Figure 36–1 Calcium and bone metabolism. Vitamin D facilitates calcium absorption from the gut. Parathyroid hormone (PTH) decreases calcium excretion in the urine but increases phosphorus excretion (not shown). Endogenously secreted PTH increases bone resorption (and also bone formation), whereas calcitonin decreases bone resorption.
Vitamin D stimulates calcium absorption by increasing the synthesis of a calcium-binding protein that mediates the gastrointestinal absorption of calcium. Vitamin D also stimulates bone resorption and the closely coupled process of bone formation.
The PTH has four actions that increase the extracellular calcium concentration. First, it stimulates resorption of calcium by renal tubules. Second, it decreases resorption of phosphate by renal tubules. This decreases the extracellular phosphate concentration, which in turn tends to increase the extracellular calcium concentration. Third, PTH stimulates the hydroxylation of vitamin D in the kidneys (Fig. 36–2). Fourth, PTH increases bone resorption by stimulating osteoclast activity, which enables bone calcium to enter the extracellular pool.
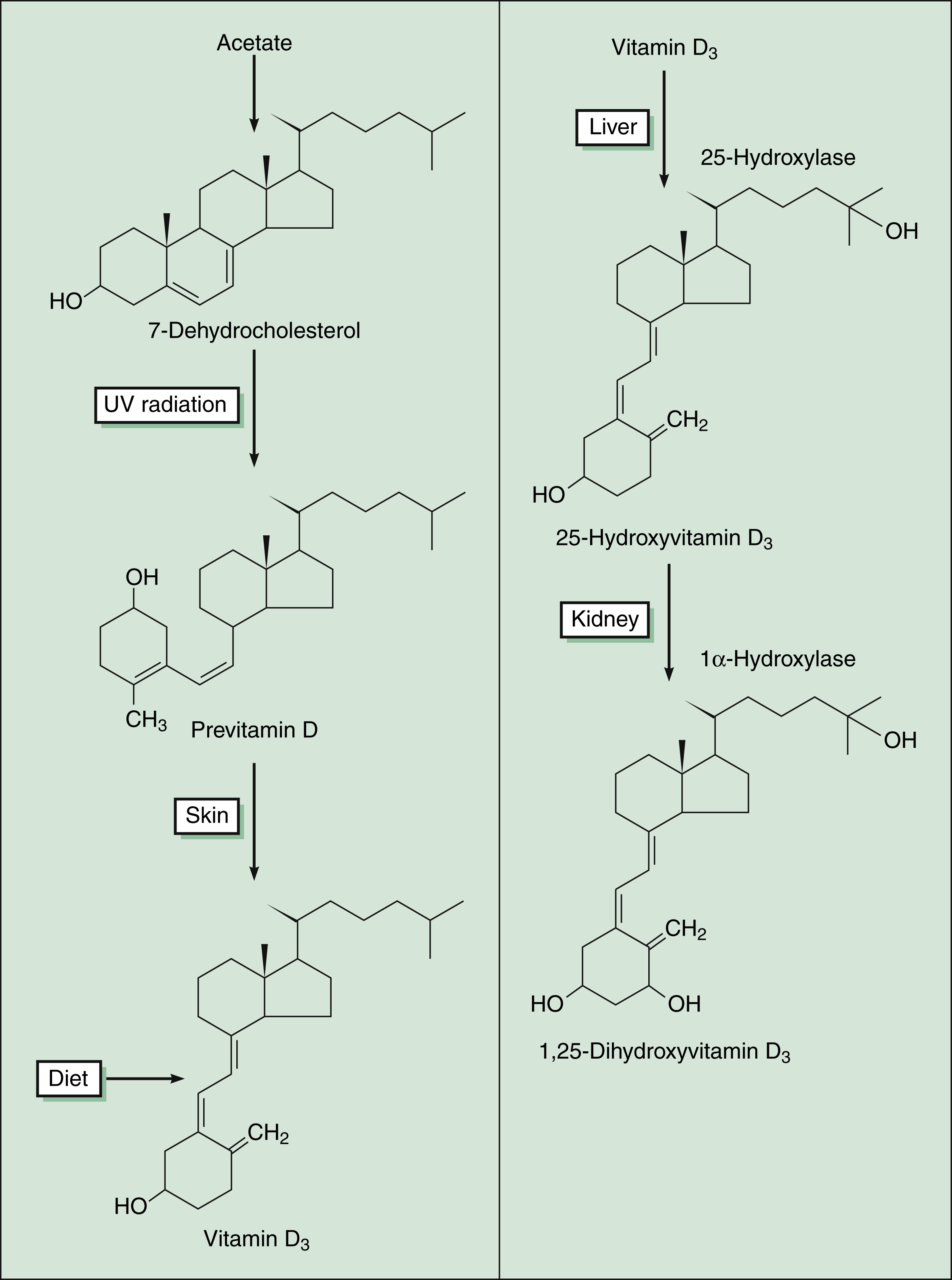
Figure 36–2 Synthesis of vitamin D. Vitamin D3 (cholecalciferol) can be synthesized in the human body from acetate through a pathway that requires ultraviolet (UV) radiation. Diet and vitamin supplements also provide vitamin D3, which is activated by specific hydroxylation steps in the liver and kidneys to form 1,25-dihydroxyvitamin D3 (calcitriol).
Calcitonin is released in response to increased plasma calcium levels, and it acts to inhibit bone resorption and thereby decreases plasma calcium levels. The physiologic significance of calcitonin is unclear, because normal calcium balance is maintained in the absence of calcitonin in persons who undergo thyroidectomy.
Bone remodeling (Fig. 36–3) consists of a sequence of events involving the dynamic interaction of osteoclasts (bone-resorbing cells) and osteoblasts (bone-forming cells). The recruitment and activation of osteoclasts are mediated by compounds released from osteoblasts and peripheral leukocytes called bone cell cytokines. The cytokines include interleukins, tumor necrosis factor, and colony-stimulating factors. After the osteoclasts are activated, they adhere to the bone surface and release hydrogen ions and proteases to break down the bone. The destroyed bone releases growth factors that increase osteoblast production and decrease osteoclast activity. The osteoblasts then lay down new bone in the cavity created by osteoclasts. The entire remodeling process takes about 100 days on average. Trabecular bone undergoes more remodeling than cortical bone (25% vs. 3% annually).
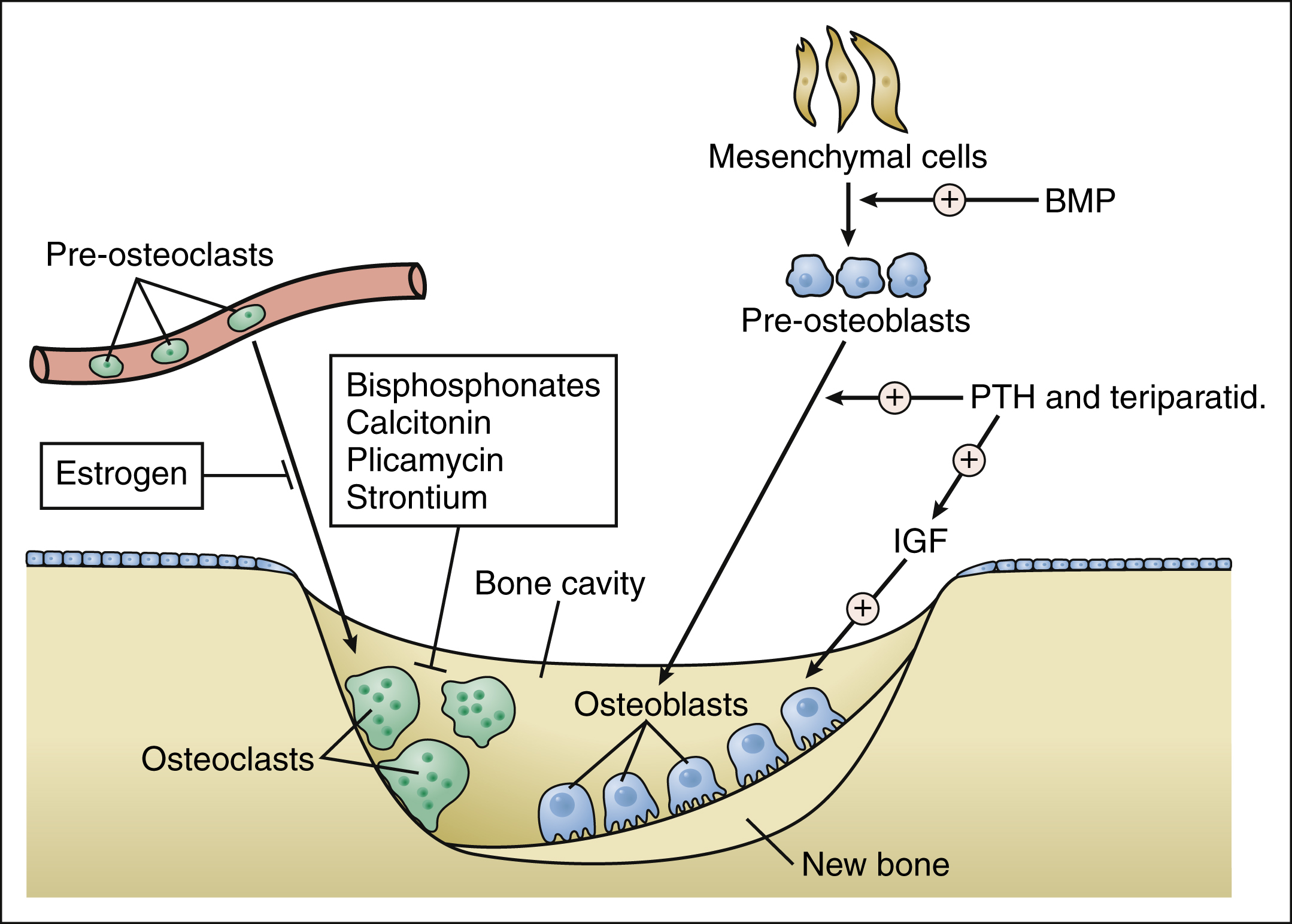
Figure 36–3 Effects of drugs and hormones on bone remodeling. Bone remodeling consists of two phases, bone resorption followed by bone formation. In the first phase, growth factors induce circulating pre-osteoclasts to differentiate to osteoclasts and attach to bone. Osteoclasts erode the mineral and matrix of bone surfaces, creating small cavities. In phase two, bone morphogenetic protein (BMP) and other factors induce mesenchymal cells to differentiate into pre-osteoblasts. Under the influence of PTH, pre-osteoblasts become osteoblasts and are further stimulated by insulin-like growth factor (IGF) to fill the cavities with new bone matrix that is subsequently mineralized. Short-term intermittent administration of teriparatide mimics the effect of PTH on bone formation and increases bone mass, but continuous long-term administration of these hormones increases bone resorption.
The balance between bone resorption and bone formation is usually maintained until the third or fourth decade of life, when a slow, age-related imbalance begins and favors resorption over formation. Hormonal and nutritional deficiencies can also contribute to this imbalance.
Bone Disorders
Osteoporosis, the most common bone disorder, is characterized by a gradual reduction in bone mass that weakens the bone and leads to the occurrence of fractures with minimal trauma. The disorder is frequently classified as postmenopausal, senile, or secondary to other diseases. Vertebral fractures are the most frequent type of fractures seen in patients with postmenopausal osteoporosis, a disorder caused primarily by estrogen deficiency. Hip, humerus, pelvis, and vertebral fractures occur in patients with senile osteoporosis, a disorder primarily resulting from advanced age; this disorder is a major cause of immobility, morbidity, and mortality in the elderly. In the United States, the annual cost of osteoporotic hip fractures alone is currently about $10 billion, and the cost is projected to rise to $240 billion by the year 2040 if more effective methods of prevention and treatment are not discovered and implemented (Box 36-1).
BOX 36–1 A CASE OF LOW BONE DENSITY
CASE PRESENTATION
A healthy 50-year-old woman has returned to her physician to assess hormone replacement therapy. She recently entered menopause and has been taking a low dose of oral estrogen and a vaginal estrogen cream along with cyclic medroxyprogesterone to relieve menopausal symptoms for the past 3 months. The treatment has reduced hot flashes and sleep disruption, but she still has an occasional episode. Because her mother suffered from osteoporosis and hip fracture, the woman asks about preventive therapy. She has been taking an adequate amount of calcium and has increased her intake of vitamin D. Her physician arranges for a BMD test, which reveals that her BMD T-score is −2 (normal is greater than −1). Based on her T-score and family history of osteoporosis, her physician suggests that she begin therapy with alendronate. She will be scheduled for a follow-up BMD in 6 months.
CASE DISCUSSION
BMD typically increases until about age 35 and then levels off until menopause. After menopause, BMD usually undergoes a sharp decline, and the risk of fractures increases with age. BMD is often determined using dual energy x-ray absorptiometry. The T-score compares a woman’s BMD in grams per square centimeter with that of healthy young adults. The T-score is calculated as (patient’s BMD − average young adult BMD) divided by 1 standard deviation of young adult BMDs. A normal T-score is greater than −1, whereas scores of −1 to −2.5 indicate low bone mass (osteopenia) and a risk of developing osteoporosis. Scores less than −2.5 indicate osteoporosis. Treatment guidelines recommend that women with risk factors receive preventive therapy if their T-score is less than −1.5. The risk factors include a previous fragility fracture, a family history of fracture, cigarette smoking, and low body weight (<127 lb). Hence, the woman meets the criteria for preventive treatment, and a bisphosphonate drug is usually selected for this purpose. If this treatment does not improve her BMD, teriparatide therapy might be considered.
Paget’s disease of bone, or osteitis deformans, is the second most common bone disorder. Characterized by excessive bone turnover, it causes bone deformities, pain, and fractures. Its cause is unknown.
Osteomalacia is characterized by abnormal mineralization of new bone matrix. The condition has numerous causes, the most common of which include vitamin D deficiency, abnormal vitamin D metabolism, phosphate deficiency, and osteoblast dysfunction. In children, osteomalacia usually results from vitamin D deficiency and is called rickets. This disorder is uncommon today because of vitamin D–supplemented foods and sun exposure. In adults, factors such as aging, malabsorption, chronic renal impairment, and use of phenytoin or other anticonvulsant drugs can interfere with vitamin D absorption, metabolism, or target organ response and result in osteomalacia.
Calcium and Vitamin D Supplements
An adequate intake of calcium and vitamin D is essential for optimal bone formation in children and to prevent osteoporosis in adults.
In the United States, two thirds of women 18 to 30 years of age and three fourths of women over 30 years of age have an inadequate calcium intake, and this predisposes them to osteoporosis. All persons, regardless of age or gender, should meet the recommendations of the National Institutes of Health for daily calcium intake (Table 36–1). These recommendations can be met by ingesting calcium-rich foods, which are primarily dairy products, and taking oral calcium supplements if dietary intake is inadequate. By ingesting optimal amounts of calcium and vitamin D, young adults may be able to increase their bone mass and older adults can decrease the rate of bone loss.
TABLE 36–1 Calcium Intake Recommended by the National Institutes of Health Consensus Panel
| Age Group | Daily Calcium Intake (mg) |
|---|---|
| Infants | |
| 0–6 months | 400 |
| 7–12 months | 600 |
| Children | |
| 1–5 years | 800 |
| 6–10 years | 800–1200 |
| Adolescents and Young Adults | |
| 11–24 years | 1200–1500 |
| Men | |
| 25–65 years | 1000 |
| >65 years | 1500 |
| Women | |
| 25–50 years | 1000 |
| >50 years (postmenopausal) Taking estrogens | 1000 |
| Not taking estrogens | 1500 |
| >65 years | 1500 |
| Pregnant and nursing | 1200–1500 |
In one clinical study, nursing-home residents who were given 800 IU of vitamin D3 and 1200 mg of calcium were found to have an increase in bone density and a decrease in the incidence of hip and nonvertebral fractures in comparison with nursing-home residents who were given placebos. In another study, administration of vitamin D3 was found to decrease the incidence of vertebral and peripheral fractures in women with previous fractures.
Calcium
PHARMACOKINETICS
Calcium absorption from the gut is incomplete, even with consumption of adequate amounts of vitamin D. Only about 30% of calcium is absorbed from milk and other dairy products, and calcium absorption from supplements is often less than 30%. To enhance absorption, calcium tablets should be taken between meals.
The absorption of calcium carbonate requires stomach acid, whereas the absorption of calcium citrate does not. Because elderly persons can have decreased stomach acid secretion, they tend to benefit more from using calcium citrate.
INDICATIONS
In addition to their role in the prevention and treatment of osteoporosis, calcium and vitamin D are also the primary treatment for hypocalcemia. For this purpose, calcium can be given orally or intravenously.
ADVERSE EFFECTS AND INTERACTIONS
The most common adverse effect of calcium supplements is constipation. This is best managed by ingesting adequate amounts of fruits and vegetables. Calcium should not be taken with fiber laxatives, because they decrease calcium absorption. Calcium can decrease the absorption of ciprofloxacin, fluoride, phenytoin, and tetracycline, so calcium supplements should be taken at least 2 hours before or after taking these drugs.
Vitamin D
CHEMISTRY AND PHARMACOKINETICS
Vitamin D is a fat-soluble substance similar to cholesterol. The form of the vitamin that is obtained from the diet and can be synthesized in skin exposed to ultraviolet radiation is called vitamin D3, or cholecalciferol. It is a relatively inactive precursor of 1,25-dihydroxyvitamin D3, which is called calcitriol, and is the most active form of the vitamin in the human body. The formation of calcitriol involves hydroxylation of vitamin D3 at the 25 position in the liver to form calcifediol (25-hydroxycholecalciferol), which is then hydroxylated at the 1 position in the kidneys to form calcitriol (see Fig. 36–2). PTH stimulates the renal hydroxylation of vitamin D. The roles of PTH and vitamin D in calcium metabolism and homeostasis are described above.
VITAMIN D PREPARATIONS
Several vitamin D preparations are available for use as nutritional supplements to prevent vitamin D deficiency. Many preparations contain vitamin D obtained from fish oil. Specific vitamin D compounds are available to treat vitamin D deficiency and related disorders, including calcifediol and calcitriol.
INDICATIONS
Vitamin D preparations are used for the following indications: to prevent and treat vitamin D deficiency and vitamin D–dependent rickets, to treat familial hypophosphatemia (vitamin D–resistant rickets), to treat hypocalcemia caused by hypoparathyroidism, to treat postoperative and idiopathic tetany, and to prevent vitamin D deficiency in persons with chronic renal failure. Persons, including the elderly, with inadequate dietary vitamin D intake and low sun exposure should take oral vitamin D supplements to develop and maintain skeletal mass and prevent osteoporosis. Patients with chronic renal failure must be treated with calcitriol because they lack the 1α-hydroxylase enzyme required to synthesize the active form of vitamin D (see Fig. 36–2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


