion, how will you teach her about potential interactions of the drugs?
Based on your knowledge of the tetracyclines, determine whether there is any reason to be concerned about Mrs. Moore’s drug regimen. Given her confusion, how will you teach her about potential interactions of the drugs?
Patient Teaching for Improved Patient Outcomes
Avoiding Drug–Food Interactions
When you teach, make sure your patient understands the following:
✓ Drugs may be taken with food or milk to minimize the risk for GI upset. However, most tetracyclines, when given with foods containing calcium, such as dairy products, are not absorbed as well as when they are taken on an empty stomach. So, if the patient is to receive tetracycline at home, it is important to be sure he or she knows to take the drug on an empty stomach, 1 hour before or 2 hours after a meal.
✓ Demonstrate to the patient how to read labels in the grocery store and to beware of items (e.g., cereals) that may be fortified with calcium.
✓ In addition, teach the patient to avoid the following dairy products before or after taking tetracycline:
 Milk (whole, low fat, skim, condensed, or evaporated) and milkshakes
Milk (whole, low fat, skim, condensed, or evaporated) and milkshakes
 Cream (half-and-half, heavy, light), sour cream, coffee creamers, and creamy salad dressings
Cream (half-and-half, heavy, light), sour cream, coffee creamers, and creamy salad dressings
 Eggnog
Eggnog
 Cheese (natural and processed) and cottage cheese
Cheese (natural and processed) and cottage cheese
 Yogurt and frozen yogurt
Yogurt and frozen yogurt
 Ice cream, ice milk, and frozen custard
Ice cream, ice milk, and frozen custard
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


