(1)
Department of Pathology, Rutgers-New Jersey Medical School, Newark, NJ, USA
Keywords
CircumvallateCircummarginateBilobed placentaSuccenturiate lobeBattledore placentaMeconiumAcute chorioamnionitisSingle umbilical arteryVelamentous cord insertionVasa previaTrue knots of cordFalse knots in cordAbruptionInfarctIntervillous thrombiFetal inflammatory responseCandida funisitisDecidual vasculopathyAtherosisChorangiosisChorangiomaChorangiomatosisVillous malperfusionMultiple pregnancyChronic histiocytic intervillositisIncreased perivillous fibrinMaternal floor infarctionVillitis of unknown etiologyTwin placentaAmnion nodosumMeconium myonecrosisIncreased syncytial knots12.1 Abnormalities and the Approach to Examination of the Placenta
The placenta can have numerous abnormalities, both gross and microscopic. The placenta may explain a poor pregnancy outcome, including growth restriction or stillbirth, and may provide information about future pregnancy risk. For many lesions, however, there is not a one to one correlation between the presence of a specific lesion and a negative fetal outcome. Epidemiologically, however, many of these lesions or groups of lesions are associated with poor outcomes (Table 12.1).
Table 12.1
Key points about placental pathology
There are large numbers of lesions. Lesions don’t always correspond directly with poor outcome, but may be epidemiologically associated with poor outcomes |
Placental lesions can be separated into categories (infectious, ischemic, immune) to better evaluate the process associated with a poor outcome |
Abruption may not always be detectible on pathology, and the gold standard for diagnosis is clinical |
Candida funisitis warrants a phone call to the clinician due to possible associated fetal candidal sepsis |
Examination of the placenta begins with a gross examination in the delivery room. The delivering provider may detect abnormalities that indicate that the placenta should be sent to the Pathology Laboratory. Some institutions send all placentas to Pathology; however, some reserve the evaluation for specific risk categories, which can be categorized as maternal, fetal, or placental issues.
On receipt of a placenta by the Pathology laboratory, a thorough gross examination is performed. Of note, by convention, placental weight is assessed after removal of the umbilical cord and membranes. A gross description is provided in the report, and then sections are selected, as with other pathology specimens. One way to think of the histopathologic evaluation of placentas is to remember to consider all the components; cord, membranes, villi, and decidua. There are many textbooks on placental pathology, which is an extensive topic. This short summary of some of the most concerning lesions will hopefully assist clinicians in interpreting their pathology reports.
12.2 Gross Placental Abnormalities
12.2.1 Abnormalities of Placental Shape
The first part of placental evaluation is gross inspection of the placenta. Abnormal shapes may reflect a variety of genetic or mechanical issues. A circumvallate placenta (Fig. 12.1a) is thought to be secondary to chronic marginal abruption lifting up the peripheral membranes, with folding over of the membranes upon themselves. The fold in the membranes inserts internal to the edge of the placental disk. Circumvallation may be partial or circumferential. There is some association with preterm labor and abruption according to some authors [1]; however, the clinical significance is unclear [2]. Circummarginate placentas show a similar ridge of fibrin internal to the placental edge (Fig. 12.1b) on the fetal surface, but the placental membranes have not folded upon themselves. These lesions are not thought to be significant clinically in most cases.
Fig. 12.1
Circumvallate placenta has folding over of the membranes, which then insert proximal to the placental edge (a right), while in circummarginate placenta, there is a ridge of fibrin; however, there is no folding of the membranes, which also insert proximal to the placental edge (a left, b)
Bilobed placentas consist of two lobes of fairly equal size (Fig. 12.2). Intervening vessels may be vulnerable to trauma. In succenturiate lobe, one lobe is smaller. The danger here is thinking the placenta is complete at delivery, with risk of postpartum hemorrhage from unsuspected retained placental tissue.
Fig. 12.2
Accessory lobes. If equal, the placenta is bilobed
12.2.2 Abnormalities of the Membranes
Gross examination of the membranes may provide a clue to underlying pathology. Meconium staining, if recent and heavy, is a pea soup green color. Histologically, meconium may denude the amniotic epithelium entirely or may show as pigmented macrophages in the membranes (Fig. 12.3a). The timing of meconium spread from amnion to chorion to decidua is not reliable. The presence of meconium in and of itself does not have major clinical significance and is very common. However, meconium may cause vasospasm, which can cause fetal hypoxic stress (not discernable on histopathology), and if the placenta is exposed to prolonged meconium, myonecrosis of the vessels of the cord and chorionic plate may occur (Fig. 12.3b), significantly associated with fetal compromise.
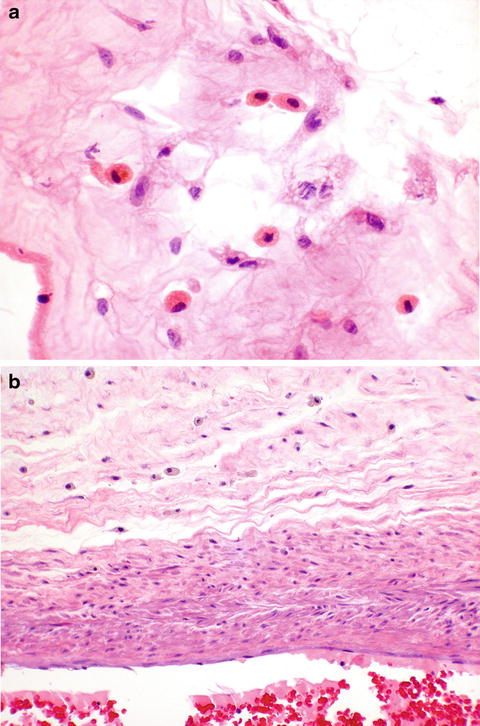
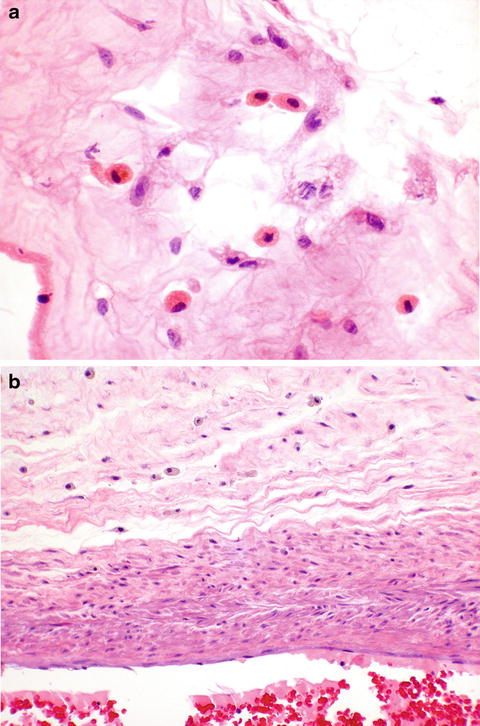
Fig. 12.3
Meconium. Meconium macrophages are seen in the membranes (a), as well as in the cord, where vascular myonecrosis is also seen adjacent in the vessel (b)
Acute chorioamnionitis, if severe, may turn yellow, or membranes may opacify the membranes. Opaque membranes may also simply indicate a larger amount of adherent decidua to the membranes. For the histology of acute chorioamnionitis, see below section on infectious lesions.
Amnion nodosum may be seen as multiple small white nodules on the placental membranes and fetal surface. Amnion nodosum is comprised of clusters of fetal squamous cells and lanugo hairs that become adherent to the amnion, sometimes with amnion epithelium overgrowing, in cases of severe oligohydramnios (Fig. 12.4).
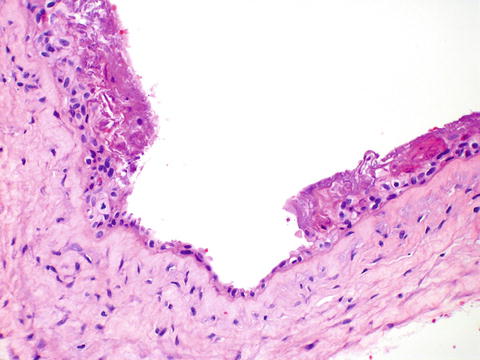
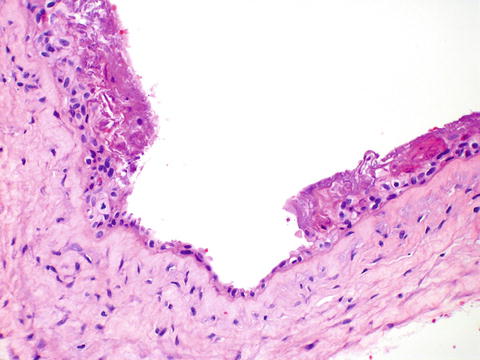
Fig. 12.4
Amnion nodosum. Numerous squames are adherent to the membranes
12.2.3 Abnormalities of the Cord
Many of the abnormalities of the umbilical cord are gross rather than microscopic diagnoses. Abnormal insertions, including velamentous insertion into the membranes, and battledore, which is marginal insertion into the disk, should be noted. Velamentous insertions are important because the exposed vessels are subject to trauma, which can compromise the fetus, as well as rupture, particularly if there is vasa previa. This can lead to fetal exsanguination. There may be increased twisting of the cord, with torsion along the length, or with stricture focally (Fig. 12.5). Hematomas of the cord are often iatrogenic, occurring during traction during the third stage of labor. However, if spontaneous, they may compress the fetal vessels and cause compromise (Fig. 12.6). Single umbilical artery can be recognized both grossly and microscopically. It is the most common placental anomaly. It is sometimes associated with abnormalities in the fetus, particularly genitourinary. True knots are common and are only significant if there is obstruction. This can be concluded from congestion of the cord on one side, or thrombi. False knots are varicosities due to the vessels being longer than the cord and are of no clinical significance.




