DRUG CLASSES
Anticholinergics
Cholinergic blocking urinary antispasmodics
Anti-Parkinson cholinergic blocking
Respiratory cholinergic blocking
Like adrenergic blocking drugs, the cholinergic blocking drugs have an effect on the autonomic nervous system. Cholinergic blocking drugs are also called anticholinergic drugs, cholinergic blockers, or parasympatholytic drugs.
Acetylcholine (ACh) is the primary neurotransmitter in the parasympathetic branch of the autonomic nervous system. Cholinergic blocking drugs block the action of the neurotransmitter ACh in the parasympathetic nervous system. Because parasympathetic nerves influence many areas of the body, the effects of the cholinergic blocking drugs are numerous.
Actions
Cholinergic blocking drugs inhibit the activity of ACh at the parasympathetic nerve synapse. When the activity of ACh is inhibited, impulses traveling along the parasympathetic nerve cannot pass from the nerve ending to the effector organ or structure.
PHARMACOLOGY IN PRACTICE

Mr. Park is in the perioperative area having just been given his preoperative medications for hip surgery. He is very concerned about the function of his bladder and bowels. His stomach feels “rumbly” and he is very concerned that he will be incontinent of stool in the bed. After reading this chapter, decide whether his concerns are valid.
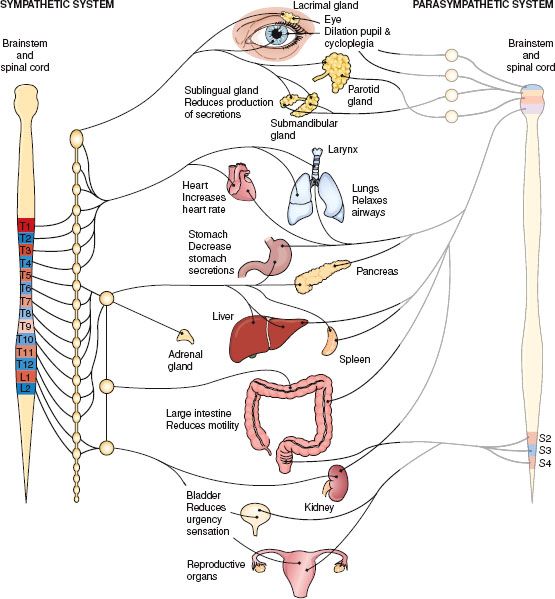
Figure 27.1 Action on body organs and structures when the parasympathetic nervous system is blocked. (From Cohen, B. J. [2003]. Medical terminology [4th ed.]. Philadelphia: Lippincott Williams & Wilkins.)
Two types of receptors are found in the parasympathetic nerve branch: muscarinic and nicotinic receptors. Cholinergic blocking drugs can specifically target one of these types of receptors. For example, antispasmodic drugs used to treat an overactive urinary bladder work by inhibiting the action of the muscarinic receptors in the parasympathetic nervous system. As a result, the detrusor muscle of the bladder does not contract, which prevents the sensations of urinary urgency. Yet, an antispasmodic drug has no effect on skeletal muscles, because it does not inhibit the nicotinic receptors in the parasympathetic nervous system.
Because of the wide distribution of parasympathetic nerves, some of these drugs that inhibit nerve impulses at both muscarinic and nicotinic receptors affect many organs and structures of the body, including the eyes, the respiratory and gastrointestinal (GI) tracts, the heart, and the bladder (Fig. 27.1).
However, responses to administration of a cholinergic blocking drug vary and often depend on the drug and the dose used. For example, scopolamine may occasionally cause excitement, delirium, and restlessness. This reaction is considered a drug idiosyncrasy (an unexpected or unusual drug effect).
Uses
The primary uses of cholinergic blocking drugs are in the treatment of the following:
• Pylorospasm and peptic ulcer
• Ureteral or biliary colic and bladder overactivity
• Vagal nerve–induced bradycardia
• Parkinsonism
In addition, the cholinergic blocking drugs are administered for the preoperative reduction of oral secretions. The Summary Drug Table: Cholinergic Blocking Drugs lists the uses of specific cholinergic blocking drugs.
Adverse Reactions
The severity of many adverse reactions is often dose dependent—that is, the larger the dose, the more intense the adverse reaction. Bodily system adverse reactions that may occur with the administration of a cholinergic blocking drug are listed in the following sections.
Gastrointestinal System Reactions
• Dry mouth, nausea, vomiting
• Difficulty in swallowing, heartburn
• Constipation
Central Nervous System Reactions
• Headache, flushing, nervousness
• Drowsiness, weakness, insomnia
• Nasal congestion, fever
Visual Reactions
• Blurred vision
• Mydriasis (dilation of the pupil)
• Photophobia
• Cycloplegia (paralysis of accommodation or inability to focus the eye)
• Increased ocular tension
Genitourinary System Reactions
• Urinary hesitancy and retention
• Dysuria
Cardiovascular System Reactions
• Palpitations
• Bradycardia (after low doses of atropine)
• Tachycardia (after higher doses of atropine)
Other Reactions
• Urticaria
• Decreased sweat production
• Anaphylactic shock
• Rash
Sometimes a secondary adverse reaction, such as drowsiness, is desirable. For example, when atropine is used before surgery to reduce the production of secretions in the respiratory tract, drowsiness is part of the desired response.
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Gerontology
Older patients receiving a cholinergic blocking drug may exhibit symptoms such as excitement, agitation, mental confusion, drowsiness, urinary retention, or other adverse effects. These effects may be seen even with small doses. If any should occur, withhold the next dose of the drug and contact the primary health care provider.
During hot summer months, patients receiving a cholinergic blocking drug should be instructed to watch for signs of heat prostration (e.g., fever; tachycardia; flushing; warm, dry skin; mental confusion) because these drugs decrease sweating.
Contraindications
Cholinergic blocking drugs are contraindicated in patients with known hypersensitivity to the drugs or glaucoma. Other patients for whom cholinergic blocking drugs are contraindicated are those with myasthenia gravis, tachyarrhythmias, myocardial infarction, and heart failure (unless bradycardia is present).
Precautions
These drugs are used with caution in patients with GI infections, benign prostatic hypertrophy, urinary retention, hyperthyroidism, hepatic or renal disease, and hypertension. Use atropine with caution in patients with asthma. Cholinergic blocking drugs are classified as pregnancy category C drugs and are used only when the benefit to the woman outweighs the risk to the fetus.
This caution also applies to over-the-counter (OTC) preparations available for the relief of allergy and cold symptoms and as aids to induce sleep. Some of these products contain atropine, scopolamine, or other cholinergic blocking drugs. Although this warning is printed on the container or package, many users fail to read drug labels carefully.
Interactions
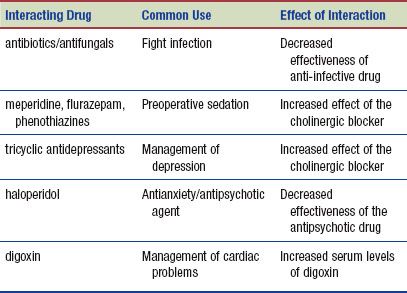
The following interactions may occur when a cholinergic blocking drug is administered with another agent:
NURSING PROCESS
PATIENT TEACHING FOR MEDICATION INFORMATION
ASSESSMENT
Preadministration Assessment
Before administering a cholinergic blocking drug to a patient for the first time, obtain a thorough health history as well as a history of the signs and symptoms of the current disorder. The focus of the initial physical assessment depends on the reason for administering the drug. In most instances, obtain the blood pressure, pulse, and respiratory rate. Additional assessments may include checking the stool of the patient who has a peptic ulcer for color and signs of occult blood, determining visual acuity in the patient with glaucoma, and looking for signs of dehydration and weighing the patient if prolonged diarrhea is one of the patient’s symptoms.
Ongoing Assessment
When administering a cholinergic blocking drug, check vital signs, observe for adverse drug reactions, and evaluate the symptoms and complaints related to the patient’s diagnosis. For example, question the patient with a peptic ulcer regarding current symptoms, and then make a comparison of these symptoms with the symptoms present before the start of therapy. Document any increase in the severity of symptoms and notify the primary health care provider.
NURSING DIAGNOSES
Drug-specific nursing diagnoses include:
 Impaired Comfort related to xerostomia
Impaired Comfort related to xerostomia
 Constipation related to slowing of peristalsis in the GI tract
Constipation related to slowing of peristalsis in the GI tract
 Risk for Injury related to dizziness, drowsiness, mental confusion, impaired vision, or heat prostration
Risk for Injury related to dizziness, drowsiness, mental confusion, impaired vision, or heat prostration
 Ineffective Tissue Perfusion related to impaired heart pumping action
Ineffective Tissue Perfusion related to impaired heart pumping action
Nursing diagnoses related to drug administration are discussed in Chapter 4.
PLANNING
The expected outcomes for the patient depend on the reason for administration of a cholinergic blocking drug but may include an optimal response to therapy, meeting patient needs related to the management of adverse reactions, and confidence in an understanding of and adherence to the prescribed medication regimen.
IMPLEMENTATION
Promoting an Optimal Response to Therapy
If a cholinergic blocking drug is administered before surgery, be sure to give it at the exact time prescribed because the drug must be given time to produce the greatest effect (i.e., the drying of upper respiratory and oral secretions) before the administration of a general anesthetic. Before administration, instruct the patient to void. Inform the patient and family members that drowsiness and extreme dryness of the mouth and nose will occur about 20 to 30 minutes after the drug is given. This is normal, and fluid is not to be taken. The side rails of the bed are raised, and the patient is instructed to remain in bed after administration of the preoperative drug.
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Gerontology
Cholinergic blocking drugs are usually not included in the preoperative drugs of patients older than 60 years because of the effects of these drugs on the eye and the central nervous system.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree