(1)
Department of Pathology, Rutgers-New Jersey Medical School, Newark, NJ, USA
Keywords
Cellular pseudosarcomatous fibroepithelial stromal polyp of the vaginaArias-Stella reactionSpontaneous abortionPregnancy-related changes in leiomyomataPlacenta acretaPlacenta incretaPlacenta percretaCouvelaire uterusSubinvolution, uterusRetained placentaPseudoneoplastic ovarian lesions: luteoma of pregnancy, hyperreactio luteinalis, large solitary luteinized follicle cyst of pregnancy and puerperium11.1 Lesims of the Female Genital Tract Related to Pregnancy
The hormonal milieu associated with pregnancy is the background for a unique group of genital tract lesions, many of which regress after the hormonal stimulus is removed. It is important to be familiar with these lesions to avoid overinterpretation of their clinical significance (Table 11.1).
Table 11.1
Key points about pregnancy-associated pathology
Vaginal fibroepithelial stromal polyps may look highly atypical in pregnancy, and these should not be mistaken for malignancy |
Luteoma, hyperreactio luteinalis, and large solitary luteinized follicle cyst of pregnancy and puerperium are hyperplastic, not neoplastic processes |
Uterine subinvolution shows histopathologic evidence of lack of involution of spiral arterioles of the implantation site |
Arias-Stella reaction can be seen with pregnancy at any site, not just tubal ectopic pregnancy |
If evaluating to confirm a spontaneous abortion, if villi aren’t present, the implantation site with associated implantational trophoblasts should be sought |
11.2 Vulvo-Vaginal Lesions Associated with Pregnancy
11.2.1 Cellular Pseudosarcomatous Fibroepithelial Stromal Polyp of the Vulva and Vagina
Although fibroepithelial stromal polyps can affect a variety of locations, the genital tract lesions are most likely to be encountered in the vulva and vagina. During pregnancy, the stroma of these lesions may show increased cellularity (Fig. 11.1a), increased mitotic activity, atypical mitoses, and cytologic atypia (Fig. 11.1b). Awareness of this effect is important to avoid overdiagnosing these lesions as sarcomas. The lesion most likely to be confused with these hormonally stimulated polyps, sarcoma botryoides (embryonal rhabdomyosarcoma), occurs most often in children, rather than reproductive-aged women. True sarcoma botryoides stains for muscle markers, which are not present in fibroepithelial stromal polyps. Unlike the cambium layer of increased cellularity under the epithelium seen in sarcoma botryoides, cellular pseudosarcomatous fibroepithelial stromal polyps tend to be more cellular in the center [1].
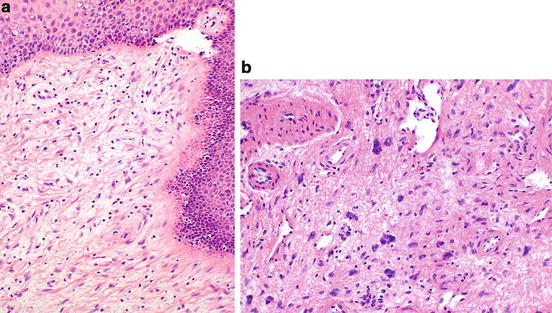
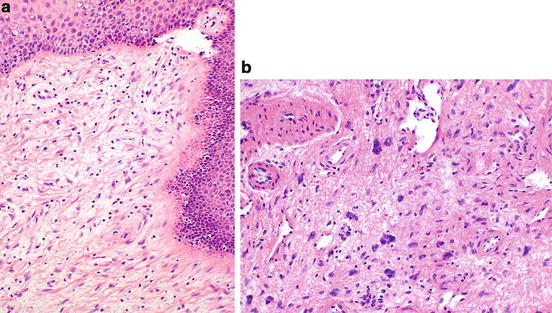
Fig. 11.1
Vaginal fibroepithelial stromal polyp. This polyp shows increased cellularity (a), with stellate cells extending to under the overlying epithelium. Additional findings that may be seen in pregnancy include nuclear atypia (b), mitoses, and atypical mitotic figures (not shown)
11.3 Uterine Lesions Associated with Pregnancy
11.3.1 Arias-Stella Reaction
The Arias-Stella reaction, named after the pathologist who first described it [2], is a pattern of exaggerated hypersecretory endometrium. It can be seen in association with intrauterine as well as ectopic pregnancies and does not indicate the location of the pregnancy. Histologically, the glands of the endometrium show cytologic atypia with hobnail cells with prominent nuclei (Fig. 11.2). This can mimic one of the histologic patterns seen with clear cell adenocarcinoma, the tubulopapillary pattern, with which Arias-Stella change should not be confused. Clear cell adenocarcinoma of the endometrium generally occurs in a much older patient population and is not associated with pregnancy. Arias-Stella change can also be seen in the cervix, and in extrauterine sites, such as in endometriosis [2].
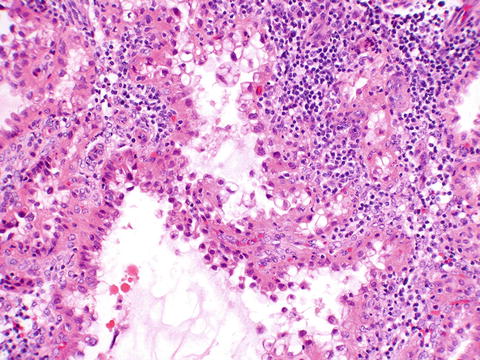
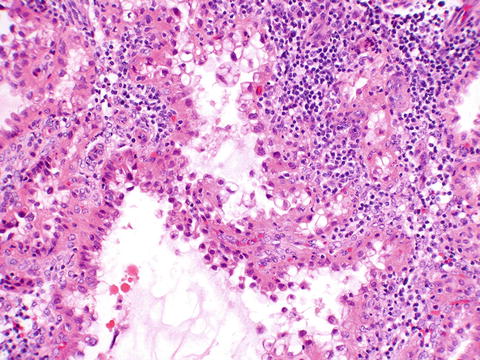
Fig. 11.2
Arias-Stella reaction in gestational endometrium from a partial mole. The glands show hobnail cells with nuclear atypia
11.3.2 Spontaneous Abortion (Implantation Site)
With first trimester pregnancy loss, the pathologist reviewing the products of conception is tasked first and foremost with proving that an intrauterine pregnancy was present. When chorionic villi are present, this is a simple task. However, often with spontaneous abortion, the entire placenta has been passed prior to the patient’s curettage. The pathologist then must seek evidence of an implantation site. While this does not completely rule out an ectopic pregnancy, it considerably lowers the risk, as heterotopic pregnancies are exceedingly rare, particularly in spontaneous gestations. Risk is greater in IVF pregnancies, but is still low. In curettings from a patient with a spontaneous abortion who has passed the placenta, the implantation site may be recognized by a fibrinoid layer on the decidua, Nitabuch’s fibrin, the best place to identify the confirmatory implantation site trophoblasts (Fig. 11.3a, b).
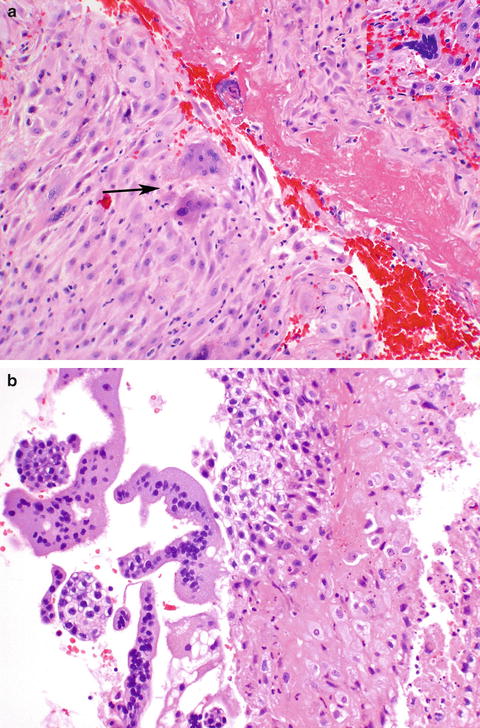
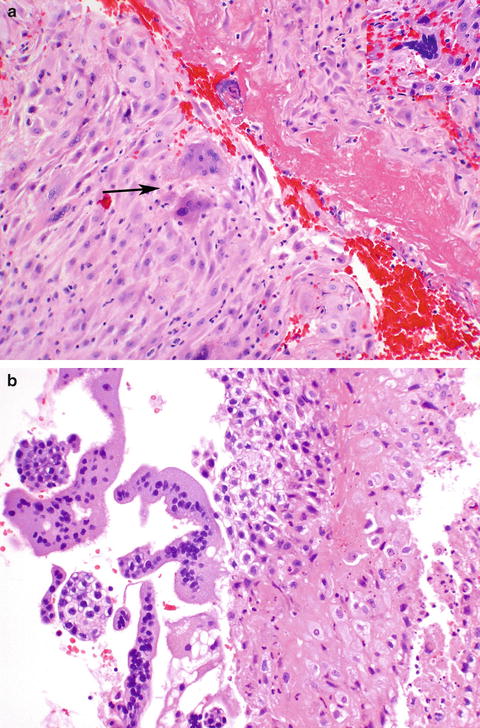
Fig. 11.3
Implantation site. Nitabuch’s fibrin is seen adjacent to two implantation site intermediate trophoblasts (arrow). Occasionally syncytiotrophoblasts may also be seen (inset upper right) (a). Implantational intermediate and syncytiotrophoblasts can sometimes be seen in curettings without villi, adjacent to fibrin, confirming a recent intrauterine pregnancy (b)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


