DRUG CLASSES
Alpha (α)-adrenergic blocking
Beta (β)-adrenergic blocking
α/β-adrenergic blocking
Centrally and peripherally acting antiadrenergic
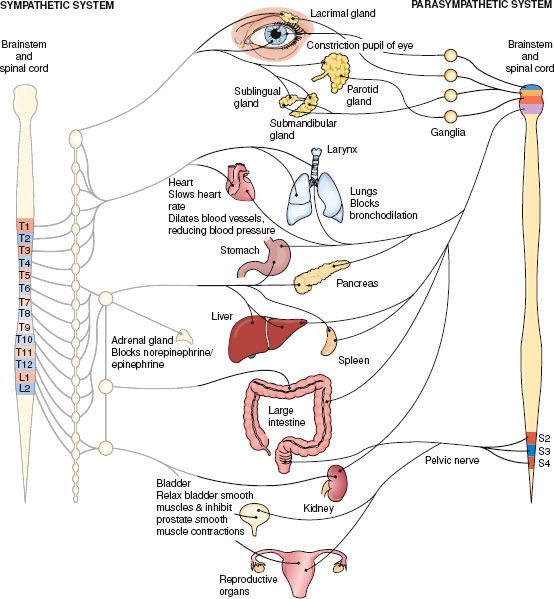
Norepinephrine is a substance that transmits nerve impulses across the sympathetic branch of the autonomic nervous system. Activation of these nerves is sometimes called our fight-or-flight response. Drugs featured in Chapter 24 facilitate the transmission of norepinephrine. In this chapter drugs that prevent the response, called adrenergic blocking, are discussed. Figure 25.1 shows the organ responses when sympathetic nerve impulses are blocked. Also called sympatholytic drugs, these agents block the transmission of norepinephrine in the sympathetic system. Drugs blocking neurotransmission in the sympathetic nervous system work directly by blocking the receptor or indirectly by preventing release of norepinephrine. They may be viewed as belonging to one of four different groups:
PHARMACOLOGY IN PRACTICE

Alfredo Garcia is accompanied by his wife to the clinic. He came in with complaints of an upper respiratory infection. While taking vital signs you discover a blood pressure of 210/120. He has never been diagnosed with hypertension. As you read, think about what antiadrenergic drugs do to blood vessels and blood pressure.
Figure 25.1 Action on body organs and structures when the sympathetic nervous system is blocked. (Adapted from Cohen, B. J. [2003]. Medical terminology [4th ed.]. Philadelphia: Lippincott Williams & Wilkins.)
• Alpha (α)-adrenergic blocking drugs—drugs that block α-adrenergic receptors. These drugs produce their greatest effect on the α receptors of the adrenergic nerves that control the vascular system.
• Beta (β)-adrenergic blocking drugs—drugs that block β-adrenergic receptors. These drugs produce their greatest effect on the β receptors of adrenergic nerves, primarily the β receptors of the heart.
• α/β-Adrenergic-blocking drugs—drugs that block both α- and β-adrenergic receptors. These drugs act on both α and β nerve fibers.
• Centrally and peripherally acting antiadrenergic drugs—drugs that prevent the release of the neurotransmitter. These drugs block the adrenergic nerve impulse in both the central and peripheral nervous systems.
Each of these groups is discussed individually, followed by an example of the Nursing Process for the group as a whole. The focal group of drugs in this chapter is the β-adrenergic blocking drugs. See the Summary Drug Table: Adrenergic Blocking Drugs for a more complete listing of these drugs.
α-ADRENERGIC BLOCKING DRUGS
Actions
Stimulation of α-adrenergic nerves results in vasoconstriction. If stimulation of α-adrenergic nerves is interrupted or blocked, the result is vasodilation. This is the direct opposite of the effect of an adrenergic drug with α activity. The drug used in this category causes vasodilation by relaxing the smooth muscle of blood vessels. α-Adrenergic blockers used in ophthalmic preparations constrict the pupil and are discussed in Chapter 53.
Uses
α-Adrenergic blocking drugs are used in the treatment of the following:
• Hypertension caused by pheochromocytoma (a tumor of the adrenal gland that produces excessive amounts of epinephrine and norepinephrine)
• Hypertension during preoperative preparation
They are also used to prevent or treat tissue damage caused by extravasation of dopamine.
Adverse Reactions
Administration of an α-adrenergic blocking drug may result in weakness, orthostatic hypotension, cardiac arrhythmias, hypotension, and tachycardia. See the Summary Drug Table: Adrenergic Blocking Drugs for more information.
Contraindications, Precautions, and Interactions
α-Adrenergic blocking drugs are contraindicated in patients who are hypersensitive to the drugs and in patients with coronary artery disease. These drugs are used cautiously during pregnancy (pregnancy category C) and lactation, after a recent myocardial infarction (MI), and in patients with renal failure or Raynaud’s disease. When phentolamine (Regitine) is administered with epinephrine, there is decreased vasoconstrictor and hypertensive action.
β-ADRENERGIC BLOCKING DRUGS
Actions
β-Adrenergic blocking drugs are also called β blockers. These drugs decrease the stimulation of the sympathetic nervous system on certain tissues. β-Adrenergic receptors are found mainly in the heart. Stimulation of β receptors of the heart results in an increase in the heart rate. Blocking the nerve impulse of β-adrenergic nerves decreases the heart rate and dilates the blood vessels (Fig. 25.2). These drugs decrease the heart’s excitability, decrease cardiac workload and oxygen consumption, and provide membrane-stabilizing effects that contribute to the antiarrhythmic activity of the β-adrenergic blocking drugs. Examples of β-adrenergic blocking drugs used for cardiac purposes are esmolol (Brevibloc) and propranolol (Inderal).
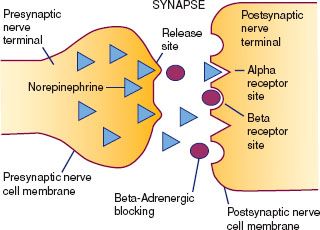
Figure 25.2 β-Adrenergic blocking drugs prevent epinephrine and norepinephrine from occupying receptor sites on cell membranes.
β-Adrenergic blocking drugs such as betaxolol (Betoptic) and timolol (Timoptic) are used to treat glaucoma. Glaucoma is a narrowing or blockage of the drainage channels (canals of Schlemm) between the anterior and posterior chambers of the eye. This results in a buildup of pressure (increased intraocular pressure) in the eye. Blindness may occur if glaucoma is left untreated. When the aforementioned drugs are used topically as ophthalmic drops, they appear to reduce the production of aqueous humor in the anterior chamber of the eye, lessening the effects of glaucoma.
Uses
β-Adrenergic blocking drugs are used in the treatment of the following:
• Hypertension (first-choice drug for patients with stable angina)
• Cardiac arrhythmia (abnormal rhythm of the heart), such as ventricular or supraventricular tachycardia
• Migraine headaches
• Heart failure (HF)
• Angina pectoris
• Glaucoma (topical ophthalmic eye drops)
β-Adrenergic blockers are also used to prevent reinfarction in patients with a recent MI (1 to 4 weeks after the MI).
 CHRONIC CARE CONSIDERATIONS
CHRONIC CARE CONSIDERATIONS
Hypertension research studies demonstrate better patient outcomes for African Americans when β blockers are used in combination with diuretics than other drugs alone to treat hypertension, such as angiotensin-converting enzyme (ACE) inhibitors (Ferdinand, 2007).
Adverse Reactions
• Cardiac reactions that affect the body in a generalized manner include orthostatic hypotension, bradycardia, dizziness, vertigo, and headache.
• Gastrointestinal (GI) reactions include hyperglycemia, nausea, vomiting, and diarrhea.
• Another bodily system reaction is bronchospasm (especially in those with a history of asthma).
Many of these reactions are mild and may disappear with therapy. More serious adverse reactions include symptoms of HF (i.e., dyspnea, weight gain, peripheral edema).
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Gerontology
Older adults are at increased risk for adverse reactions when taking β-adrenergic blocking drugs. Monitor the older adult closely for confusion, HF, worsening of angina, shortness of breath, and peripheral vascular insufficiency (e.g., cold extremities, paresthesia of the hands, weak peripheral pulses).
Contraindications, Precautions, and Interactions
These drugs are contraindicated in patients with an allergy to β blockers; in patients with sinus bradycardia, second- or third-degree heart block, or HF; and in those with asthma, emphysema, and hypotension. The drugs are used cautiously in patients with diabetes, thyrotoxicosis, or peptic ulcer.
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Pregnancy
β Blockers are recommended for pregnant women over other hypertensive drugs because the risk to the fetus is less with these drugs.
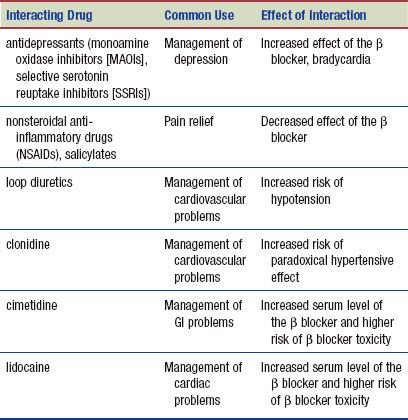
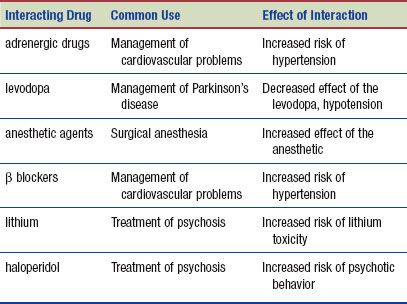
The following interactions may occur when a β-adrenergic blocker is administered with another agent:
α/β-ADRENERGIC BLOCKING DRUGS
Actions
α/β-Adrenergic blocking drugs block the stimulation of both the α- and β-adrenergic receptors, resulting in peripheral vasodilation. The two drugs in this category are carvedilol (Coreg) and labetalol (Trandate).
Uses
Carvedilol is used to treat essential hypertension and in HF to reduce progression of the disease. Labetalol is used in the treatment of hypertension, either alone or in combination with another drug, such as a diuretic.
Adverse Reactions
Most adverse effects of α/β-adrenergic blocking drugs are mild and do not require discontinuation of therapy. General body system adverse reactions include fatigue, dizziness, hypotension, drowsiness, insomnia, weakness, diarrhea, dyspnea, chest pain, bradycardia, and skin rash.
Contraindications, Precautions, and Interactions
α/β-Adrenergic blockers are contraindicated in patients with hypersensitivity to the drugs, bronchial asthma, decompensated HF, and severe bradycardia. The drugs are used cautiously in patients with drug-controlled HF, chronic bronchitis, or impaired hepatic or cardiac function; in those with diabetes; and during pregnancy (pregnancy category C) and lactation.
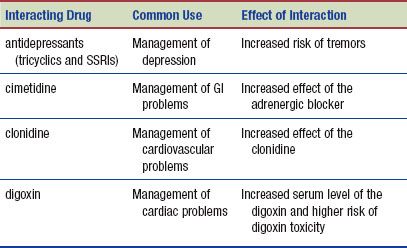
The following interactions may occur when an α/β-adrenergic blocker is administered with another agent:
CENTRALLY AND PERIPHERALLY ACTING ANTIADRENERGIC DRUGS
Actions
One group of antiadrenergic drugs inhibits the release of norepinephrine from certain adrenergic nerve endings in the peripheral nervous system. This group is composed of peripherally acting (i.e., acting on peripheral structures) antiadrenergic drugs. An example of a peripherally acting antiadrenergic drug for treating hypertension is prazosin (Minipress). These drugs are also used to treat benign prostatic hypertrophy (BPH). Another group of antiadrenergic drugs are called centrally acting antiadrenergic drugs because they act on the central nervous system (CNS) rather than on the peripheral nervous system. This group affects specific CNS centers, thereby decreasing some of the activity of the sympathetic nervous system. Although the action of both types of antiadrenergic drugs is somewhat different, the results are basically the same. An example of a centrally acting antiadrenergic drug is clonidine (Catapres).
Uses
Antiadrenergic drugs are used mainly for the treatment of certain cardiac arrhythmias, hypertension, and BPH (see the Summary Drug Table: Adrenergic Blocking Drugs).
Adverse Reactions
• Dry mouth, drowsiness, sedation, anorexia, rash, malaise, and weakness are generalized reactions to antiadrenergic drugs that work on the CNS.
• Hypotension, weakness, lightheadedness, and bradycardia are adverse reactions associated with the administration of peripherally acting antiadrenergic drugs.
Contraindications, Precautions, and Interactions
Centrally acting antiadrenergic drugs are contraindicated in active hepatic disease, in antidepressant therapy using MAOIs, and in patients with a history of hypersensitivity to these drugs. The centrally acting antiadrenergic drugs are used cautiously in patients with a history of liver disease or renal impairment and during pregnancy and lactation.
The peripherally acting antiadrenergic drugs are contraindicated in patients with a hypersensitivity to any of the drugs. Reserpine (Serpasil) is contraindicated in patients who have an active peptic ulcer or ulcerative colitis and in patients who are mentally depressed. Reserpine is used cautiously in patients with a history of depression, in those with renal impairment or cardiovascular disease, and during pregnancy and lactation.
The following interactions may occur when an antiadrenergic drug is administered with another agent:
NURSING PROCESS
PATIENT TEACHING FOR MEDICATION INFORMATION
ASSESSMENT
Assessment depends on the drug, the patient, and the reason for administration.
Preadministration Assessment
Establish an accurate database before any adrenergic blocking drug is administered for the first time. If, for example, the patient has hypertensive disease, document the subjective and objective symptoms as well as vital signs during the initial assessment. Patients with hypertension have their blood pressure and pulse taken on both arms in sitting, standing, and supine positions before therapy is begun. If the patient has a cardiac arrhythmia, the initial assessment includes taking the pulse rate, determining the pulse rhythm, and noting the patient’s general appearance.
If the drug is given for anginal pain, document the pain experience of the patient, and ask about the onset, type (e.g., sharp, dull, squeezing), radiation, location, intensity, and duration of anginal pain. Ask about any precipitating factors of the anginal pain, such as exertion or emotional stress. Once drug therapy is started, evaluation of the effects of therapy can be made by comparing the patient’s current symptoms with the symptoms experienced before therapy was initiated. Additional diagnostic studies and laboratory tests, such as an electrocardiogram, also may be ordered.
If the drug is given to treat HF, the patient is assessed for evidence of the disease, such as dyspnea (especially on exertion), peripheral edema, distended neck veins, and cough.
Ongoing Assessment
It is important to perform an ongoing assessment of the patient receiving adrenergic blocking drug therapy. This assessment often depends on the reason the drug is administered. For all adrenergic blocking drugs, it is important to observe these patients continually for the appearance of adverse reactions. Some adverse reactions are mild, whereas others, such as diarrhea, may cause a problem, especially if the patient is older or debilitated.
Typically hypertensive patients will be asked to monitor their own blood pressures between clinic visits. This can be accomplished by obtaining equipment for the home or periodic visits to a local fire station or pharmacy. More in-depth information regarding care of the patient with hypertension is provided in Chapter 35.
Drug-specific nursing diagnoses are the following:
 Impaired Comfort related to drying of secretions secondary to medication
Impaired Comfort related to drying of secretions secondary to medication
 Ineffective Tissue Perfusion: Peripheral related to hypotension
Ineffective Tissue Perfusion: Peripheral related to hypotension
 Risk for Injury related to vertigo, dizziness, weakness, and syncope secondary to hypotension
Risk for Injury related to vertigo, dizziness, weakness, and syncope secondary to hypotension
Nursing diagnoses related to drug administration are discussed in Chapter 4.
PLANNING
The expected outcomes for the patient depend on the reason for administration of an adrenergic blocking drug but may include an optimal response to drug therapy, meeting of patient needs related to the management of adverse reactions, and confidence in an understanding of the medication regimen.
IMPLEMENTATION
Promoting an Optimal Response to Therapy
Most adrenergic blocking drugs may be given without regard to food. However, the drugs preventing release of neurotransmitters (antiadrenergics) should be taken at the same time each day because the fluctuation in blood level can affect blood pressure. Sotalol (Betapace) is given on an empty stomach because food may reduce absorption of the drug.
When adrenergic blocking drugs are given to patients to control hypertension, angina, or cardiac arrhythmias, it is important to communicate with the primary health care provider about the patient’s response to therapy. When given for a cardiac arrhythmia, these drugs can provoke new or worsen existing ventricular arrhythmias. If angina worsens or does not appear to be controlled by the drug, the patient needs to feel confident to contact the primary health care provider immediately.
When the drug is administered for hypertension, the patient is monitored for a decrease in blood pressure. On the other hand, if there is a significant increase in blood pressure, administer the ordered dose and notify the primary health care provider immediately because additional drug therapy may be necessary.
When a β-adrenergic blocking ophthalmic preparation, such as timolol, is used by patients with glaucoma, it is important they continue periodic follow-up examinations with an ophthalmologist. At these examinations, the intraocular pressure is measured to determine the effectiveness of drug therapy.
Monitoring and Managing Patient Needs
IMPAIRED COMFORT. Some patients may experience one or more adverse drug reactions during treatment with adrenergic blocking drugs. Adverse reactions that pose no serious threat to the patient’s well-being, such as dry mouth or mild constipation, are reactions that impair comfort.
Even minor adverse drug reactions can be distressing to the patient, especially when they persist for a long time. Therefore, when possible, you can relieve minor adverse reactions with simple nursing measures. For example, assist or teach the patient with dry mouth to take frequent sips of water or suck on a piece of hard candy (provided that the patient does not have diabetes or is not on a special diet that limits sugar intake) to relieve the dryness. Help relieve a patient’s constipation by encouraging increased intake of high-fiber foods and fluids, unless extra fluids are contraindicated. The primary health care provider also may order a laxative or stool softener. It is important for you to maintain a daily record of bowel elimination for the hospitalized patient. Dryness, slower GI motility, and immobility all make constipation a greater risk for the hospitalized patient. Other GI side effects, such as anorexia, diarrhea, and constipation, can be minimized by administering drugs at a specific time in relation to meals, with food, or with antacids.
INEFFECTIVE TISSUE PERFUSION: PERIPHERAL. During therapy with an adrenergic blocking drug for hypertension, the patient’s blood pressure is taken before each dose is given. Some patients have an unusual response to the drugs. In addition, some drugs may, in some individuals, decrease the blood pressure at a more rapid rate than other drugs. It is important to monitor the patient’s blood pressure on both arms and in the sitting, standing, and supine positions for the first week or more of therapy. Once the patient’s blood pressure has stabilized, take the blood pressure before each drug administration using the same arm and position for each reading until the patient is ready to return home. It is a good idea to make a notation on the medication administration record or care plan about the position and arm used for blood pressure determinations. Measuring the blood pressure near the end of the dosing interval or near the end of the day after the last dose of the day helps to determine if the blood pressure is controlled throughout the day.
 NURSING ALERT
NURSING ALERT
When administering a sympatholytic drug, such as propranolol (Inderal), take an apical pulse rate and blood pressure before giving the drug. If the pulse is below 60 beats/min, or if there is any irregularity in the patient’s heart rate or rhythm, or if systolic blood pressure is less than 90 mm Hg, withhold the drug and contact the primary health care provider.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree