Figure 33–1 Biosynthetic pathways for adrenal steroids. (A) Major pathways for mineralocorticoid, glucocorticoid, and androgen biosynthesis are shown. Important enzymes include 3β-hydroxysteroid dehydrogenase (3β-HSD), steroid 21-hydroxylase (P45021), steroid 11β-hydroxylase (P45011β), aldosterone synthase (P450aldo), steroid 17α-hydroxylase (P45017α), and 17β-hydroxysteroid dehydrogenase (17β-HSD). The structural changes produced by each reaction are unshaded. Aminoglutethimide blocks the synthesis of all adrenal steroids by inhibiting the conversion of cholesterol to pregnenolone. Ketoconazole and metyrapone inhibit P45011β. The most common defect causing congenital adrenal hyperplasia is P45021 deficiency. (B) The structure of dexamethasone is shown by the inset in lower right corner. In the synthetic steroids, glucocorticoid potency is enhanced by the introduction of a double bond at the 1,2 position or the introduction of a hydroxyl or methyl group at the 16 position. Both glucocorticoid and mineralocorticoid activities are increased by a fluorine substitution at the 9 position.
The regulation of corticosteroid secretion is depicted in Figure 33–2. The secretion of cortisol and adrenal androgens is primarily controlled by corticotropin (ACTH) secreted by the pituitary gland, whereas the secretion of aldosterone is chiefly regulated by the renin-angiotensin system. Various types of physical and mental stress are powerful activators of corticotropin-releasing hormone secretion, leading to increased corticotropin and cortisol production. Cortisol exerts several effects that increase the body’s resistance to stress.
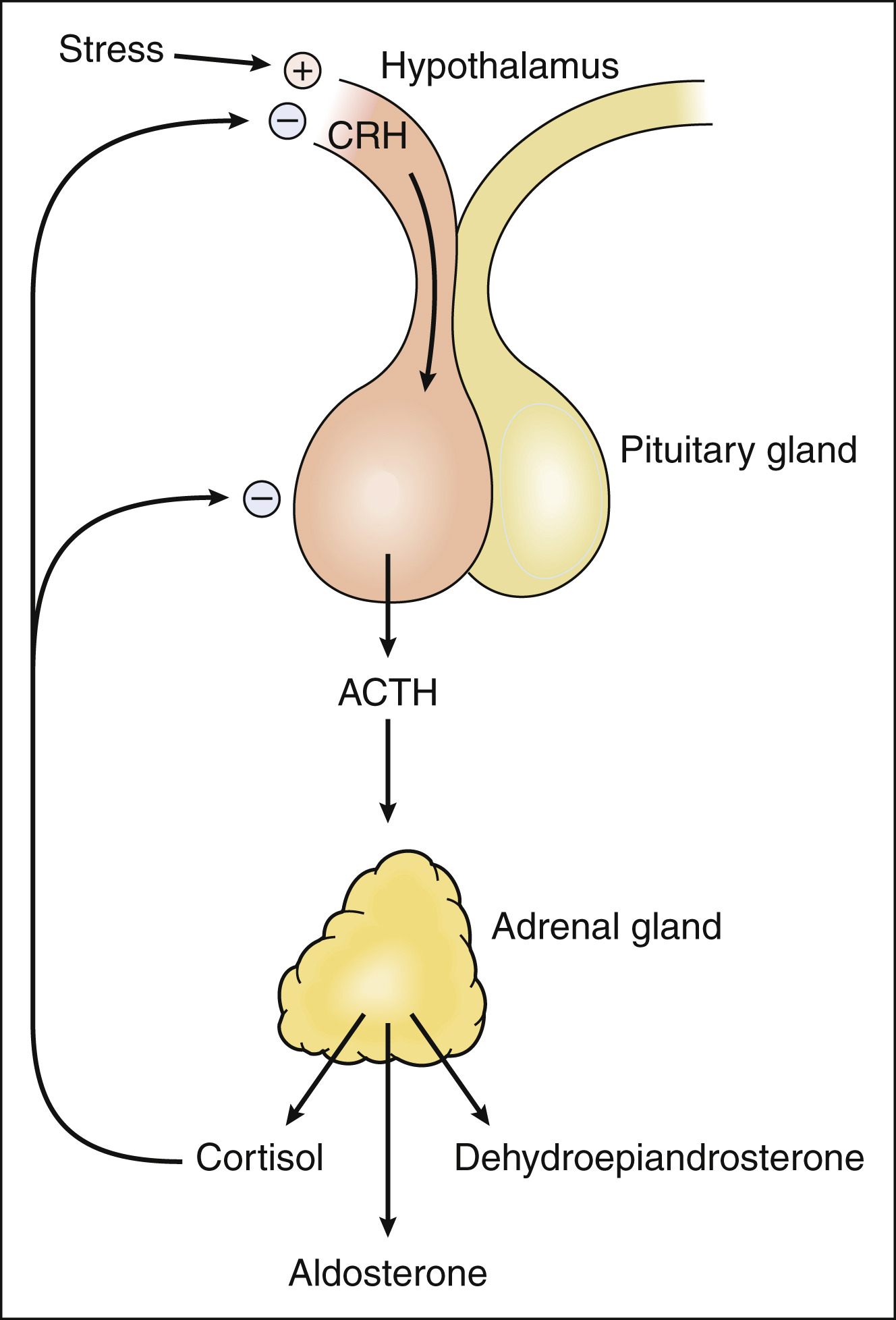
Figure 33–2 Regulation of the secretion of cortisol by the adrenal cortex. Stress and other stimuli increase the release of corticotropin-releasing hormone (CRH) from hypothalamic paraventricular nuclei, and CRH is carried by hypophysioportal vessels to the anterior pituitary, where it stimulates the release of corticotropin (ACTH). Corticotropin acts on the adrenal cortex to increase the release of adrenal steroids, although the release of aldosterone is primarily regulated by the renin-angiotensin system. Cortisol exerts feedback inhibition on the hypothalamus and pituitary to inhibit the release of CRH and corticotropin.
As shown in Figure 33–2, cortisol and other glucocorticoids act as feedback inhibitors of both corticotropin-releasing hormone and corticotropin. This is why exogenously administered glucocorticoids can suppress the hypothalamic-pituitary-adrenal axis and inhibit endogenous cortisol production, leading to adrenal insufficiency when the exogenous glucocorticoid is withdrawn.
PHYSIOLOGIC EFFECTS OF ADRENAL STEROIDS
The adrenal steroids act on target tissues by binding to specific cytoplasmic steroid receptors, which are then translocated to the cell nucleus, a common mechanism for all steroid hormones (see Fig. 3–4 in Chapter 3). In the nucleus, the activated receptors stimulate the transcription of specific genes and thereby increase the translation of specific proteins. These actions lead to the various metabolic and anti-inflammatory effects of glucocorticoids, which are described below. In the renal tubules, activation of the mineralocorticoid receptor stimulates the synthesis of sodium channels and the sodium-potassium adenosine triphosphatase that are needed for sodium reabsorption. This mechanism is responsible for the salt-retaining effects of mineralocorticoids.
The glucocorticoid receptor has a high affinity for cortisol but a much lower affinity for aldosterone, whereas the mineralocorticoid receptor has a high affinity for both aldosterone and cortisol. This enables cortisol to exert both glucocorticoid and mineralocorticoid actions.
Glucocorticoids induce enzymes involved in gluconeogenesis (the formation of glucose from amino acids) and have an anti-insulin effect. For this reason, glucocorticoid insufficiency can lead to hypoglycemia during stress. Glucocorticoids also activate enzymes involved in protein catabolism, thereby increasing the supply of amino acids needed for gluconeogenesis. Glucocorticoids stimulate lipolysis and inhibit the uptake of glucose by adipose tissue. By this mechanism, excessive glucocorticoid levels can lead to abnormal fat distribution and muscle wasting (see below).
CORTICOSTEROID DRUGS
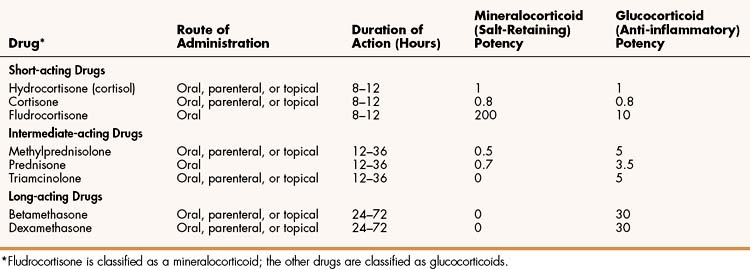
A large number of semisynthetic glucocorticoid drugs are available; they are most frequently employed to attain the anti-inflammatory effects produced by supra-physiologic doses of these drugs. Less commonly, corticosteroids are used as replacement therapy in the treatment of adrenal insufficiency and in the treatment of adrenogenital syndromes that produce excessive quantities of adrenal androgens and insufficient quantities of other corticosteroids. Mineralocorticoids are primarily used as replacement therapy in persons with adrenal insufficiency. The properties of selected corticosteroids are listed in Table 33–1.
MINERALOCORTICOIDS
Aldosterone, the major mineralocorticoid in humans, is not suitable for clinical use due to the potential for electrolyte disturbances. Fludrocortisone is a mineralocorticoid that is used as replacement therapy in patients with primary adrenal insufficiency (Addison’s disease). The drug’s salt-retaining potency is about 20 times greater than its anti-inflammatory potency.
GLUCOCORTICOIDS
A large number of glucocorticoid preparations are available for oral, parenteral, inhalational, or topical administration for the treatment of a wide range of inflammatory, allergic, autoimmune, and other disorders. Whenever possible, topical or inhalational administration is preferred because it is usually well tolerated and avoids most systemic adverse effects. Topical administration is widely used in the treatment of allergic or inflammatory conditions affecting the skin (see below), mucous membranes, or eyes. For example, topical ocular glucocorticoids are used to treat acute uveitis (inflammation of the iris, ciliary body, or choroid). Glucocorticoids are given by inhalation to treat allergic rhinitis, aspiration pneumonia, asthma, and other respiratory conditions (see Chapter 27).
CLASSIFICATION
The glucocorticoids are usually classified according to their potency and duration of action (see Table 33–1). When given systemically, the duration of action of glucocorticoids is primarily determined by their potency at the glucocorticoid receptor, rather than by their elimination half-life. This is because the highly potent drugs evoke a longer-lasting stimulation of gene transcription than do less potent glucocorticoids. The potency of specific topical corticosteroids is discussed under the treatment of dermatologic conditions (see below).
LOW POTENCY, SHORT-ACTING GLUCOCORTICOIDS
Cortisol, the major glucocorticoid in humans, is called hydrocortisone when used as a pharmaceutical. Hydrocortisone and cortisone have a duration of action of 8 to 12 hours, have equal glucocorticoid and mineralocorticoid effects, and are the preferred glucocorticoids when replacement therapy is needed for patients with adrenal insufficiency. These drugs are also used as anti-inflammatory agents, but more potent glucocorticoids are often preferred for treating most inflammatory, allergic, and autoimmune disorders.
Medium Potency, Intermediate-acting Glucocorticoids
Prednisone, prednisolone, methylprednisolone, and triamcinolone are the glucocorticoids used most often for systemic treatment. In the body, prednisone is rapidly converted to prednisolone, a substance that is itself available as a drug. The intermediate-acting glucocorticoids have a duration of action of 12 to 36 hours and are often used to treat cancer, inflammation, allergy, and autoimmune disorders.
High Potency, Long-acting Glucocorticoids
Betamethasone and dexamethasone are stereoisomers that differ only in the configuration of a methyl group. Betamethasone is available for systemic use, and it is also used in the topical treatment of a number of skin disorders, including psoriasis, seborrheic or atopic dermatitis, and neurodermatitis. Dexamethasone is used in diagnostic dexamethasone suppression tests and in the treatment of a variety of neoplastic, infectious, and other inflammatory conditions that require the use of a potent and long-acting drug. Budesonide is a long-acting glucocorticoid that is administered by inhalation.
Anti-inflammatory Effects
The anti-inflammatory effects of glucocorticoids are primarily attributable to their multiple actions on several types of leukocytes (Fig. 33–3). First, glucocorticoids suppress the activation of T lymphocytes by interleukins and nuclear factor kappaB (NF-кB), a transcription factor for pro-inflammatory cytokine genes. Second, they suppress the production of cytokines by activated helper T cells. Cytokines play a major role in inflammation by recruiting and activating eosinophils and by stimulating antibody production by B cells. Glucocorticoids inhibit the production of pro-inflammatory cytokines by increasing the transcription of a gene for a protein that blocks NF-кB, as above.
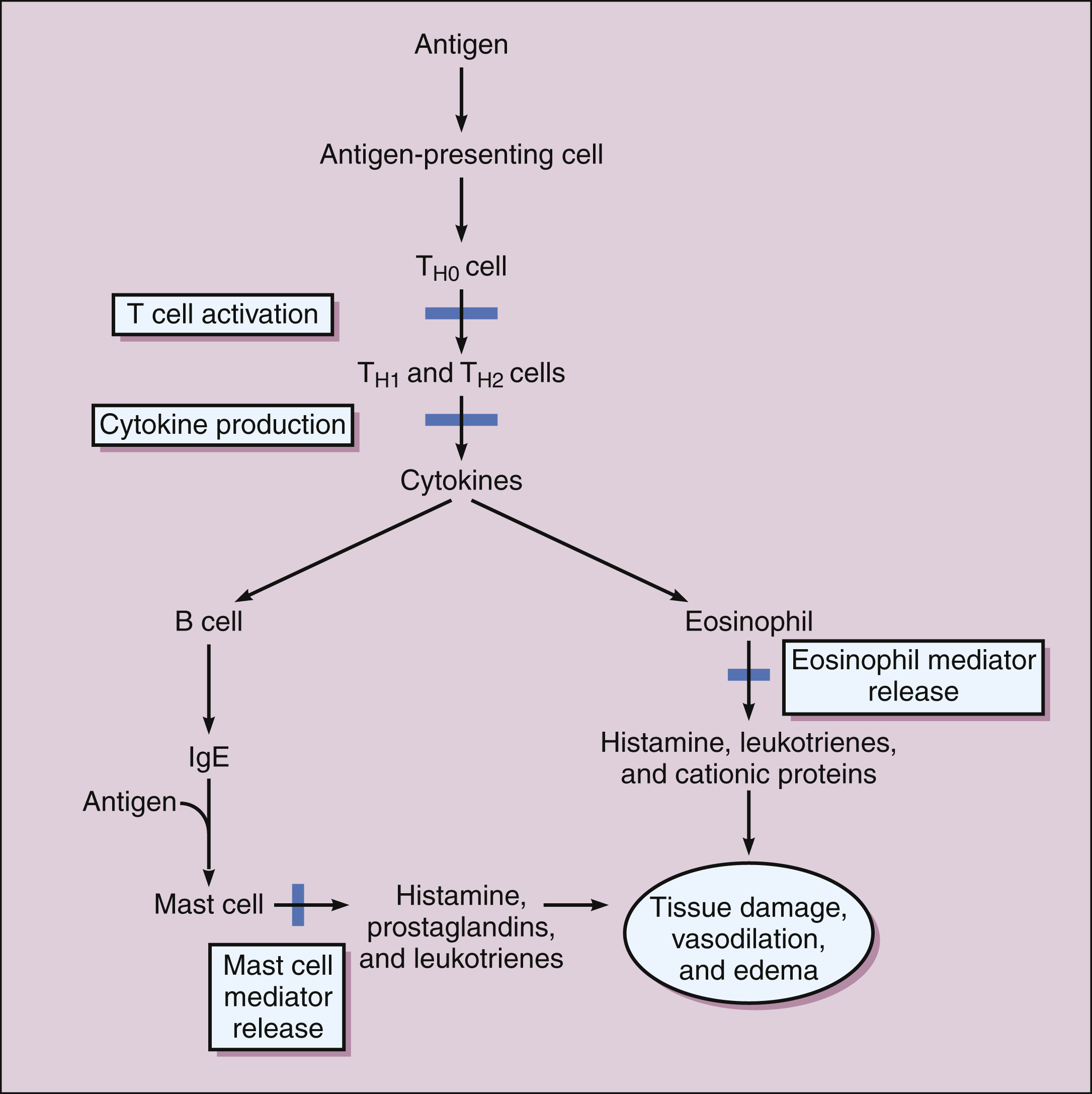
Figure 33–3 Anti-inflammatory actions of glucocorticoids. During the inflammatory process, undifferentiated helper T cells (TH0) become activated T cells (TH1 and TH2) and produce cytokines. In addition to stimulating antibody production by B cells, cytokines recruit and activate eosinophils. Glucocorticoids act by suppressing T-cell activation, suppressing cytokine production, and preventing mast cells and eosinophils from releasing various chemical mediators of inflammation, including histamine, prostaglandins, leukotrienes, and other substances that cause tissue damage, vasodilatation, and edema. Glucocorticoids have additional anti-inflammatory effects that are described in the text. IgE = immunoglobulin E.
Third, glucocorticoids decrease the release of various chemical mediators of inflammation, including histamine, prostaglandins, leukotrienes, and other substances from mast cells, eosinophils, and inflamed tissue. They decrease the synthesis of prostaglandins and leukotrienes by increasing the transcription of lipocortin which inhibits phospholipase A, the first step in the eicosanoid pathway (Chapter 26).
Fourth, glucocorticoids stabilize lysosomal membranes of neutrophils and prevent the release of catabolic enzymes (e.g., acid phosphatase) from these organelles; this limits cytotoxic effects of inflammation. Finally, glucocorticoids cause vasoconstriction and decrease capillary permeability by increased synthesis of lipocortin leading to decreased prostacyclin by the mechanism outlined above. They also decrease the synthesis of pro-inflammatory cytokines and other substances released from eosinophils in blood vessels as noted above, and both actions reduce the vasodilation and plasma extravasation that are the signs of inflammation.
Glucocorticoids also have multiple effects on circulating leukocytes. Pharmacological doses of glucocorticoids suppress lymphoid tissue and reduce the number of circulating lymphocytes. They also reduce the concentration of circulating eosinophils, basophils, and monocytes while at the same time increasing the concentration of erythrocytes, platelets, and polymorphonuclear leukocytes.
INDICATIONS
Glucocorticoids are used for the diagnosis and treatment of adrenal diseases and for the treatment of a diverse group of nonadrenal disorders.
INFLAMMATION, ALLERGY, AND AUTOIMMUNE DISORDERS
The glucocorticoids are frequently used to suppress inflammation and immune dysfunction associated with diseases affecting almost every organ in the body. Glucocorticoids counteract inflammation evoked by physical trauma, extreme temperatures, noxious chemicals, radiation damage, and microbial pathogens. They also suppress inflammation caused by allergic and autoimmune reactions and other disease states. Examples of diseases treated with corticosteroids include systemic lupus erythematosus, autoimmune thrombocytopenia purpura, polyarteritis nodosa, multiple sclerosis, ulcerative colitis, and polymyositis.
Several glucocorticoids, including beclomethasone, are available for nasal inhalation or oral inhalation to treat allergic rhinitis or asthma, respectively. Inhaled glucocorticoids are often first-line therapy for these disorders, and their administration and use are described in Chapter 27. Ciclesonide is a newer agent also indicated for “hayfever” or allergic rhinitis.
For corneal inflammation and keratitis, many glucocorticoids are available in eyedrops, including a new combination of loteprednol and the antibiotic tobramycin (Zylet). There are also combinations for the treatment of superficial bacterial infections of the external auditory canal (“swimmers ear”) containing hydrocortisone and neomycin (Cortisporin).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree