(1)
Department of Pathology, Rutgers-New Jersey Medical School, Newark, NJ, USA
Keywords
Vaginal agenesisVaginal duplicationLongitudinal vaginal septumTransverse vaginal septumImperforate hymenVaginal cysts: Müllerian cyst, Wolffian cyst, mucinous cyst, epidermal inclusion cystVaginitis emphysematosaEndometriosisAdenosisTrichomonasBacterial vaginosisCandidaCondyloma accuminatumHerpesUlcersFistulasProlapsed fallopian tubeGranulation tissueFibroepithelial polypLeiomyomaVaginal intraepithelial neoplasiaSquamous cell carcinomaMetastatic carcinomaClear cell adenocarcinomaSarcoma botryoidesMelanomaEndodermal sinus tumor (yolk sac tumor)Urethral prolapseUrethral diverticulumUrethral caruncleUrethral carcinoma4.1 Diseases of the Vagina
“The vagina … seems almost an afterthought in the minds of most pathologists, a structure serving only to connect other far more interesting reproductive organs which harbor more curious and challenging diseases” [1]. Pathologists receive many fewer vaginal specimens than from other areas of the female reproductive tract. This is probably due to the lower rates of primary vaginal malignancies. This chapter serves to review vaginal pathology. An appropriate history supplied with these specimens will assist pathologists in providing a more useful diagnosis, and perhaps recognizing that the vagina is more than a conduit between the vulva and cervix (Table 4.1).
Table 4.1
Key points about vaginal pathology
History and location of vaginal cysts may assist in evaluating the origin of these lesions |
Superficial biopsies may impede diagnosis of processes requiring evaluation of subepithelial tissue |
Metastatic squamous cell carcinoma from cervix or vulva, including a prior history of these neoplasms, should be ruled out before primary vaginal squamous cell carcinoma is diagnosed |
4.2 Congenital Anomalies of the Vagina
The vagina is formed embryologically by two different structures. The lower 1/3 is formed by the urogenital sinus, which meets up with the upper 2/3 of the vagina, which is formed after fusion of the two Müllerian ducts. Anomalies of the vagina are subsequent to abnormalities of this process. A proposed classification based on embryology has been set forth [2]. The more common are touched on briefly here.
4.2.1 Vaginal Agenesis
Vaginal agenesis may be isolated, or may be part of the Mayer–Rokitansky–Küster–Hauser syndrome in association with uterine agenesis.
4.2.2 Vaginal Duplication
Failure of fusion of the two Müllerian ducts leads to vaginal duplication, which may occur in isolation, or with duplication of the uterus as well.
4.2.3 Longitudinal Vaginal Septum
If fusion occurs, but the septum is not resorbed, longitudinal vaginal septum is present.
4.2.4 Transverse Vaginal Septum
Transverse vaginal septum occurs due to failure of resorption of the Müllerian septum at the interface of the urogenital sinus and fused Müllerian ducts [1]. A specimen from an excision of a transverse vaginal septum may show squamous epithelium on the more caudal aspect and columnar epithelium on the more rostral.
4.2.5 Imperforate Hymen
Imperforate hymen may present in childhood as mucocolpos, or not show up until menarche as hematocolpos. Hymenal tissue is lined by nonkeratinizing squamous epithelium.
4.2.6 Adenosis
During embryogenesis, the urogenital sinus meets up with the fused Müllerian ducts. At birth, the lower genital tract is lined by squamous epithelium extending up the vagina to the squamo-columnar junction of the cervix. While it had been believed that this was urogenital squamous epithelium replacing any glandular epithelium that had been present in the upper vagina, more recently, some investigators have put forth that the upper vaginal squamous epithelium is derived from Müllerian epithelium [3]. Either spontaneously, or due to an exogenous interference with embryogenesis such as diethylstilbestrol (DES) exposure, remnants of glands may remain in the vaginal submucosa (adenosis), and over time, are replaced by metaplastic squamous epithelium (Fig. 4.1).
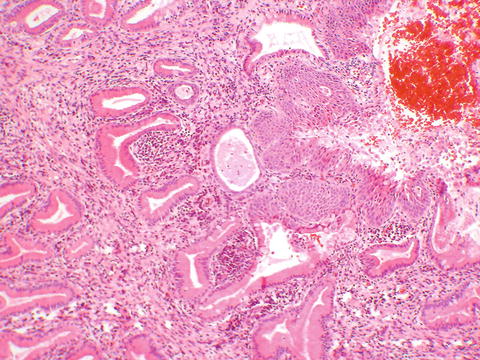
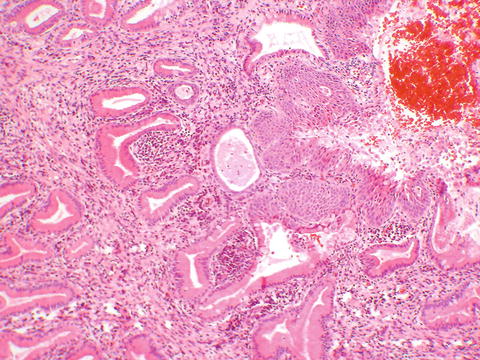
Fig. 4.1
Adenosis. Submucosal glands are being replaced by squamous metaplasia (center)
4.3 Cysts of the Vagina
Vaginal cysts are fairly common and may be either congenital or acquired. Congenital cysts may raise consideration of a genitourinary anomaly and require investigation including imaging. Acquired cysts are often at the site of prior surgery such as episiotomy [4]. The location in the vagina as well as how long the cyst has been present may be helpful to the pathologist in determining a cyst’s origin, although this can’t always be confirmed.
4.3.1 Müllerian Cyst
Müllerian cysts may arise from foci of adenosis. They are the most common vaginal cysts and may be symptomatic owing to their larger size, with symptoms including sensation of mass, pain, dyspareunia, discharge, and urinary symptoms [4]. They can occur anywhere in the vagina. Lining is variable, typical of the multipotential Müllerian epithelium, and hence mucinous, tubal, endometrioid or squamous epithelium may be seen (Fig. 4.2a).
Fig. 4.2
(a) Müllerian cyst lined with a fallopian tube type lining. (b) Gartner’s (Wolffian) duct cyst with a flat cuboidal lining. (c) Mucinous cyst, lined with a single layer of mucinous columnar epithelium. (d) Epidermal inclusion cyst, lined by squamous epithelium and containing keratinaceous debris
4.3.2 Gartner (Mesonephric, Wolffian) Cyst
The mesonephric ducts regress during embryogenesis of a female. Remnants can form cysts. These cysts are generally located along the lateral vagina, in the location of the mesonephric ducts. They tend to be smaller and less symptomatic than Müllerian cysts [4]. They are lined by a cuboidal non-mucinous epithelium and may contain eosinophilic secretions (Fig. 4.2b).
4.3.3 Mucinous Cyst
Mucinous cysts are often located in the vestibule. They may be either congenital or acquired and are thought to arise from minor vestibular glands (Fig. 4.2c).
4.3.4 Epidermal Inclusion Cyst
Squamous inclusion cysts are usually localized to prior surgery such as episiotomy, but can occur in any vaginal location. Histologically, they are lined by squamous epithelium, and the cheesy contents are histologically seen to be keratinaceous debris (Fig. 4.2d).
4.3.5 Endometriosis
Endometriosis may be cystic or solid and tends to occur in sites of prior surgery such as episiotomy, or trauma, lending credence to the implantation theory. Symptoms may be cyclic. Histologically, endometrial glandular epithelium and stroma must be present to confirm the diagnosis for the pathologist (Fig. 4.3).
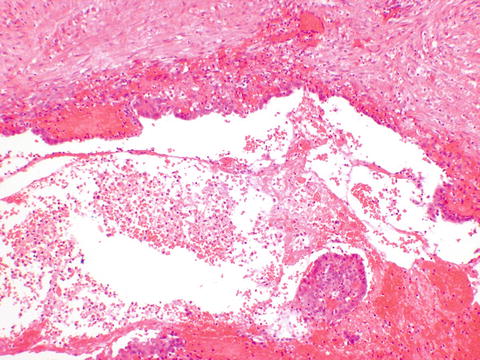
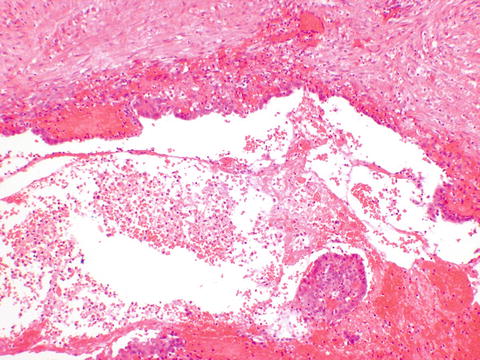
Fig. 4.3
Endometriosis. Abundant hemorrhage makes appreciation of the compressed stroma under the endometrial glandular type epithelium difficult
4.3.6 Vaginitis Emphysematosa
This is a rare self-limiting condition where multiple vaginal blebs are formed. Symptoms may include pressure, with relief if the blebs rupture during intercourse or examination [4]. The condition is thought to be related to trichomonas or bacterial vaginosis [5]. The lesions are rarely biopsied, but consistent of empty gas-filled subepithelial spaces [6].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


