Figure 27–1 Pathophysiology of asthma and sites of anti-inflammatory drug action. When allergens activate T cells, cytokine production is stimulated. The cytokines, in turn, trigger the recruitment, activation, and release of a variety of cells and mediators. Glucocorticoids inhibit numerous steps in this process, including T-cell activation, cytokine production, eosinophil recruitment and activation, and mast cell migration. Glucocorticoids, cromolyn sodium, and other cromolyn-related drugs all inhibit the release of mediators from mast cells and eosinophils. Cromolyn and related drugs also inhibit eosinophil chemotaxis induced by cytokines and other mediators. Leukotriene inhibitors either block leukotriene receptors or inhibit leukotriene synthesis. IgE = immunoglobulin E.
Rhinitis
Rhinitis is most frequently caused by allergic reactions to pollens, mold spores, dust mites, and other environmental allergens or by infections with viruses, such as rhinoviruses and other agents of the common cold.
Allergic rhinitis can be seasonal or nonseasonal (perennial), whereas viral rhinitis is an acute, self-limiting condition. Both types of rhinitis are characterized by sneezing, nasal congestion, and rhinorrhea. Nasal pruritus and conjunctivitis are more commonly associated with allergic rhinitis than with viral rhinitis. Malaise, pain, and general discomfort are generally associated with viral rhinitis.
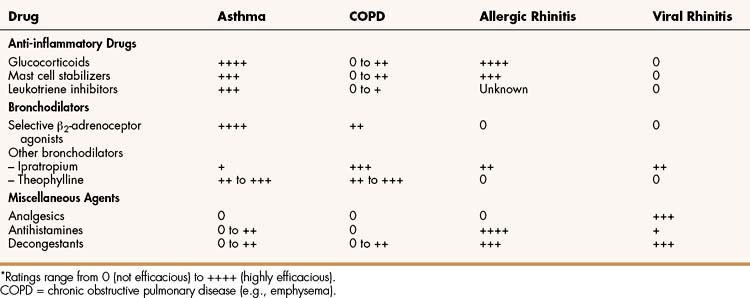
Table 27–1 shows the relative efficacy of various types of respiratory tract drugs, including those used in the treatment of allergic rhinitis and viral rhinitis.
Chronic Obstructive Pulmonary Diseases
COPDs include chronic bronchitis and emphysema. Chronic bronchitis is characterized by a productive cough associated with inflammation of the bronchioles, whereas emphysema is caused by permanent destruction and enlargement of the airspaces distal to the bronchioles. Both conditions result in airway obstruction, dyspnea (difficult breathing), decreased blood oxygen concentrations, and elevated blood carbon dioxide concentrations. Patients with these conditions have abnormal pulmonary function test values, such as a decreased forced expiratory volume in 1 second (FEV1). Smoking and advanced age are the primary risk factors for COPD, and smoking cessation can slow disease progression. Although most of the airway obstruction in COPD is irreversible, a portion of the obstruction is caused by smooth muscle spasm and bronchiolar inflammation, and this portion can be reversed by bronchodilator drugs. Patients with COPD often require long-term oxygen therapy, and antibiotics can be used to treat acute exacerbations caused by bacterial infections.
ANTI-INFLAMMATORY DRUGS
Glucocorticoids
Glucocorticoids (corticosteroids) are effective in the treatment of a wide variety of inflammatory and other diseases. The discussion here focuses on the use of glucocorticoids for asthma, allergic rhinitis, and COPD. Chapter 33 provides a detailed description of their properties and use.
The recognition that asthma is primarily an inflammatory disease has increased the role of glucocorticoids in asthma therapy. For persons with moderate to severe asthma, glucocorticoids have become the cornerstone of therapy, and some patients with mild asthma may derive significant benefit from their use as well. Although glucocorticoids are the most efficacious anti-inflammatory drugs available for the treatment of both asthma and allergic rhinitis (see Table 27–1), they have the potential to cause a number of adverse effects if given systemically. The incidence of adverse effects is markedly reduced when these drugs are given by inhalation, so this route of administration is employed whenever possible. Systemic administration is usually reserved for the treatment of severe asthma or for short-term treatment of severe allergic rhinitis.
Among the glucocorticoids available as metered-dose inhalers are beclomethasone, budesonide, fluticasone, and triamcinolone. Beclomethasone and triamcinolone are usually administered three or four times a day, whereas fluticasone and budesonide need to be administered only twice a day. The proper use of metered-dose inhalers requires considerable skill and the utilization of a spacer device between the mouth and the inhaler. The spacer decreases the amount of drug that is deposited in the mouth and upper airway and facilitates the delivery of the drug to the bronchioles.
As with other anti-inflammatory drugs, glucocorticoids are primarily used on a long-term basis to prevent asthmatic attacks, rather than to treat acute bronchospasm. The maximal response to glucocorticoids usually requires treatment for up to 8 weeks. Glucocorticoids can reduce the number and severity of symptoms and decrease the need for β2-adrenoceptor agonists and other bronchodilators.
Adverse effects associated with inhaled glucocorticoids are usually mild. Excessive deposition of the drugs in the mouth and upper airway can lead to oral candidiasis (thrush). There has been some concern about the potential for glucocorticoids to suppress growth in children. This problem is difficult to evaluate because asthmatic children may have growth disturbances related to their disease. A meta-analysis of 21 studies, however, concluded that inhaled beclomethasone does not cause growth impairment. Another study showed that 95% of children who received inhaled budesonide for an average of 9 years reached their target adult height despite initial growth retardation.
Mast Cell Stabilizers
Cromolyn Sodium
CHEMISTRY AND MECHANISMS
Cromolyn sodium and related drugs are nonsteroidal compounds that stabilize the plasma membranes of mast cells and eosinophils and thereby prevent degranulation and release of histamine, leukotrienes, and other substances that cause airway inflammation (see Fig. 27–1). Hence, these drugs are often called mast cell stabilizers. Inhibition of mediator release by cromolyn and related drugs is thought to result from blockade of calcium influx into mast cells. Cromolyn and related drugs do not interfere with the binding of immunoglobulin E (IgE) to mast cells or with the binding of antigen to IgE. Their beneficial effects in asthma and other conditions are largely prophylactic.
PHARMACOKINETICS
Cromolyn and other mast cell stabilizers are rather insoluble in body fluids, and minimal systemic absorption occurs after oral administration or inhalation of these drugs. In fact, the oral bioavailability of cromolyn is about 1%. When cromolyn is administered by inhalation, its major effect is exerted on the respiratory tract and very little is absorbed into the circulation. Most of the drug is swallowed following inhalation, and about 98% is excreted in the feces.
INDICATIONS
Cromolyn is administered by inhalation to treat asthma or allergic rhinitis and is available in an ophthalmic solution to treat vernal (seasonal) conjunctivitis. Cromolyn and related compounds are primarily used for the long-term prophylaxis of asthmatic bronchoconstriction and allergic reactions, and they have no role in the treatment of acute bronchospasm. For perennial asthma, the drug is usually given several times a day at regular intervals until symptoms resolve. Improvement can require several weeks, and then the dosage can be reduced to the lowest effective level. For exercise-induced asthma, cromolyn is inhaled 1 hour or less before the anticipated exercise. For allergic rhinitis or vernal conjunctivitis, cromolyn is administered several times a day at regular intervals.
Cromolyn is administered orally before meals and at bedtime to treat systemic mastocytosis, a rare condition characterized by infiltration of the liver, spleen, lymph nodes, and gastrointestinal tract with mast cells. A similar dosage schedule has been used to treat ulcerative colitis and food allergy.
ADVERSE EFFECTS
Cromolyn and other mast cell stabilizers are remarkably nontoxic, partly because of their low solubility and systemic absorption. In some patients, however, inhaled cromolyn can irritate the throat and cause cough and bronchospasm. Administration of a β2-adrenoceptor agonist can usually prevent or relieve this reaction. Nasal and ocular preparations can cause localized pain and irritation, but these effects are usually mild and transient. Cromolyn does not interact significantly with other drugs.
Lodoxamide and Nedocromil
Lodoxamide is formulated as an ophthalmic solution to treat ocular allergies, including vernal keratitis and vernal conjunctivitis. It can cause ocular discomfort but is generally well tolerated.
Nedocromil has properties that are similar to those of cromolyn, but it is only available as an aerosol for the prevention of bronchoconstriction in patients with asthma. It is initially administered as two inhalations four times a day, but the frequency of doses can be reduced in persons whose asthma is well controlled.
Leukotriene Inhibitors
Leukotrienes (leuko from leukocytes; trienes from three conjugated double bonds) are a group of arachidonic acid metabolites formed via the 5-lipoxygenase pathway in mast cells and various types of leukocytes, as shown in Figure 27–2. Cysteinyl leukotrienes C4, D4, and E4 activate the type 1 cysteinyl leukotriene receptor (CysLT1) and thereby increase recruitment of leukocytes, stimulate mucus secretion, increase vascular permeability, increase collagen, and cause smooth muscle proliferation and contraction. These effects lead to airway inflammation and to sustained bronchoconstriction. The effects of leukotrienes are mediated by activation of G protein–coupled receptors linked with Gq and Gi, which increase intracellular calcium, decrease cyclic adenosine monophosphate (cAMP), and lead to protein kinase activation and tissue responses.
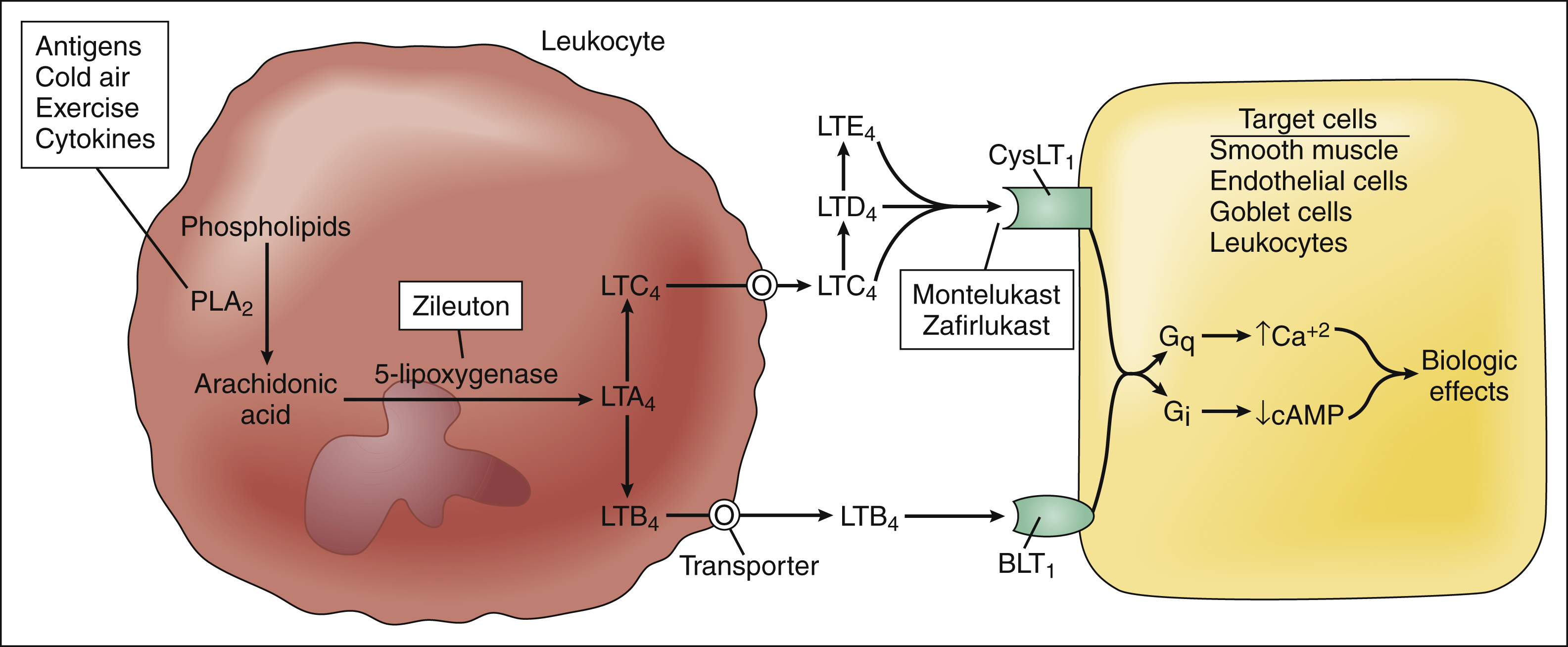
Figure 27–2 Synthesis and effects of leukotrienes and sites of drug action. Asthmatic stimuli (antigens, cold air, exercise, cytokines, and others) activate phospholipase A2 (PLA2), leading to formation of leukotriene A4 (LTA4) by 5-lipoxygenase, which is inhibited by zileuton. LTA4 is converted to leukotriene B4, which activates B leukotriene receptors, such as BLT1. LTA4 is also converted to the cysteinyl leukotrienes C4, D4, and E4, which activate cysteinyl leukotriene receptors, such as CysLT1. These receptors are blocked by montelukast and zafirlukast. Leukotriene receptors are coupled with Gq and Gi, leading to increased intracellular calcium, decreased cAMP, activation of protein kinases, and biologic effects.
Leukotriene Receptor Antagonists
MECHANISMS
Montelukast and zafirlukast have a structure that resembles that of the cysteinyl leukotrienes, and they compete with these substances for the CysLT1 receptor. These drugs inhibit both the early and the late phases of bronchoconstriction induced by antigen challenge. However, they do not block the effects of leukotriene B4, which appear to be important in severe asthma and asthma exacerbations.
PHARMACOKINETICS
Montelukast and zafirlukast are administered orally and are well absorbed from the gut. Montelukast is taken as a single daily dose in the evening and is available in dosage forms for treating adults and pediatric patients as young as 6 months old. Zafirlukast is indicated for patients aged 5 years and older and is given twice daily 1 to 2 hours before meals because food retards its absorption. These drugs are highly bound to plasma proteins (>99%) and are extensively metabolized by hepatic cytochrome P450 enzymes.
EFFECTS AND INDICATIONS
Montelukast and zafirlukast have been shown to improve pulmonary function, control symptoms, reduce the need for short-acting rescue β2-agonists, decrease asthma exacerbations, and improve overall quality of life. Although inhaled glucocorticoids are more potent than leukotriene antagonists and are generally preferred for initial therapy, antileukotriene agents can be used in persons who are unable or unwilling to take glucocorticoids. Leukotriene receptor antagonists offer the advantages of convenient oral administration and minimal side effects, and they often benefit asthmatic patients not adequately controlled by inhaled steroids alone. They are probably not as effective as long-acting β2-agonists as add-on therapy to glucocorticoids, but they may be safer (see below).
Antileukotriene drugs are effective in persons with allergic asthma, including aspirin-sensitive asthma, and they may be used to prevent exercised-induced asthma when taken at least 2 hours before the precipitating event. The beneficial effects of these drugs are cumulative, and maximal effectiveness may require several weeks to months of therapy. Although they are not indicated for the treatment of acute bronchospasm, they do enhance the bronchodilating effect of β2-agonists. In general, antileukotriene agents benefit children more than adults, and younger children more than older children.
ADVERSE EFFECTS AND INTERACTIONS
Leukotriene antagonists are relatively free of serious adverse effects, but hypersensitivity reactions and other adverse effects may occur in a small percentage of patients. Rare cases of liver injury have been reported, and a few cases of liver failure have occurred. Rarely, allergic granulomatous vasculitis (Churg-Strauss syndrome), a condition often treated with corticosteroids, has developed in patients being withdrawn from glucocorticoid therapy while substituting a leukotriene antagonist. In such cases, glucocorticoids should be withdrawn gradually and patients closely monitored.
Zafirlukast inhibits CYP2C9 and CYP3A4 and may interfere with the metabolism of phenytoin and warfarin (metabolized by CYP2C9) and of felodipine, lovastatin, and triazolam (metabolized by CYP3A4). Montelukast does not inhibit these isozymes or exhibit significant drug interactions, and its use may be preferred in patients receiving concomitant drug therapy.
Zileuton
EFFECTS AND INDICATIONS
Leukotriene synthesis increases during an asthmatic attack; this can be prevented by zileuton, which inhibits 5-lipoxygenase and blocks the formation of all leukotrienes, including LTB4. Because the CysLT1 receptor antagonists do not block the leukocyte chemoattractant and other effects of LTB4, zileuton might be more effective in severe cases of asthma where these effects may be particularly important.
Zileuton is indicated for the prophylaxis and treatment of asthma in adults and children 12 years of age and older. The immediate-release formulation should be taken orally four times a day, but a sustained-release preparation is now available for twice-daily administration. Zileuton undergoes some first-pass hepatic inactivation and is almost entirely eliminated as the glucuronide metabolite with a half-life of about 2 hours.
ADVERSE EFFECTS AND INTERACTIONS
Mild and transient adverse reactions to zileuton use include a flulike syndrome, headache, drowsiness, and dyspepsia. Zileuton may elevate hepatic enzyme levels, so patients taking the drug should be monitored for signs of hepatitis. Patients with transaminase levels greater than three times the upper limit of normal should discontinue zileuton, and it should be used cautiously in patients who consume substantial quantities of alcohol.
Zileuton inhibits CYP1A2 and CYP3A4, and it may elevate plasma concentrations of theophylline and warfarin. Doses of these drugs may need to be reduced in individuals taking zileuton.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree