(1)
Department of Pathology, Rutgers-New Jersey Medical School, Newark, NJ, USA
Keywords
Complete hydatidiform molePartial hydatidiform moleInvasive moleChoriocarcinomaPlacental site trophoblastic tumorEpithelioid trophoblastic tumorPlacental site nodulePlacental site plaqueExaggerated placental site13.1 Gestational Trophoblastic Neoplasia
Gestational trophoblastic neoplasia (GTN) is classified differently by the clinician and the pathologist. There may be treatment decisions made without tissue being obtained for histopathologic evaluation, particularly in GTN that follows a known hydatidiform mole. The clinical classification relates to tumor location and risk factors, not to histology. GTN may be uterine or extrauterine (invasive mole can rarely go to lungs, vulva, vagina), and tissue is not always available or needed to treat these patients. Clinical GTN is considered either benign (i.e., hydatidiform moles) or malignant. Malignant GTN is either nonmetastatic or metastatic. Metastatic disease is subdivided into good or poor prognosis based on specific risk factors. FIGO staging with a WHO scoring system [1] is utilized to make the prognostic determinations. The following discussion refers to the pathology of GTN where tissue is available for evaluation and some of the recent developments and challenges associated with diagnosis (Table 13.1).
Table 13.1
Key points about gestational trophoblastic disease
Tissue may not be obtained in cases of GTN |
There are areas of diagnostic difficulty for the pathologist: |
Areas of pathological diagnostic difficulty |
Early complete mole may not be recognized, or may be diagnosed as a partial mole |
Partial mole is difficult to distinguish histologically from missed hydropic abortion |
There is a risk of overdiagnosis of mole in tubal ectopic pregnancies due to exuberant trophoblast |
There is a risk of overdiagnosis of exaggerated placental site as PSTT, particularly on curettage |
There is a risk of overdiagnosis of atypical nonvillous trophoblast (often with a complete mole) as choriocarcinoma or PSTT |
The best approach is to consider patient age, beta-hCG levels, history of recent or remote pregnancy, imaging findings, then perform in-depth histopathologic evaluation with appropriate immunohistochemistry |
13.2 Hydatidiform Mole
Hydatidiform moles may either be complete or partial. These present differently clinically, are genetically different, and have different risks for persistent GTN.
13.2.1 Complete Hydatidiform Mole
Complete moles are mostly 46XX, which can result from paternal duplication occurring after loss of maternal genetic material, or occasionally with dispermic fertilization of an empty egg. Geography and age have impact on risk, with the lesion being more common in Asian populations, as well as mothers under 15 years or over 45 years of age. Fathers over 45 years of age contribute to risk.
The older clinical presentation for a complete mole was in the second trimester, with bleeding, disproportionally elevated serum beta-hCG, uterine size greater than dates, and possible hyperemesis, toxemia, hyperthyroidism, or respiratory distress in some cases. Ultrasound showed absence of a fetus with a snowstorm pattern for the molar villi. Evacuation led to a specimen composed of “grapes,” the hydropic villi. Patients may have ovarian theca lutein cysts at presentation (see Chap. 9).
However, patients present earlier in gestation than previously, and the first trimester specimens received by the pathology laboratory often lack the pronounced features of a second trimester complete mole (Fig. 13.1a–d). Second trimester moles show pronounced trophoblastic hyperplasia circumferentially around villi, and as extravillous clusters, with hydropic villi, enlarged, and some so edematous that cisterns have formed. With earlier terminations, uniform trophoblast hyperplasia and villous cavitation (“grapes”) may not have developed yet. Five features have been identified as providing histologic evidence [2]: Redundant bulbous terminal villi, hypercellular myxoid villous stroma, labyrinthine network of villous stromal canaliculi, focal nonpolar cyto- and syncytiotrophoblastic hyperplasia of villi and undersurface of chorionic plate, and enlarged atypical hyperchromatic implantation site trophoblasts (Fig. 13.1e).
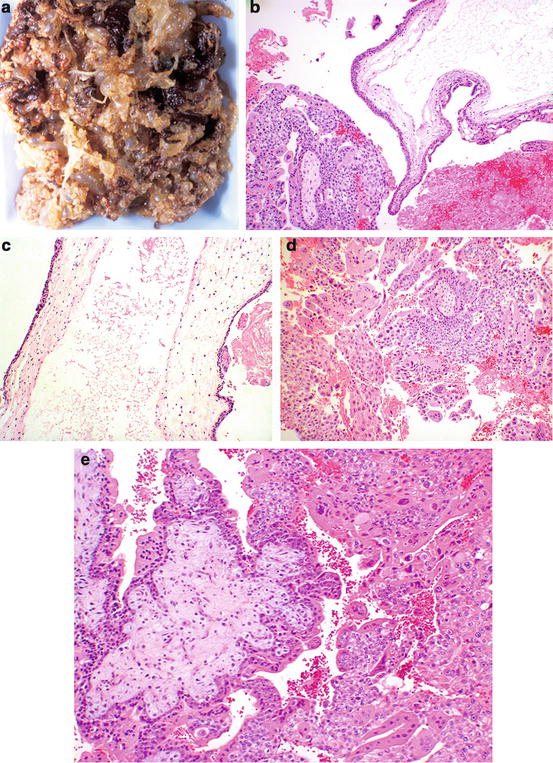
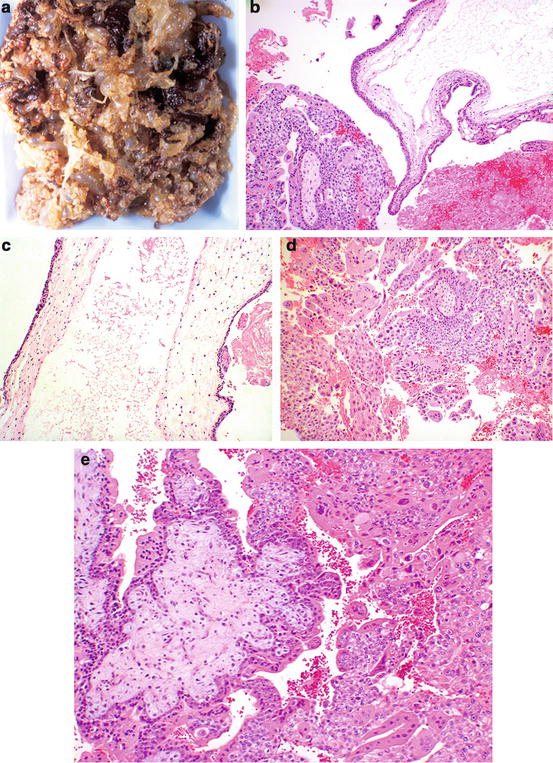
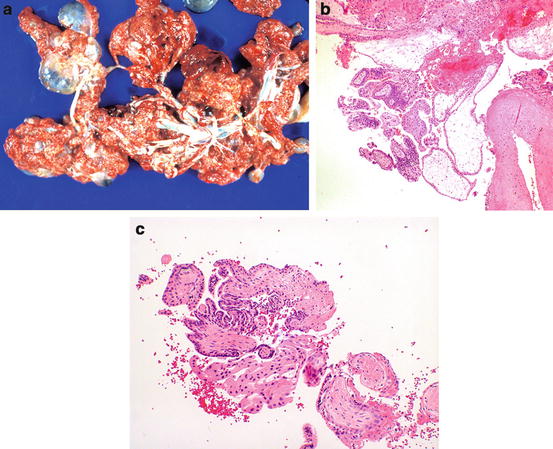
Fig. 13.1
Complete hydatidiform mole. Note the grape-like vesicular tissue (a). Histologically there is villous edema with cistern formation (right), and trophoblastic proliferation (left) (b). Higher power shows the cistern in the center of a markedly hydropic villus (c). Trophoblast proliferation is biphasic, with multinucleated syncytiotrophoblasts, and cytotrophoblasts with well-demarcated cell membranes (d). In early complete moles (e), hydropic change is less pronounced, but the villi show redundant bulbous outpouchings, hypercellular myxoid stroma with vascular anastomosing channels (left), and trophoblast proliferation (right)
A significant number of complete moles go on to persistent GTN as evidenced by elevated serum beta-hCG, but most of these are probably persistent moles or invasive moles, with only a small percent going on to choriocarcinoma. Tissue in these cases may not be acquired, and the diagnosis and treatment may be based on clinical findings alone. Although the risk of persistent GTN is greater in complete moles than partial moles, recurrence risk of both complete and partial moles is less than 2 % in subsequent pregnancies [3].
13.2.2 Partial Hydatidiform Mole
Partial moles are triploid, usually XXY, which can result from dispermic fertilization of an egg. Clinically, partial moles present as missed abortions. Unlike complete mole, there is no age-associated risk. Grossly, molar changes are much less, and only occasional or no significantly hydropic villi may be seen. Histologically, there is usually evidence of a fetus. If the fetus develops, it is abnormal, but early termination may only show fetal tissue fragments or nucleated red blood cells in villous fetal vessels as evidence of a fetus. There is a mix of normal and molar villi. The molar villi are less edematous, irregular, and scalloped in shape, and there is less trophoblastic proliferation than complete mole (Fig. 13.2a–c). This makes the distinction from hydropic (missed) abortion a challenge at times, where there may be hydropic villi, but no trophoblast proliferation. Partial moles can persist in a small number of cases, but choriocarcinoma is rare. Recurrence of a partial mole in a subsequent pregnancy is similar to complete mole, with about a 2 % risk [3].