DRUG CLASSES
Urinary anti-infectives
Urinary analgesics
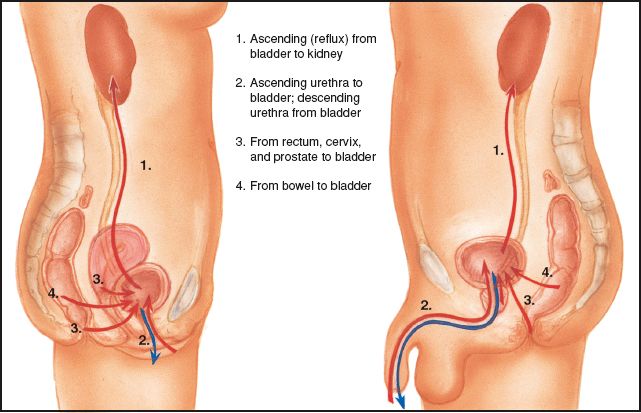
This chapter discusses drugs used to treat urinary tract infections (UTIs). These types of infections are caused by pathogenic microorganisms of one or more structures of the urinary tract (Fig. 48.1). Because the female urethra is considerably shorter than the male urethra, women are affected by UTIs much more frequently than men. The most common structure affected is the bladder. Clinical manifestations of a UTI of the bladder (cystitis) include urgency, frequency, pressure, burning and pain on urination, and pain caused by spasm in the region of the bladder and the suprapubic area. With chronic UTIs, the urethra, prostate (prostatitis), and kidney (pyelonephritis) may also be affected.
The drugs discussed in this chapter are anti-infectives. They are used in the treatment of UTIs, and they have an effect on bacteria in the urinary tract. Although administered systemically, that is, by the oral or parenteral routes, they do not achieve significant levels in the bloodstream and are of no value in treating systemic infections. They are primarily excreted by the kidneys and exert their major antibacterial effects in the urine as it travels through the bladder.
Some drugs used in the treatment of UTIs, such as nitrofurantoin, do not belong to the antibiotic or sulfonamide groups of drugs. Examples of the most common drugs used in treating UTIs include amoxicillin (broad-spectrum penicillins; see Chapter 7), trimethoprim (sulfonamides; see Chapter 6), and nitrofurantoin. The anti-infective drugs known as fluoroquinolones (see Chapter 9) were initially approved for UTI treatment, but have become of greater use in systemic infection treatment. Combination drugs such as trimethoprim and sulfamethoxazole (Bactrim or Septra) are also used. The Summary Drug Table: Urinary Tract Anti-Infectives gives examples of the drugs used for UTIs.
Another drug frequently used to treat UTIs is phenazopyridine (Pyridium), a urinary analgesic, used to relieve discomfort associated with UTIs.
PHARMACOLOGY IN PRACTICE

Janna Wong is a 16-year-old high school gymnast. She is at the clinic for a routine physical. Vital signs show that Janna has a fever of 100.5°F. She says she feels tired, yet is fidgety. When asked if she would like some water, Janna says no because she does not want to urinate until she gets home. Think about her remarks as you read this chapter.
Figure 48.1 Routes of infection in the urinary tract.
Actions and Uses
These drugs are used for UTIs that are caused by susceptible bacterial microorganisms. Many of the anti-infective drugs used for treating UTIs are chosen because of the rapid excretion rate of the drugs rather than the way they act inside the body. As a result, these anti-infectives have a high concentration in the urine and appear to act by interfering with bacterial multiplication in the urine. Nitrofurantoin (Macrodantin) may be bacteriostatic (slows or retards the multiplication of bacteria) or bactericidal (destroys bacteria), depending on the concentration of the drug in the urine. See the specific anti-infective chapters for the manner in which other anti-infective drugs work.
Phenazopyridine is a dye that exerts a topical analgesic effect on the lining of the urinary tract. It does not have anti-infective activity. Phenazopyridine is available as a separate drug but is also included in some urinary tract anti-infective combination drugs.
Adverse Reactions
Adverse reactions are primarily gastrointestinal (GI) disturbances and include the following:
• Anorexia, nausea, vomiting, and diarrhea
• Abdominal pain or stomatitis
Other generalized body system reactions include:
• Drowsiness, dizziness, headache, blurred vision, weakness, and peripheral neuropathy
• Rash, pruritus, photosensitivity reactions, and leg cramps
When these drugs are given in large doses, patients may experience burning on urination and bladder irritation; this should not be mistaken for a continued infection. Nitrofurantoin has been known to cause acute and chronic pulmonary reactions. Patients should be told that phenazopyridine will discolor the urine (dark orange to brown) and permanently stain undergarments that come in contact with the urine.
Contraindications and Precautions
Anti-infectives are contraindicated in patients with a hypersensitivity to the drugs and during pregnancy (pregnancy category C) and lactation. One exception is nitrofurantoin, which is classified as a pregnancy category B drug and is used with caution during pregnancy.
The anti-infectives should be used cautiously in those with renal or hepatic impairment. Patients who are allergic to tartrazine (a food dye) should not take methenamine (Hiprex). This drug is used cautiously in patients with gout, because it may cause crystals to form in the urine. Nitrofurantoin is used cautiously in patients with cerebral arteriosclerosis, diabetes, or a glucose-6-phosphate dehydrogenase (G6PD) deficiency.
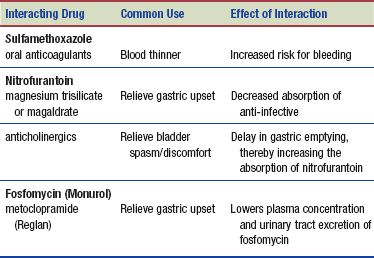
Interactions
Anti-Infectives
The following interactions may occur when a specific urinary anti-infective is administered with another agent:
An increased urinary pH (alkaline urine) decreases the effectiveness of methenamine. Therefore, to avoid raising the urine pH when taking methenamine, the patient should not use antacids containing sodium bicarbonate or sodium carbonate.
 HERBAL CONSIDERATIONS
HERBAL CONSIDERATIONS
Cranberry juice has long been recommended for use in treating and preventing UTIs. Clinical studies have confirmed that cranberry juice is beneficial to individuals with frequent UTIs. Cranberry juice inhibits bacteria from attaching to the walls of the urinary tract and prevents certain bacteria from forming dental plaque in the mouth. Cranberry juice is safe for use as a food and for urinary tract health. Cranberry juice and capsules have no contraindications, no known adverse reactions, and no drug interactions. The recommended dosage is 9 to 15 capsules a day (400 to 500 mg/day) or 4 to 8 ounces of juice daily (Brown, 2012).
NURSING PROCESS
PATIENT TEACHING FOR MEDICATION INFORMATION
ASSESSMENT
Preadministration Assessment
When a UTI has been diagnosed, urine culture and sensitivity tests are performed to determine bacterial sensitivity to the drugs (antibiotics and urinary tract anti-infectives) that will control the infection. Ask the patient about symptoms of the infection before instituting therapy. Document a description of the urine including the color (clear, straw, or amber) and the appearance (clear or cloudy). Typically you will check for fever by taking the vital signs and may perform a urine check for blood or protein.
Document the subjective symptoms the patient is experiencing to provide a baseline for future assessment. Record the patient’s complaints of pain, urinary frequency, bladder distension, and other symptoms associated with the urinary system.
Ongoing Assessment
Many UTIs are treated on an outpatient basis because hospitalization is seldom required. UTIs may affect the hospitalized patient or nursing home resident with an indwelling urethral catheter or a disorder such as a stone in the urinary tract. The primary nursing intervention to prevent UTIs in the hospitalized patient is good hand hygiene (handwashing).
When caring for a hospitalized patient with a UTI, monitor the vital signs every 4 hours or as ordered by the primary health care provider. Any significant rise in body temperature is reported to the primary health care provider, because intervention to reduce the fever or culture and sensitivity tests may need to be repeated.
If after several days the symptoms of the UTI do not improve or they become worse, contact the primary health care provider as soon as possible. Periodic urinalysis and urine culture and sensitivity tests may be ordered to monitor the effects of drug therapy.
NURSING DIAGNOSES
Drug-specific nursing diagnoses include the following:
 Impaired Urinary Elimination related to discomfort of urinary tract infection
Impaired Urinary Elimination related to discomfort of urinary tract infection
 Ineffective Breathing Pattern related to adverse reaction to drug
Ineffective Breathing Pattern related to adverse reaction to drug
Nursing diagnoses related to drug administration are discussed in Chapter 4.
PLANNING
The expected outcomes for the patient may include an optimal response to drug therapy, support of patient needs related to the management of adverse reactions, and confidence in an understanding of the medication regimen.
IMPLEMENTATION
Promoting an Optimal Response to Therapy
To promote an optimal response to therapy, give urinary tract anti-infectives with food to prevent GI upset. Nitrofurantoin especially should be given with food, meals, or milk, because this drug is particularly irritating to the stomach. Fosfomycin (Monurol) has special administration requirements; it comes in a 3-gram, one-dose packet that must be dissolved in 90 to 120 mL of water (not hot water). Administer the drug immediately after dissolving it in water. Phenazopyridine is administered after meals to prevent GI upset.
 NURSING ALERT
NURSING ALERT
Phenazopyridine is not administered for more than 2 days when used in combination with an antibacterial drug to treat a UTI. When used for more than 2 days, the drug may mask the symptoms of a more serious disorder.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree