13 Head and neck
ANATOMY
ANATOMY OF THE NECK
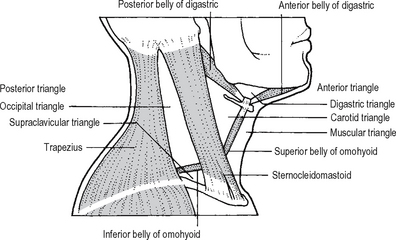
A thorough knowledge of anatomy is required to treat surgical conditions affecting the neck. For descriptive purposes the neck is divided into various triangles (Fig. 13.1). The sternocleidomastoid (SCM) divides it into two large triangles, the anterior triangle between the SCM and the midline and the posterior triangle between it and the trapezius.
Surface anatomy of the neck
The following can be felt in the midline from above downwards (Fig. 13.2):
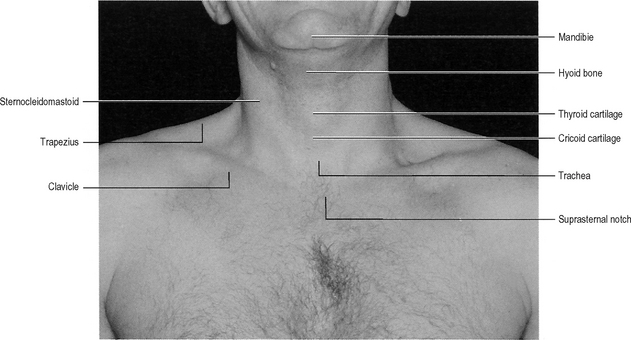
Fig. 13.2 Surface anatomy of the neck.
Source: Jacob S, Anatomy: a dissection manual and atlas; Churchill Livingstone, Edinburgh (1996).
The lower border of the cricoid is an important level in the neck and it corresponds to:
Each SCM can be tensed and tested by turning the head against resistance to the opposite side.
Deep fascia of the neck
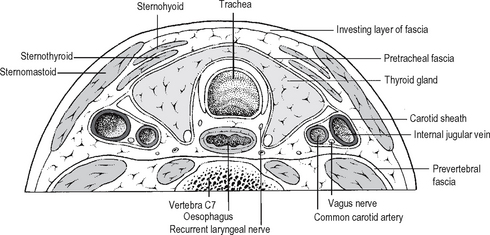
There are three distinct layers (Fig. 13.3):
The pretracheal fascia splits into an anterior layer that encloses the infrahyoid (strap) muscles and a posterior layer which forms the fascial capsule of the thyroid gland. The fascia extends into the mediastinium and merges with the pericardium. Laterally it blends with the investing layer deep to the SCM. It also contributes to the carotid sheath.
THE ANTERIOR TRIANGLE
The anterior triangle is bounded by the anterior border of the SCM, the midline and inferior margin of the mandible. It is subdivided into four smaller triangles: submental, submandibular, carotid, and muscular (Fig. 13.1). The anterior triangle contains among other structures the thyroid gland, the submandibular gland, the carotid sheath, the deep cervical group of lymph nodes, and the supra and infra hyoid groups of muscles.
Muscles attached to the hyoid bone
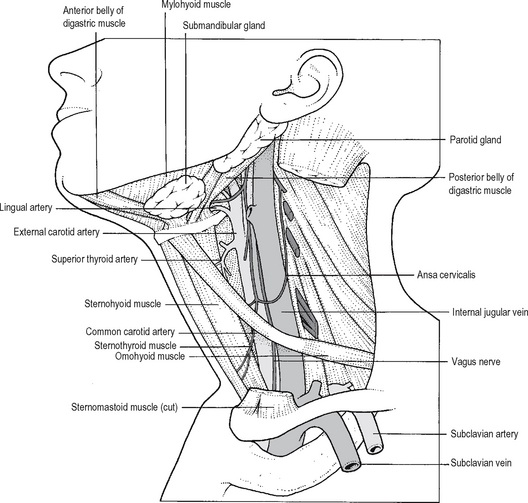
Deep to these lie the thyroid gland, the larynx, and the trachea. The infahyoids or the strap muscles are supplied by the ansa cervicalis (C1,C2,C3) which is a nerve loop on the internal jugular vein (Fig. 13.4). The branches to the muscles enter in their lower half. During exposure of a large goitre the strap muscles are cut in their upper half to preserve the nerve supply from the ansa cervicalis.
Blood vessels in the Anterior Triangle
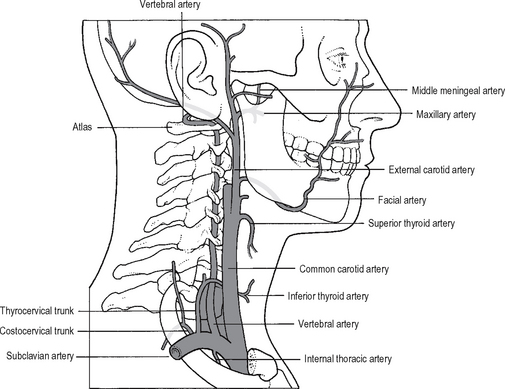
Carotid arteries
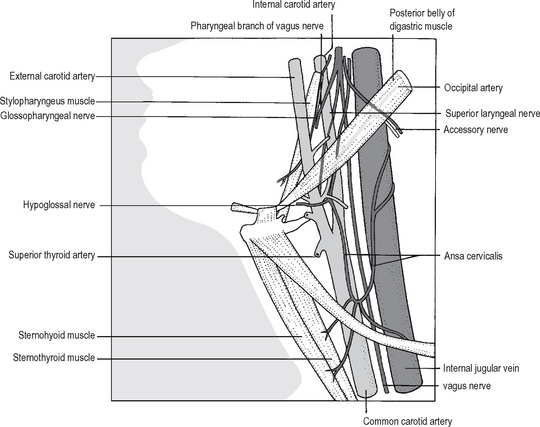
The common carotid artery is crossed at the level of the 6th cervical vertebra by the omohyoid muscle (Fig. 13.4). Above this level the artery is superficial and its pulsation can easily be felt whereas below, the artery is covered by the infrahyoid muscles and the SCM. The artery is enclosed in the carotid sheath with the internal jugular vein lateral to it and the vagus nerve between the artery and the vein at a deeper plane. The internal carotid artery passes vertically upwards as a continuation of the common carotid without giving any branches in the neck. The artery which is also enclosed in the carotid sheath is separated from the external carotid by (Fig. 13.5):
The external carotid artery extends from the point of bifurcation of the common carotid to a point midway between the angle of mandible and the mastoid process. The upper part of the artery enters the parotid gland where it divides into its two terminal branches: the maxillary artery and the superficial temporal artery. At its commencement the artery is anteromedial to the internal and can be distinguished from the internal by the presence of branches (the internal carotid has no branches in the neck). The branches of the external carotid artery are (Fig. 13.6):
POSTERIOR TRIANGLE
The boundaries are
The external jugular vein courses in the superficial fascia obliquely, pierces the deep fascia just above the clavicle and drains into the subclavian vein. Dissection of the lower part of the triangle may cause troublesome bleeding from this vein. The spinal accessory nerve is the most important structure in the posterior triangle. It exits from the jugular foramen, passes through the deep part of the sternocleidomastoid and enters the posterior triangle where it lies fairly superficially embedded in the deep fascia along the roof. It then enters the under surface of the trapezius. The nerve supplies the sternocleidomastoid and the trapezius. The accessory nerve can be damaged during biopsy of lymph nodes in the posterior triangle. This will paralyse the trapezius resulting in inability to raise the arm above the level of the shoulder as well as inability to shrug the shoulder.
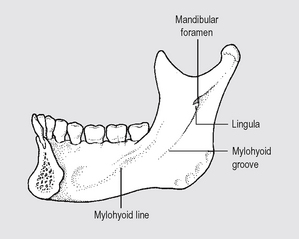
MANDIBLE
The mandible, or the lower jaw, consists of a horizontal body bearing the alveolar process and the lower teeth, and a vertically orientated ramus. The junction between the body and the ramus is the angle of the mandible. The upper part of the ramus divides into an anterior coronoid process and a posterior condyloid process which bears the head and neck of the mandible (Fig. 13.7). The head articulates with the mandibular fossa at the base of the skull to formthe temporo-mandibular joint. The neck has a depression, the pterygoid fovea, in its upper part for the insertion of the lateral pterygoid muscle. The coronoid process receives the attachment of the temporalismuscle.
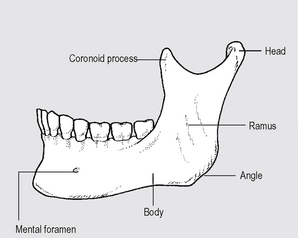
Fig. 13.7 The mandible: external surface.
Source: Rogers A W, Textbook of anatomy; Churchill Livingstone, Edinburgh (1992).
Medial surface
On the medial aspect of the ramus is the mandibular foramen (Fig. 13.8). This is guarded anteriorly by a projecting process called the lingula to which the sphenomandibular ligament is attached. The inferior alveolar (dental) nerve enters the mandibular foramen and traverses the body within the mandibular canal. It divides into the mental nerve and the incisive nerve. The incisive nerve which supplies of the incisors and canine teeth runs beyond the mental foramen within the body in the incisive canal. The trunk of the inferior alveolar nerve supplies the premolars and the molars.
A small groove runs inferiorly and forward from the mandibular foramen. This is the mylohyoid groove and is produced by the nerve to mylohyoid which supplies the mylohyoid and the anterior belly of the digastric muscles. Above the groove is a prominent ridge, the mylohyoid line for the attachment of the mylohyoid muscle. The muscle extends from the level of the last molar tooth to the midline. The two mylohyoids which form the floor of the mouth separate the oral cavity from the neck. The slight depression on the bone below the mylohyoid line is the submandibular fossa where the superficial part of the submandibular gland is located. The deep part of the gland and the sublingual gland lie above the mylohyoid line in the oral cavity. This part of the mandible is lined by the mucous membrane of the mouth.
MUSCLES OF MASTICATION
There are four pairs of muscles in this group attaching the mandible to the base of the skull:
Testing of the muscles of mastication
The muscles of mastication and their nerve supply are tested clinically by asking the patient:
TONGUE
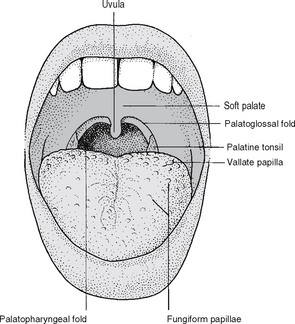
Mucosal surface
The dorsum of the tongue is divided into an anterior two-third and a posterior third by a V-shaped groove, the sulcus terminalis, the apex of which has the foramen caecum from which the thyroglossal duct giving rise to the thyroid gland develops. The mucosa of the anterior twothird carries the filiform papillae, which gives the tongue its rough feel. Slightly larger and reddish fungiform papillae are also present scattered in between these papillae. Just in front of the sulcus terminalis and parallel to it is a row of even larger papillae, the vallate papillae, about 8–12 in number. The vallate papillae carry taste buds (Fig. 13.9).
The inferior surface of the tongue is smooth and shiny and in the midline has the frenulum of the tongue. On either side of the frenulum the deep vein of the tongue can be seen (Fig. 13.10).
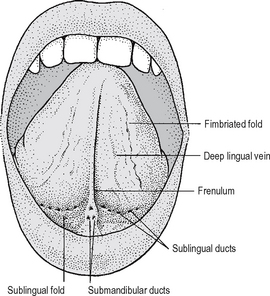
Fig. 13.10 The buccal cavity: the inferior surface of the tongue and the floor of the mouth.
Source: Rogers op. cit.
Blood supply
Arteries
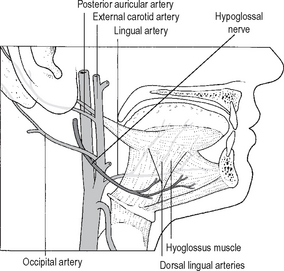
The tongue is supplied by the lingual artery, a branch of the external carotid artery the course of which is illustrated in Fig. 13.12. The dorsal lingual arteries are branches which supply the mucous membrane as well as the palatine tonsil and the soft palate. The artery is accompanied by the deep lingual vein. At its commencement, the hypoglossal nerve and its companion vein crosses superficial to the artery. At the posterior third, branches from the tonsillar artery (branch of the facial) and ascending pharyngeal artery anastomose with those of the lingual artery. There is only a poor communication between the two lingual arteries across the median septum.
Lymphatic drainage
Lymphatics from the tip of the tongue pass to the submental nodes and from there to the lower deep cervical nodes. From the mid portion lymphatics pass to the submandibular nodes and then to the deep cervical from the margin of the tongue ipsilaterally and the rest bilateral. From the posterior third the drainage is to the upper deep cervical of both sides.
FLOOR OF THE MOUTH
The floor of the mouth separating the oral cavity from the neck is formed by the mylohyoid diaphragm formed by the fusion of the mylohyoid muscles of both sides along the midline raphe Above the mylohyoid is the mouth and below is the neck. The mylohyoids are reinforced superiorly by the two geniohyoids. The anterior part of the tongue rests on the mucosa covering the floor of the mouth. In the midline, the frenulum of the tongue is seen on the floor connecting the tongue to the mandible. On either side of the frenulum is the sublingual papilla on which the submandibular gland duct opens (Fig. 13.10). Lateral to this is the sublingual fold produced by the sublingual gland.
The deep part of the submandibular gland and the submandibular duct are described on page 72.
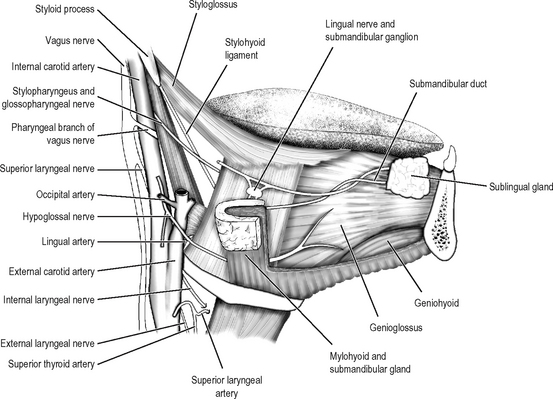
The lingual nerve, a branch of the mandibular division of the trigeminal nerve, runs forward above the mylohyoid. It gives off a gingival branch which supplies the whole of the lingual gingiva and the mucous membrane of the floor of the mouth. The lingual nerve winds round the submandibular duct (page 72) before getting distributed to the mucosa of the anterior two-thirds of the tongue. The submandibular ganglion is suspended from the lingual nerve as it lies on the hyoglossus. The preganglionic fibres in the chorda tympani synapse in this ganglion. Before reaching the floor of the mouth the lingual nerve lies against the periosteum of the alveolar process closely related to the 3rd molar tooth. The nerve can be damaged here during dental extraction.
SALIVARY GLANDS
Parotid gland
This serous salivary gland has a complex shape, irregular surfaces and important relations. An anatomy teacher told his students that during the Creation of Man the Creator poured ‘liquid parotid tissue’ into the area between the mastoid process and the ramus of the mandible, the liquid trickled into all the crevices in this region and solidified around a number of important structures. The story emphasises the complex configuration and relations of the gland which will no doubt be appreciated by a surgeon doing a total parotidectomy.
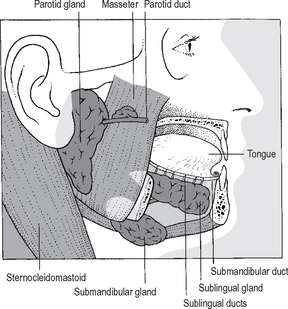
The parotid gland lies between the mastoid process and the sternocleidomastoid posteriorly, and the ramus of the mandible, which it clasps anteriorly (Fig. 13.13).
Structures passing through the parotid gland
The external carotid artery, the retromandibular vein and the facial nerve pass through the parotid gland (Fig. 13.14).
The facial nerve leaves the base of the skull through the stylomastoid foramen. The main trunk of the nerve is located in the triangle formed by the mastoid, the angle of the mandible and the cartilaginous part of the external auditory meatus. During parotidectomy, the trunk of the nerve is approached along a plane in front of the anterior margin of the cartilage. The cartilage in this region has a small projection pointing towards the nerve.
Before entering the gland the following three branches are given off from the nerve:
Submandibular gland
The submandibular gland (Fig. 13.14) and the submandibular group of lymph nodes fill the submandibular triangle which is bounded by the anterior and posterior bellies of the digastric muscle and the lower border of the mandible. The gland also extends upward deep to the mandible. Differentiating an enlargement of the gland from that of the lymph nodes can be difficult.
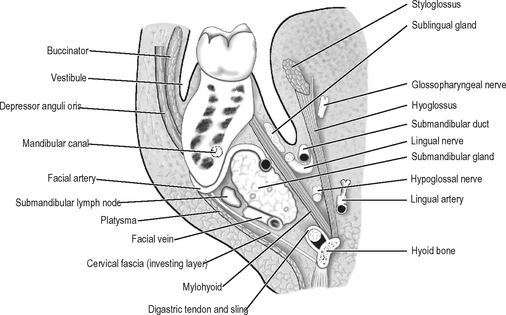
The superficial surface of the gland is covered by the skin, platysma and the investing layer of deep fascia and is crossed by the facial vein, the cervical branch of the facial nerve and also often by the marginal mandibular branch of the facial nerve. The marginal mandibular branch lies deep to the platysma and is one of the most important relations of the gland. This branch which supplies the depressor anguli oris and the depressor labii inferioris is liable to injury during surgery of the submandibular region. Injury of the nerve can result in facial asymmetry and occasional dribling. Skin incisions in the submandibular region are made about 4 cms below the mandible to avoid injury to the marginal mandibular branch.
The superficial part
This part of the gland lying superficial to the mylohyoid muscle has a superficial surface facing inferiorly in the submandibular triangle. The upper part of this surface lies deep to the body of the mandible. Its deep surface is related to the digastric below and above this to the mylohyoid anteriorly, and to the hyoglossus muscle posteriorly. The facial artery grooves the deep surface and emerges on to the face by passing between the gland and the mandible (Fig. 13.15). Several submandibular lymph nodes lie on the superficial surface.
Submandibular duct
The duct of the submandibular gland (Wharton’s duct) starts in the superficial part, running posteriorly and superiorly to reach the deep part. Here it turns forward and medially and emerges on to the surface of the hyoglossus muscle. It runs forward deep to the mucosa of the floor of the mouth between the mucosa and the sublingual gland and the geniohyoid muscle to open into the floor of the mouth on either side of the frenulum of the tongue. The duct, on the floor of the mouth is closely related to the lingual nerve. As it goes forward it crosses medial to the nerve to lie above the nerve and then crosses back, this time lateral to it to reach a position once again below the nerve (Fig. 13.16).
Four nerves are closely related to the submandibular glands and hence are vulnerable during its removal. marginal mandibular branch of the facial nerve may be bruised during skin incision. The nerve to mylohyoid is closely related to the superficial part of the gland. The lingual nerve can be damaged during ligation of the submandibular duct. The hypoglossal nerve is related to the deep part of the gland.
PHARYNX
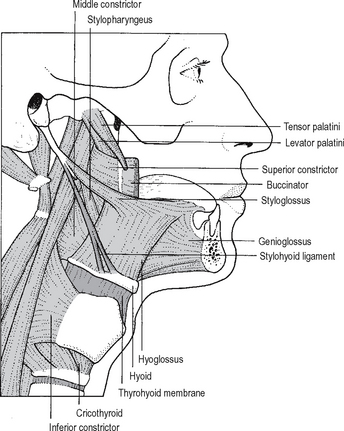
Muscles of the pharynx
The main muscles of the pharynx are the three fan-shaped constrictor muscles:
These are reinforced by much smaller longitudinal muscles: