DRUG CLASSES
Cholinesterase inhibitors
N-methyl-D-aspartate (NMDA) receptor antagonists
One of the greatest fears of aging is dementia. An overall term used in a variety of diseases and conditions, dementia involves the decrease in cognitive functioning, such as memory, attention, language or communication ability, and problem-solving skills. Alzheimer’s disease (AD) is the cause of about 60% to 80% of these cases of dementia. The specific pathologic changes of AD occur in the cortex of the brain. These changes involve the degeneration of nerves by amyloid plaques and tangled nerve bundles (Fig. 19.1). When neurotransmission is impaired, the clinical symptoms of dementia result. Cholinesterase inhibitors and the newer N-methyl-D-aspartate (NMDA) receptor antagonists are used to strengthen neurotransmission and improve or maintain memory in those with dementia.
PHARMACOLOGY IN PRACTICE

Mrs. Moore, 85 years of age, has been experiencing progressive forgetfulness for about a year. Her daughter was in town last week and accompanied her to the clinic. After an initial examination, the primary health care provider decided to try a cholinesterase inhibitor. Mrs. Moore has called the clinic today complaining of gastrointestinal distress symptoms. She tells you to order an x-ray and find the ulcer in her tummy. You ask her to come to the clinic and she agrees. What assessment questions do you need to ask to determine if this is an appropriate request?
Approximately 5.4 million people in the United States are diagnosed with AD. Currently the Alzheimer’s Association and the National Institutes of Health are working to create a three-stage definition of the disease, which will aid in research of causes and ways to limit progression of symptoms. Display 19.1 identifies the stages of AD and their associated clinical manifestations.
Figure 19.1 Alzheimer’s disease and the resulting dementia occur when changes in the brain hamper neurotransmission.
Other diseases, such as Parkinson’s disease, may have a dementia component, but cholinesterase inhibitors are approved primarily to treat mild to moderate dementia caused by AD. Drugs used to treat AD do not cure the disease but slow the progression of dementia. Examples of the cholinesterase inhibitors include donepezil (Aricept) and rivastigmine (Exelon). Other drug classes are used for symptomatic relief. For example, wandering, irritability, and aggression in people with AD are treated with antipsychotics, such as risperidone and olanzapine. Other drugs, such as antidepressants or antianxiety drugs, may be helpful in AD for symptoms of depression and anxiety; these drugs are all discussed in individual chapters.
Actions
Acetylcholine is the transmitter substance in the parasympathetic (or cholinergic) neuropathway. Individuals with AD experience reduction in nerve impulse transmission due to plaques and tangles as illustrated in Figure 19.2. As a result, the patient experiences problems with memory and thinking. The cholinesterase inhibitors act to increase the level of acetylcholine in the central nervous system (CNS) by inhibiting its breakdown and slowing neural destruction. However, the disease is progressive, and although these drugs alter the progress of the disease, they do not stop it. Cholinesterase inhibitors are not frequently used in late-stage AD. A newer group of drugs, NMDA receptor antagonists, is available. Memantine (Namenda) is thought to work by decreasing the excitability of neurotransmission caused by an excess of the amino acid glutamate in the CNS.
Display 19.1 Proposed Three Stages of Alzheimer’s Disease (AD)
Preclinical AD (may occur 20 years before clinical symptoms)
• Focus on research
• Measureable changes are seen in the brain on magnetic resonance imaging
• Biomarkers may be present in blood or cerebrospinal fluid
• No changes in cognitive or functional ability
Mild Cognitive Impairment (MCI) Due to AD
• Focus on limiting progression with medications
• Changes in thinking ability noticeable to patient and family members
• Thinking or memory changes due to other causes ruled out
• Functional ability remains intact
• Mild to moderate anxiety noted by person
Dementia Due to AD
• Focus on supporting function
• Memory, thinking, and behavior limit ability to function
• Variable degrees of assistance needed for activities of daily living
• Reasoning and judgement impaired
Adapted from Jack, C. R. Jr., et al. (2011). Introduction to the recommendations from the National Institute on Aging— Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, 7(3), 257–262.

Figure 19.2 Amyloid plaques and nerve tangles clog neuropathways; cholinesterase inhibitors keep acetylcholine at the nerve junction longer to promote transmission.
Uses
Cholinesterase inhibitors are used to treat early and moderate stages of dementia associated with AD. Their use for severe cognitive decline as well as other dementias, such as vascular or Parkinson’s dementia, is being studied.
Adverse Reactions
Generalized adverse reactions include:
• Anorexia, nausea, vomiting, diarrhea
• Dizziness and headache
Additional adverse reactions are listed in the Summary Drug Table: Cholinesterase Inhibitors.
Contraindications and Precautions
Cholinesterase inhibitors are contraindicated in patients with hypersensitivity to the drugs and during pregnancy and lactation (pregnancy category B).
These drugs are used cautiously in patients with renal disease, bladder obstruction, seizure disorders, sick sinus syndrome, gastrointestinal (GI) bleeding, and asthma. In individuals with a history of ulcer disease, bleeding may recur. Some patients may experience delirium as well as their underlying dementia. These drugs are used to treat dementia and should not be used to treat confused patients experiencing delirium. Display 19.2 outlines the differences between delirium and dementia.
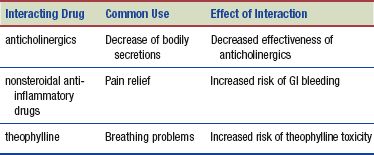
Interactions
The following interactions may occur when a cholinesterase inhibitor is administered with another agent:
 HERBAL CONSIDERATIONS
HERBAL CONSIDERATIONS
Ginkgo, one of the oldest herbs in the world, has many beneficial effects. It is thought to improve memory and brain function and enhance circulation to the brain, heart, limbs, and eyes. Conflicting research both supports and disputes ginkgo’s ability to enhance memory. Medical studies in the United States and England (UM, 2008; Snitz, 2009) have not demonstrated increases in mental function. Despite this research, the “brain herb” is still taken by healthy adults hoping to retain their current memory and cognitive function. The recommended dose is 40 mg standardized extract ginkgo three times daily. The effects of ginkgo may not be evident until after 4 to 24 weeks of treatment. The most common adverse reactions include mild GI discomfort, headache, and rash. Excessively large doses have been reported to cause diarrhea, nausea, vomiting, and restlessness. Ginkgo is contraindicated in patients taking selective serotonin reuptake inhibitor (SSRI) or monoamine oxidase inhibitor (MAOI) antidepressants because of the risk of a toxic reaction. Moreover, individuals taking anticoagulants should take ginkgo only on the advice of a primary care provider.
NURSING PROCESS
PATIENT TEACHING FOR MEDICATION INFORMATION
ASSESSMENT
Preadministration Assessment
A patient receiving a cholinesterase inhibitor may be treated in the hospital, long-term care facility, or outpatient setting. The patient’s cognitive ability and functional ability are assessed before and during therapy. Cognition can be screened by using a tool called the Mini-Mental Status Examination (MMSE). Patients are assessed on items such as orientation, calculation, recall, and language. Scoring is done by comparison with a standardized answer sheet, and the likelihood of dementia is determined. You should also assess the patient for agitation, impulsive behavior, and functional ability, such as performing activities of daily living and self-care. These assessments are used not only for monitoring the patient’s improvement (if any) after taking a cholinesterase inhibitor but also to determine appropriate living arrangements and level of care.
Before starting therapy, obtain a complete mental health and medical history. When the disease is advancing, patients with AD are not always able to give a reliable history of their illness. A family member or primary caregiver may be helpful in verifying or providing information needed for an accurate assessment. Ask the family about unusual behaviors, such as wandering or outbursts of anger or frustration. When taking the history, observe the patient for any behavior patterns that appear to deviate from normal. Examples of deviations include poor eye contact, failure to answer questions completely, inappropriate answers to questions, monotone speech pattern, and inappropriate laughter, sadness, or crying, signifying varying stages of decline. Using a standard assessment tool such as the MMSE, document the patient’s cognitive ability.
Physical assessments include obtaining blood pressure measurements on both arms with the patient in a sitting position, the pulse, the respiratory rate, and weight. Assessing the patient’s functional ability is also important.
Ongoing Assessment
Ongoing assessment of patients taking cholinesterase inhibitors includes both mental and physical assessments. Cognitive and functional abilities are assessed routinely for changes. Initial assessments will be compared with the ongoing assessments to monitor the patient’s improvement (if any) after taking the cholinesterase inhibitors.
Using standardized tools to obtain an accurate description of the patient’s behavior and cognitive ability aids the primary health care provider in planning therapy and thus becomes an important part of patient management. Patients with poor response to drug therapy may require dosage changes, discontinuation of the drug therapy, or the addition of other therapies to the treatment regimen. However, response to these drugs may take several weeks. The symptoms that the patient is experiencing may improve or remain the same, or the patient may experience only a small response to therapy. It is important to remember that a treatment that slows the progression of symptoms in AD is a successful treatment.
NURSING DIAGNOSES
Drug-specific nursing diagnoses include the following:
 Imbalanced Nutrition: Less Than Body Requirements related to anorexia, nausea, or vomiting
Imbalanced Nutrition: Less Than Body Requirements related to anorexia, nausea, or vomiting
 Risk for Injury related to dizziness, syncope, clumsiness, or the disease process
Risk for Injury related to dizziness, syncope, clumsiness, or the disease process
Nursing diagnoses related to drug administration are discussed in Chapter 4.
PLANNING
The expected outcomes for the patient may include an optimal response to drug therapy, meeting patient needs related to the management of adverse reactions, an absence of injury, and confidence in an understanding of the medication regimen.
IMPLEMENTATION
Promoting an Optimal Response to Therapy
As you develop a care plan to meet the patient’s individual needs, keep in mind this is a progressive disease. When the drugs no longer provide memory enhancement, environmental factors may need to change rather than modifying the patient’s behavior.
If the patient is hospitalized, it is important to monitor vital signs and other assessments to determine if changes may be from the dementia or if the patient is experiencing delirium (acute confusion) due to reversible causes (see Display 19.2).
 NURSING ALERT
NURSING ALERT
Should cholinesterase inhibitor therapy be discontinued, individuals lose any benefit they have received from the drugs within 6 weeks.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree