Urinary System Disorders
Learning Objectives
After studying this chapter, the student is expected to:
1. Compare the etiology, pathophysiology, and manifestations of cystitis and pyelonephritis.
3. Describe the etiology and significant manifestations of nephrotic syndrome.
4. Explain the common signs and symptoms of urinary tract obstruction.
5. List common causes of urinary calculi.
6. Explain how hydronephrosis develops and its effects on the kidney.
8. Explain how nephrosclerosis affects: (a) the kidney, and (b) systemic blood pressure.
9. Describe the etiology, usual age at onset, manifestations, and outcome of adult polycystic disease.
Key Terms
anasarca
anuria
azotemia
calculi
dialysate
dysuria
frequency
glucosuria
hematuria
nocturia
oliguria
osteodystrophy
polyuria
proteinuria
pyuria
renal colic
retroperitoneally
ultrafiltration
urgency
Review of the Urinary System
The functions of the urinary system are:
• Removal of metabolic wastes (nitrogenous and acidic)
• Removal of hormones, drugs, and other foreign material from the body
• Regulation of water, electrolytes, and acid-base balance in the body
• Regulation of blood pressure through the renin-angiotensin-aldosterone system
Structures and Anatomy
Kidneys
The two kidneys are bean-shaped structures, each the size of a fist, located behind the peritoneum (that is, retroperitoneally) on the posterior abdominal wall. The kidneys are covered by a fibrous capsule and are embedded in fat, with the superior portion also protected by the lower ribs (Fig. 18-1).
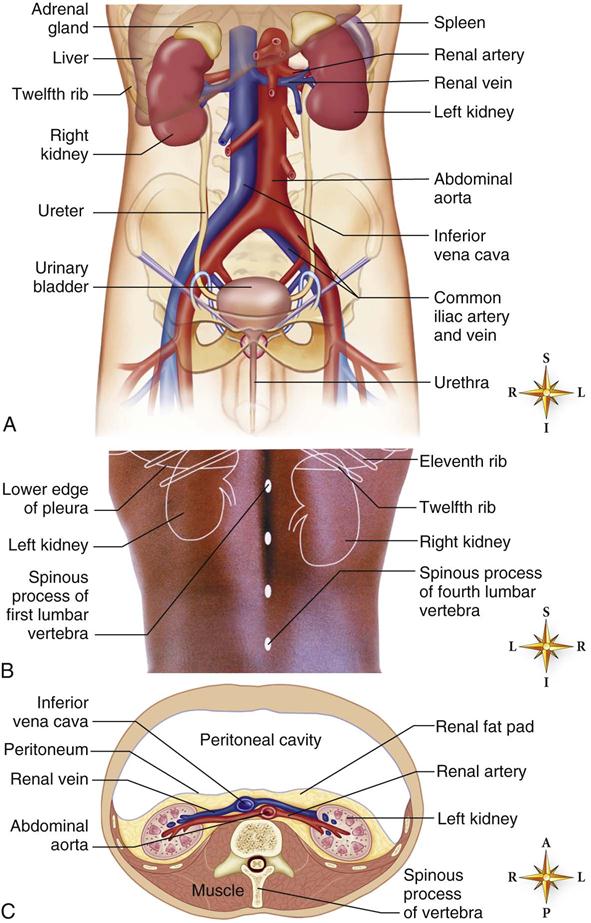
A, Anterior view of the urinary organs with the peritoneum and visceral organs removed. B, Surface markings of the kidneys, eleventh and twelfth ribs, spinous processes of L1 to L4, and lower edge of the pleura (posterior view). C, Horizontal (transverse) section of the abdomen showing the retroperitoneal position of the kidneys. (A, From Barbara Cousins. B, From Abrahams P, Marks S, Hutchings R: McMinn’s Color Atlas of Human Anatomy, ed 5, Philadelphia, 2003, Mosby, C: From Patton KT, Thibodeau GA: Anatomy & Physiology, ed 8, St. Louis, 2013, Mosby.)
Inside each kidney is the cortex, or outer layer, in which the majority of the glomeruli are located, and the medulla, or inner section of tissue, which consists primarily of the tubules and collecting ducts. Inside the medulla lie the renal pelvis and calyces, through which urine flows into the ureter (Fig. 18-2).
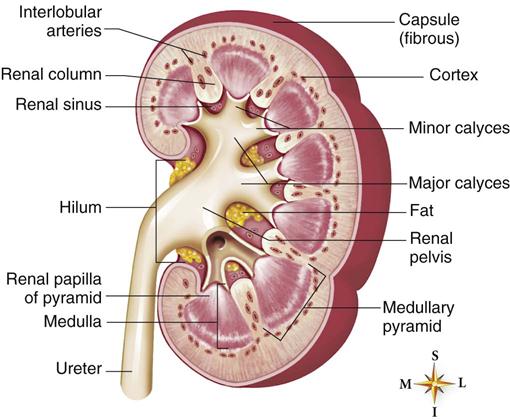
Coronal section of the right kidney in an artist’s rendering. (Adapted from Brundage DJ: Renal Disorders. Mosby’s Clinical Nursing Series, St. Louis, 1992, Mosby.)
Each kidney consists of over a million nephrons, the functional units of the kidney (Fig. 18-3). The renal corpuscle consists of Bowman’s capsule (glomerular capsule), which is the blind end of the proximal convoluted tubule. This capsule surrounds a network of capillaries, called the glomerulus or glomerular capillaries. These form the filtration unit for the blood.
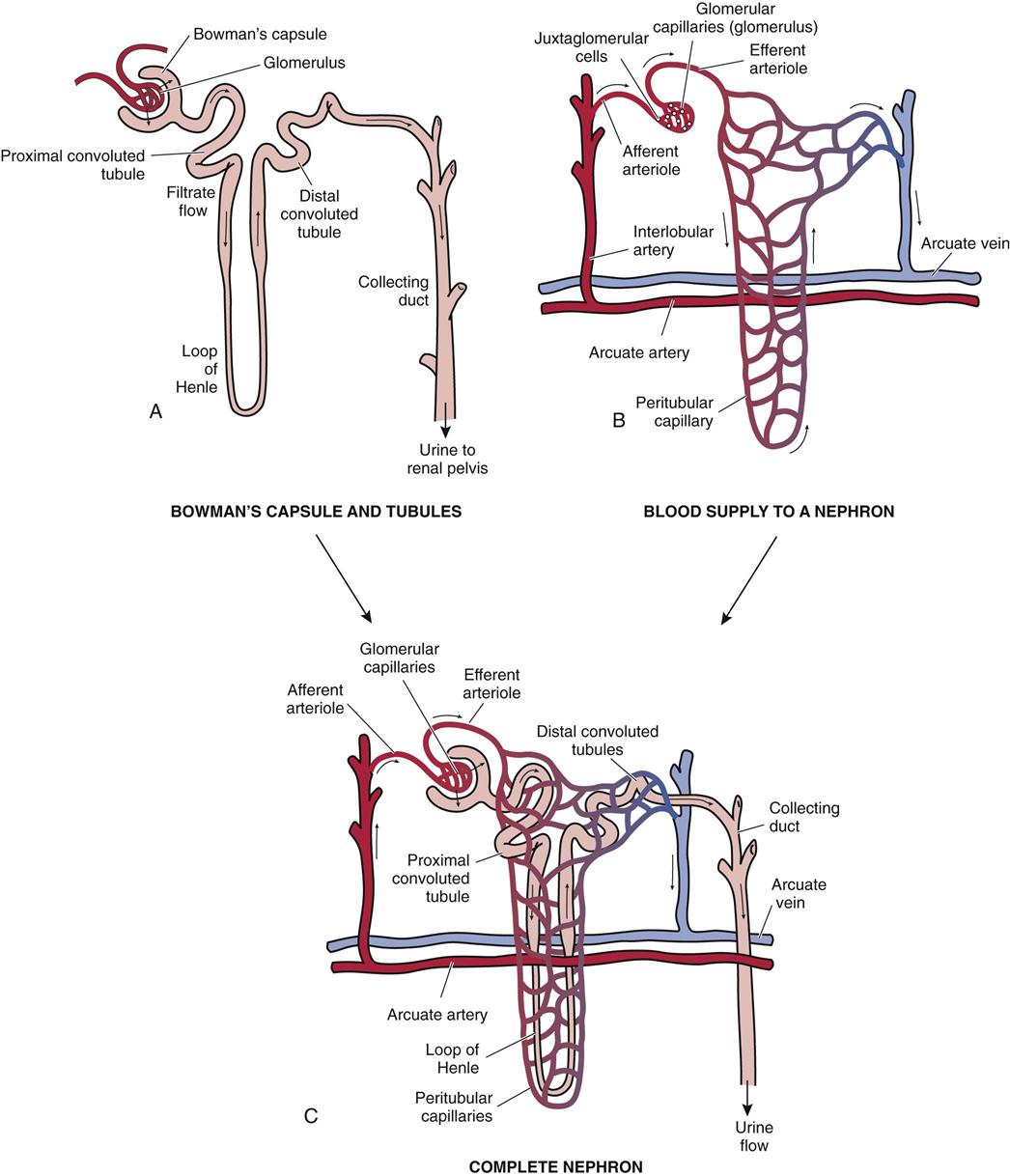
A, Glomerulus and tubules. B, Blood supply to the nephron. C, Complete nephron.
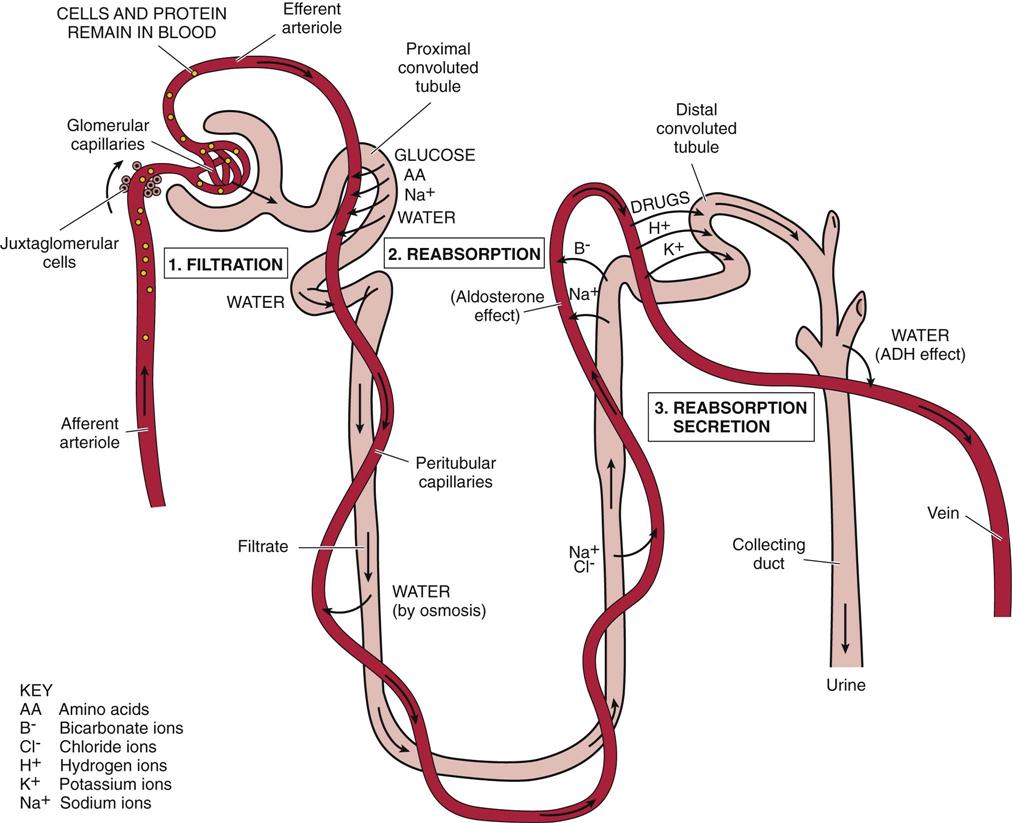
During filtration, a large volume of fluid, including wastes, nutrients, electrolytes, and other dissolved substances, passes from the blood into the tubule. Cells and protein remain in the blood (Table 18-1). When the filtration pressure increases, more filtrate forms, and more urine is produced. The filtrate flows into the tubules. The tubule consists of three parts, the proximal convoluted tubule, the loop of Henle, and the distal convoluted tubule. Here reabsorption of essential nutrients, water, and electrolytes takes place and secretion of certain wastes and electrolytes occurs. The collecting ducts transport the urine to the renal pelvis.
TABLE 18-1
Composition of Blood, Filtrate, and Urine
| Substance | Blood | Filtrate | Urine |
| Water (L) | 180 | 180 | 1.4 |
| Cells | Yes | No | No |
| Glucose (mg/L) | 1000 | 1000 | 0 |
| Protein (mg/L) | 40,000 | 0-trace | 0-trace |
| Urea (mg/L) | 260 | 260 | 18,000 |
| Na+ (mEq/L) | 142 | 142 | 128 |
| K+ (mEq/L) | 5 | 5 | 60 |
| HCO3− (mEq/L) | 28 | 28 | 14 |

Reabsorption is one process that takes place in the tubules. In the proximal convoluted tubule, most of the water is reabsorbed into the blood in the peritubular capillaries, along with glucose and other nutrients and some electrolytes. Reabsorption of nutrients and electrolytes involves the use of active transport (e.g., sodium ions), which requires carrier molecules and an energy source. Sodium absorption may be linked to the cotransport of other molecules (e.g., glucose or amino acids with Na+). Anions such as chloride may be reabsorbed by electrochemical gradient or by cotransport with Na+. If a substance such as glucose is present in excessive amounts in the filtrate, there are insufficient carrier molecules in the tubules for complete reabsorption into the blood in the peritubular capillaries. Therefore the excess glucose is present in the urine. This limit on reabsorption is called the transport or tubular maximum (e.g., approximately 310 mg/min for glucose). Thus, persistent glucosuria is an indication of hyperglycemia associated with diabetes mellitus.
Water is reabsorbed by osmosis. As the filtrate progresses through the loop of Henle and the distal convoluted tubule, electrolytes and water are adjusted to the body’s current needs.
Hormones control the reabsorption of fluid and electrolytes (see Chapters 2 and 16):
Concurrently the acid-base balance of the blood is maintained, with removal of excess acids and replacement of buffers such as bicarbonate (see Chapter 2).
Active secretion of some wastes and drugs from the blood into the filtrate also occurs in the distal tubule (Fig. 18-4).
The organization of the nephrons within a kidney is complex and must be maintained for effective renal function. The blood vessels and the collecting tubules and ducts for the filtrate must be functionally integrated to fulfill the purpose of the system. Scar tissue can interfere with blood or filtrate flow and thus can lead to secondary damage and progressive destruction of the kidney.
Renal Arteries and Veins
A large amount of blood enters and leaves the kidney at the hilum through the renal artery and vein. From 20% to 25% of the cardiac output enters the renal arteries from the aorta; thus the kidneys are processing a large volume of blood at any given time. Each renal artery passes through the renal pelvis, dividing several times during its passage (see Fig. 18-2). No anastomoses or junctions exist between the interlobar and arcuate arteries, meaning that no alternative blood supply is available to a lobe of the kidney that is deprived of its blood supply, perhaps by an embolus (e.g., a blood clot). Any obstruction to blood flow would therefore cause that particular lobe to undergo necrosis and infarction.
The interlobar arteries divide several times, eventually forming the afferent arterioles, which supply the glomerular capillaries (see Fig. 18-3). The arrangement of blood vessels in the kidney is unique because the blood from the glomerular capillaries then flows into another arteriole, the efferent arteriole, and then into a second capillary network, the peritubular capillaries or vasa recta. Therefore there are two arterioles and two sets of capillaries included in each nephron.
This blood supply also provides nourishment for the renal tissues. Note that the kidney tubules are last to receive nutrients.
To summarize the blood flow: renal artery → interlobar artery → arcuate artery → interlobular artery → afferent arteriole → glomerular capillaries → efferent arteriole → peritubular capillaries → interlobular vein → arcuate vein → interlobar vein → renal vein. The names of the blood vessels match the structures.
The purpose of the dual arterioles is to control the pressure in the glomerular capillaries and consequently the glomerular filtration pressure. This pressure determines the glomerular filtration rate (GFR). By constricting or dilating the arterioles, the amount of blood in the glomerular capillaries is adjusted, and filtration is normally maintained regardless of fluctuations in the systemic blood pressure. For instance, if the afferent arteriole is dilated and the efferent arteriole is constricted, hydrostatic pressure in the glomerular capillaries will increase, and GFR will increase (Fig. 18-5).
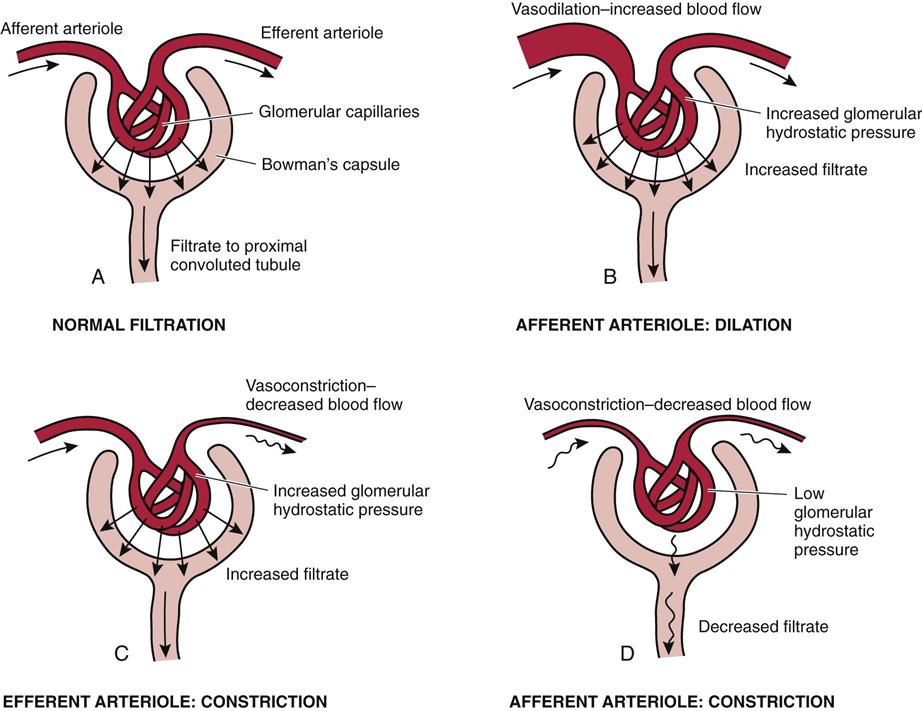
A, Normal filtration. B, Afferent arteriole: dilation. C, Efferent arteriole: constriction. D, Afferent arteriole: constriction.
The degree of constriction in the arterioles is controlled primarily by three factors, local autoregulation, the sympathetic nervous system, and the renin-angiotensin mechanism.
2. The sympathetic nervous system (SNS) increases vasoconstriction in both arterioles when stimulated.
3. Renin is secreted by the juxtaglomerular cells in the kidney when blood flow in the afferent arteriole is reduced for any reason (see Fig. 18-5). Through a series of enzyme reactions, renin acts on the plasma protein angiotensinogen to produce angiotensin I and as the blood passes through the lung, angiotensin converting enzyme (ACE) converts angiotensin I to angiotensin II, which is a powerful systemic vasoconstrictor.
If blood flow in the kidney is seriously impaired, as it is when blood pressure drops, both the SNS and the renin-angiotensin mechanism are activated to restore blood pressure and blood flow to vital areas.
Blood pressure is closely related to kidney function, and frequently it is elevated with renal disease. When the blood flow or blood pressure in the afferent arteriole decreases for any reason, the renin-angiotensin-aldosterone triad is stimulated. Angiotensin not only causes systemic vasoconstriction, it also stimulates the secretion of aldosterone. This hormone increases the reabsorption of sodium and water to increase blood volume, thus increasing blood pressure. Serum renin levels can determine whether this mechanism is a factor in hypertension (high blood pressure), in which case renin-blocking drugs (beta-adrenergic blocking drugs) can be prescribed (see Chapter 12).
When the filtrate has been processed in the tubules and collecting ducts, it is considered to be urine. Urine is transported through the collecting ducts to the renal calyces and pelvis and then into the ureters, where peristaltic movements assist its flow to the urinary bladder. The renal pelvis, calyces, ureters, and bladder are lined with transitional epithelium that is not permeable to water and can resist the irritation of constant contact with urine.
The bladder is composed of smooth muscle that falls in rugae, or folds, to form an expandable sac. It is located retroperitoneally in the pelvic cavity. The bladder has openings for the two ureters to bring urine in and an outlet for the urethra through which urine flows out of the body. The triangular section outlined by these three openings is called the trigone (see Fig. 18-1).
The female urethra is 3 to 4 cm long. It is relatively short and wide and opens onto the perineum anterior to the vagina and anus. The proximity of the urethra to these two sources promotes infection of the bladder in women.
The male urethra is about 20 cm long and passes through the penis. At the base of the male bladder is the prostate gland, which plays a role in semen production and frequently is hypertrophied in older men, obstructing urine flow (see Chapter 19 for reproductive disorders). During orgasm in the male, a sphincter closes off the flow of urine and semen is ejaculated through the urethra.
The mucosa lining the urinary tract is continuous through the urethra, bladder, and ureter to the pelvis of the kidney. Organisms can easily enter the system through the urethra, and this continuous mucosa facilitates the spread of infection through the urinary tract (an ascending infection).
Micturition (urination, voiding) occurs when a reflex is stimulated by increased pressure as the bladder distends. The reflex is transmitted by parasympathetic nerves extending to the sacral spinal cord. If the time is appropriate, under voluntary control, the external and internal sphincters of the bladder and the pelvic diaphragm relax while the bladder muscle contracts, emptying the bladder.
Incontinence and Retention
Incontinence, or the loss of voluntary control of the bladder, has many causes. Young children must learn voluntary control as the nervous system matures. Enuresis defines involuntary urination by a child after age 4 to 5, when bladder control can be expected. Most children have nocturnal enuresis only. The majority of cases appear to be related to factors such as a developmental delay, sleep pattern, or psychosocial aspects rather than to a physical defect. Stress incontinence occurs when increased intra-abdominal pressure forces urine through the sphincter. This can occur with coughing, lifting, or laughing, but occurs more frequently in women after the urogenital diaphragm has become weakened by multiple pregnancies or age. Overflow incontinence results from an incompetent bladder sphincter. In the elderly, a weakened detrusor muscle may prevent complete emptying of the bladder, leading to frequent emptying and incontinence. Spinal cord injuries or brain damage frequently cause a neurogenic bladder, which may be spastic or flaccid, due to interference with central nervous system (CNS) and autonomic nervous system control of the bladder emptying.
Retention is an inability to empty the bladder. It may be accompanied by overflow incontinence. Note that a spinal cord injury at the sacral level blocks the micturition reflex, resulting in retention of urine or failure to void. Retention also may occur after anesthesia, either general or spinal. Inability to control urine flow may be managed by wearing pads or briefs that contain the urine.
A catheter is a tube inserted in the urethra that drains urine from the bladder to a collecting bag outside the body. Catheters are common sources of infection in the urinary tract because they are irritating to the tissue and, when inserted, may be a means of introducing bacteria directly into the bladder if sterile technique is not used. Catheters prevent kidney damage due to backup of urine, collect urine, and prevent skin breakdown in the incontinent client.
Diagnostic Tests
Urinalysis
The constituents and characteristics of urine may vary with dietary intake, drugs, and the care with which a specimen is handled. Urine normally is clear and straw-colored and has a mild odor. Urine pH is in the range of 4.5 to 8.0. The following lists offer general guidelines to common abnormalities noted in freshly voided specimens. An “old” specimen will not provide accurate information. See the inside front cover of this book for normal values.
Appearance
Abnormal Constituents (Present in Significant Quantities)
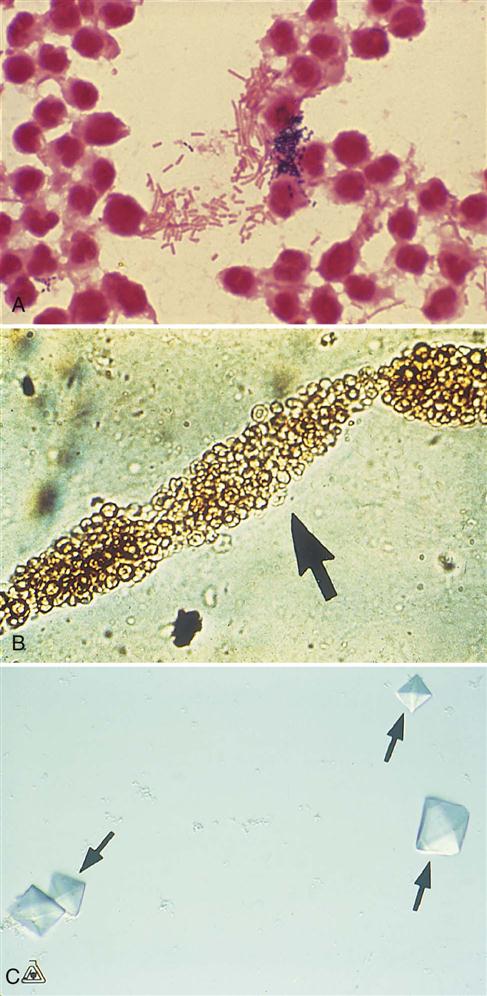
• Bacteria (bacteriuria) and pus (pyuria)—indicate infection in the urinary tract (Fig. 18-6A)
• Urinary casts (microscopic-sized molds of the tubules, consisting of one or more cells, bacteria, protein, and so on)—indicate inflammation of the kidney tubules (see Fig. 18-6B)
• Glucose and ketones (ketoacids) are found in the urine when diabetes mellitus is not well controlled (see Chapter 16)
Blood Tests
Like most other diseases, urinary tract disorders produce abnormalities that can be detected by various blood tests. Some of the more commonly used tests and implications are described here.
Other Tests
• Culture and sensitivity studies on urine specimens are used to identify the causative organism and select drug treatment when infection is suspected (see Chapter 6).
Diuretic Drugs
Diuretics, commonly referred to as “water pills,” are used to remove excess sodium ions and water from the body, therefore increasing the excretion of water through the kidneys and urinary output. In turn, this reduces fluid volume in the tissues (edema) and blood. They are prescribed for many disorders other than renal disease, including hypertension, edema, congestive heart failure, liver disease, and pulmonary edema (see Chapter 12).
There are several mechanisms by which urine volume can be increased. A few examples of diuretic drugs are listed in Table 18-2. The most commonly used drug group inhibits sodium chloride reabsorption in the tubules. Examples of this group include hydrochlorothiazide (Hydro Diuril), a mild diuretic, and furosemide (Lasix), which is more potent. Hydrochlorothiazide is useful because it has an additional antihypertensive action, the mechanism for which is unknown. The major side effect of these drugs is excessive loss of electrolytes, which may cause muscle weakness or cardiac arrhythmias. Because these drugs may cause marked loss of potassium, patients may require dietary supplements such as bananas or replacement by potassium chloride tablets. Another group of diuretics, the potassium-sparing type (e.g., spironolactone [Aldactone]), may be given in combination with thiazides to minimize the risk of hyperkalemia or hypokalemia (high or low serum potassium levels). Many combinations of diuretics with other drugs, such as hydrochlorothiazide/propranolol or hydrochlorothiazide/quinapril, are available to treat hypertension or heart failure.
TABLE 18-2
| Name of Drug | Action | Use |
| hydrochlorothiazide (Hydro DIURIL) | Inhibits reabsorption of Na+ and water in distal tubule (thiazide type) | Increase excretion of fluid in hypertension, CHF, edema |
| furosemide (Lasix) | Decreases reabsorption of Na+ and water in the proximal and distal tubules and the loop of Henle (a loop diuretic) | Reduce body fluids in hypertension, CHF, edema, renal disease, liver disease |
| spironolactone (Aldactone) | Aldosterone antagonist, blocks reabsorption of Na+ and K+ in distal tubule (potassium-sparing diuretic) | Decrease Na+ and water in body, but conserve K+ in CHF, hypertension, liver disease |
| acetazolamide (Diamox) | Carbonic anhydrase inhibitor blocks reabsorption of Na+ and secretion of H+ | Reduce fluids in CHF, glaucoma |
| mannitol (intravenous) | Increases osmotic pressure and water in the filtrate, reduces Na+ absorption (osmotic diuretic) | Cerebral edema, glaucoma |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree