Digestive System Disorders
Learning Objectives
After studying this chapter, the student is expected to:
1. Describe the various causes of vomiting and the vomiting process.
2. Differentiate diarrhea from constipation.
3. Differentiate cleft lip from cleft palate.
4. Describe the common oral infections and periodontal disease.
5. Explain the common causes of dysphagia.
6. Differentiate the types of hiatal hernias and explain their effects.
7. List the causes of acute gastritis and describe the common signs.
8. Compare the effects of acute gastritis, chronic gastritis, and gastroenteritis.
9. Describe the etiology, the signs, and possible complications of peptic ulcers.
10. Describe the pathophysiology, etiology, and early signs of gastric cancer.
11. Explain how dumping syndrome develops and list the signs associated with the syndrome.
12. Explain how pyloric stenosis interferes with normal function, and list the common manifestations.
13. Describe how gallstones develop and the signs of obstruction.
14. Differentiate the types of jaundice.
15. Compare the types of infectious hepatitis.
16. Describe the common manifestations of hepatitis.
17. Explain why the cause of toxic hepatitis should be identified quickly.
18. Differentiate the types of cirrhosis.
19. Describe the pathophysiology and manifestations of cirrhosis.
20. Describe the pathophysiology, signs, and possible complications of acute pancreatitis.
21. Explain how gluten toxicity may affect individuals with celiac disease.
22. Describe the signs of malabsorption.
23. Compare Crohn’s disease with ulcerative colitis.
24. Describe the symptoms and the various causes of irritable bowel syndrome.
26. Explain how diverticulosis and diverticulitis develop.
27. Describe the causes and possible characteristics of colorectal cancer.
28. Relate the location of colorectal cancer to the possible signs.
29. Describe the common causes of intestinal obstruction.
31. Explain the progressive effects of intestinal obstruction and the related signs.
32. Differentiate chemical peritonitis from bacterial peritonitis, including causes for each.
33. Describe the pathophysiology of peritonitis and possible complications.
Key Terms
abscesses
adhesions
autodigestion
bolus
calculi
cholestasis
chyme
colostomy
exocrine
fecalith
gastrectomy
gluconeogenesis
glycogen
hematemesis
hepatocytes
hepatotoxins
hyperbilirubinemia
icterus
ileostomy
impaction
mastication
melena
mesentery
multiparity
occult
pruritus
retroperitoneal
rugae
sinusoids
splenomegaly
steatorrhea
stricture
tenesmus
ulcerogenic
Review of the Digestive System
The general purpose of the digestive system is to efficiently process ingested food and fluids and the various secretions from glands. First they are broken down into their separate constituents; then the desired nutrients, water, and electrolytes are absorbed into the blood for use by the cells, and waste elements are eliminated from the body. Within this system, the liver can reassemble the component nutrients into new materials as they are needed by the body. For example, the proteins in milk are digested by enzymes in the digestive tract, producing the component amino acids, which are then absorbed into the blood. The individual amino acids are used by the liver cells to produce new proteins, such as albumin or prothrombin, or they may circulate unchanged in the blood to be taken up by individual cells as necessary.
Structures and Their Functions
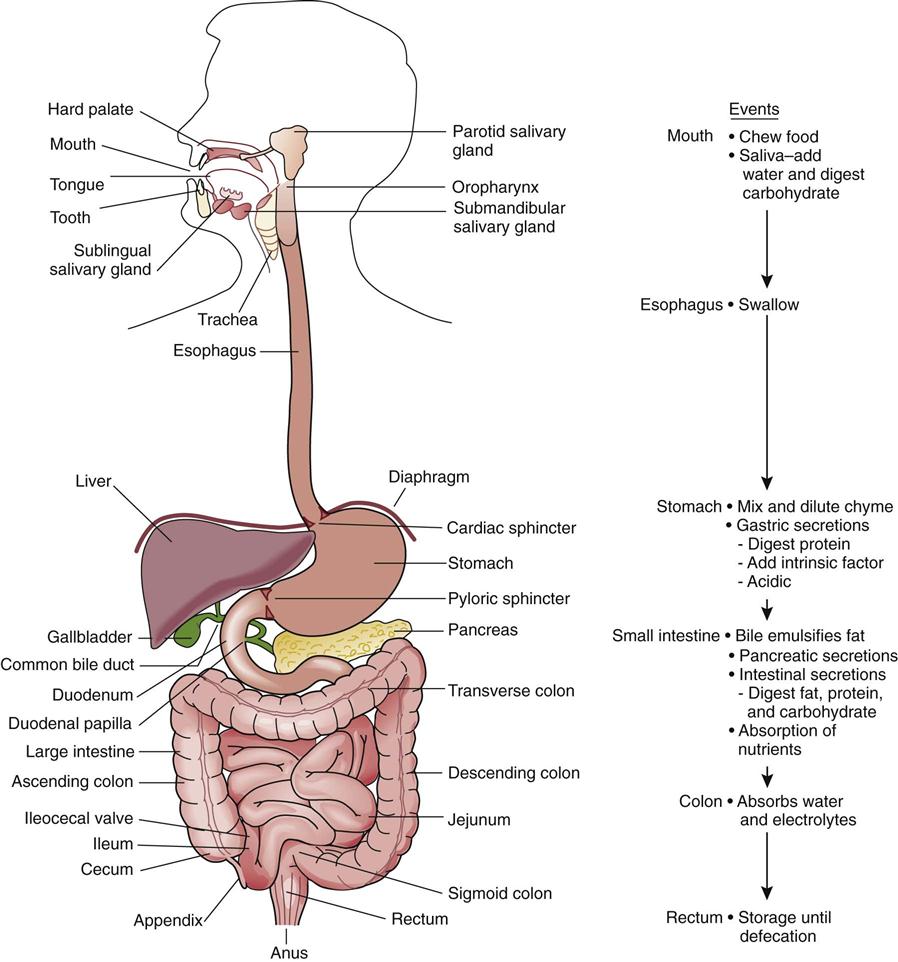
The digestive system, sometimes called the gastrointestinal tract, alimentary tract, or gut, consists of a long hollow tube which extends through the trunk of the body, and its accessory structures: the salivary glands, liver, gallbladder, and pancreas (Fig. 17-1). The digestive tract is divided into two sections, the upper tract, consisting of the mouth, esophagus, and stomach, and the lower tract, consisting of the intestines.
Although variations occur along the tube, the wall of the gut basically has five continuous layers:
3. Circular smooth muscle fibers.
4. Longitudinal smooth muscle fibers.
These two smooth muscle layers are responsible for transport or motility in the tract.
5. The outer layer of the wall comprises the visceral peritoneum, or serosa.
The peritoneum is a large serous membrane in the abdominal cavity (see Ready Reference 1). The parietal peritoneum covers the abdominal wall and the superior surface of the urinary bladder and uterus, and then continues, reflecting back to form the visceral peritoneum, which encases the organs, such as the stomach and intestine. This arrangement creates a double-walled membrane in the abdominal cavity, which is similar to the pleural and pericardial membranes. Pain receptors connected to spinal nerves are located in the parietal peritoneum.
The peritoneal cavity refers to the potential space between the parietal and visceral peritoneum. A small amount of serous fluid is present in the cavity to facilitate the necessary movement of structures such as the stomach. Numerous lymphatic channels drain excessive fluid from the cavity.
Because serous membranes are normally thin, somewhat permeable, and highly vascular, the peritoneal membranes are useful as an exchange site for blood during peritoneal dialysis in patients with kidney failure (see Chapter 18). However, such an extensive membrane may also facilitate the spread of infection or malignant tumor cells throughout the abdominal cavity or into the general circulation.
The mesentery is a double layer of peritoneum that supports the intestines and conveys blood vessels and nerves to supply the wall of the intestine. The mesentery attaches the jejunum and ileum to the posterior (dorsal) abdominal wall. This arrangement provides a balance between the need for support of the intestines and the need for considerable flexibility to accommodate peristalsis and varying amounts of content.
The greater omentum is a layer of fatty peritoneum that hangs from the stomach like an apron over the anterior surface of the transverse colon and the small intestine. The lesser omentum is part of the peritoneum that suspends the stomach and duodenum from the liver. When inflammation develops in the intestinal wall, the greater omentum, with its many lymph nodes, tends to adhere to the site, walling off the inflammation and temporarily localizing the source of the problem. Inflammation of the omentum and peritoneum may lead to scar tissue and the formation of adhesions between structures in the abdominal cavity, such as loops of intestine, restricting motility and perhaps leading to obstruction.
The kidneys and pancreas are located posterior to the stomach against the abdominal wall and behind the parietal peritoneum. They are covered with peritoneum only on the anterior surface and are therefore referred to as retroperitoneal organs.
Upper Gastrointestinal Tract
Oral Cavity
Food and fluid are taken into the body through the mouth, where the initial phase of mechanical breakdown and digestion takes place, and are then stored in the stomach, where processing continues. The mouth is separated from the nasal cavity by the hard and soft palates. A large variety of microorganisms make up the resident flora of the mouth. In the mouth, or oral cavity (Fig. 17-2), mastication takes place as the teeth break down solid food and mix it with saliva. Salivary secretions from the parotid, sublingual, and submandibular glands enter the mouth through the salivary ducts, moisturizing and lubricating (with mucins) the food particles and facilitating the passage of solid material down the esophagus to the stomach. Saliva also contains the enzyme amylase, which begins the digestion of carbohydrate in the mouth (Table 17-1). Perhaps you have noted how chewing crackers can bring a sweet taste in the mouth as the starch is broken down. The tongue and cheeks facilitate the movement and mixing of the food in the mouth. Chewing is usually considered a voluntary action, but reflex chewing can occur if voluntary control is lost.
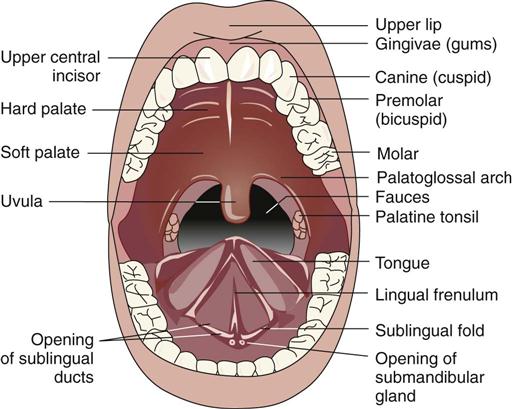
TABLE 17-1
Major Digestive Enzymes and Their Actions
| Enzyme | Source | Action |
| Salivary amylase | Parotid gland | Splits starch and glycogen into disaccharides |
| Pepsin | Gastric chief cells | Initiates splitting of proteins |
| Pancreatic amylase | Pancreas | Splits starch and glycogen into disaccharides |
| Pancreatic lipase | Pancreas | Splits triglycerides into fatty acids and monoglycerides |
| Trypsin, chymotrypsin, carboxypeptidase | Pancreas | Splits proteins into peptides |
| Pancreatic nucleases | Pancreas | Splits nucleic acids into nucleotides |
| Intestinal peptidase | Intestinal mucosa | Converts peptides into amino acids |
| Intestinal lipase | Intestinal mucosa | Converts fats into fatty acids and glycerol |
| Intestinal sucrase, maltase, lactase | Intestinal mucosa | Converts disaccharides into monosaccharides |
Esophagus
When food is ready to be swallowed, the tongue pushes the bolus or ball of food back to the pharyngeal wall, where receptors of the trigeminal and glossopharyngeal nerves relay the information to the swallowing center in the medulla. Because the reflex is activated at this point, swallowing (or deglutition) becomes an involuntary activity. The swallowing center coordinates the actions required to move food or fluid into the stomach, without aspiration into the lungs, by means of cranial nerves V, IX, X, and XII in the following steps:
• The soft palate is pulled upward.
• The vocal cords are approximated.
• The epiglottis covers the larynx.
• The bolus is seized by the constricted pharynx.
The pressure in this sphincter normally prevents reflux of gastric contents back up the esophagus. The esophagus is composed of skeletal muscle at the superior end that is gradually replaced by smooth muscle fibers. The entire tube is lined with mucous membrane and is closed, except when swallowing is in progress.
Stomach
The stomach is an expansible muscular sac that acts as a reservoir for food and fluid. The stomach can hold 1.0 to 1.5 liters of food and fluid. When empty, the stomach wall falls into folds, or rugae. The outer surface is covered by visceral peritoneum. The wall of the stomach consists of three smooth muscle layers—longitudinal and circular layers and an additional oblique muscle layer—plus the mucosa and submucosa. The epithelial cells of the mucosa are tightly packed together to prevent penetration of acid or pepsin into the wall. Numerous glands are located in the mucosa, and there is a layer of thick protective mucus covering the inner surface.
Constant mixing and churning of food occurs as secretions are added from the gastric glands. These secretions dilute the gastric contents, or chyme, and initiate the digestion of protein. The gastric glands located in the fundus of the stomach contain parietal cells that secrete hydrochloric acid and chief cells that secrete pepsinogen, which is converted to the active form, pepsin, by the action of hydrochloric acid. Intrinsic factor, required for the absorption of vitamin B12 in the ileum, is also produced by the parietal cells (see Chapter 10 for discussion of pernicious anemia). The gastric secretions act as a defensive mechanism because of the highly acidic pH (around 2), which destroys many microorganisms that enter the stomach from the resident flora in the mouth or from food or utensils. Protective mucus is secreted by glands in the cardiac and pyloric areas. Also, enteroendocrine cells in the glands secrete a variety of chemicals, the most important of which is the hormone gastrin, which is released when food enters the stomach and then stimulates the parietal and chief cells.
Depending to some extent on the type of food ingested, gastric emptying proceeds slowly, with small amounts of chyme (1 to 3 mL) passing intermittently through the pyloric sphincter into the duodenum. Secretions from the liver and the exocrine pancreas are added to the chyme in the duodenum through the ampulla of Vater and duodenal papilla (see Fig. 17-18).
Liver
The liver is located in the upper right quadrant (URQ) of the abdomen under the diaphragm and serves as the “metabolic factory” of the body. It is a large organ covered by a fibrous capsule, distention of which causes a dull, aching pain. The liver cells can regenerate, but if the organizational structure of the lobule, with its unique arrangement of blood vessels and bile ducts, is altered by necrosis and scar tissue, the regenerated areas may not be functional.
The hepatocytes, or liver cells, are arranged in lobules, and each lobule has plates of cells radiating from central veins, which eventually drain blood back into the general circulation through the hepatic veins and inferior vena cava (see Fig. 17-20). Channels or sinusoids filled with blood from two sources pass between the plates of hepatocytes. Entering the sinusoid is blood from branches of the hepatic artery, carrying oxygen to the liver cells; venous blood from the portal vein, which transports nutrients absorbed from the stomach and intestines (hepatic portal circulation); as well as from the pancreas and spleen. The arterial and venous blood mix and flow slowly through the sinusoids, permitting the hepatocytes to do their jobs. The sinusoids are lined with endothelial cells and Kupffer cells, which remove and phagocytose any foreign material and bacteria from the digestive tract before the blood enters the general circulation.
As blood flows through the sinusoids, many substances are exchanged to facilitate liver functions. Absorbed nutrients are taken up by the hepatocytes to be stored (e.g., the minerals iron and copper, or vitamins A, B6, B12, D, and K, and folic acid). Many blood components such as iron or amino acids are monitored, and those that have been depleted as the blood circulates through the body are replaced. Blood glucose levels are maintained; glucose is essential for brain function.
In conjunction with the hormone insulin, the liver responds to high levels of blood glucose by glycogenesis, converting glucose to glycogen, which is stored in the liver. Alternatively, the hepatocytes break down liver glycogen to glucose (glycogenolysis) when blood glucose levels drop and glucagon secretion increases. Gluconeogenesis, the conversion of protein and fat into glucose, may take place when blood glucose levels drop, under the influence of hormones such as cortisol or epinephrine.
Conversion of one amino acid into another takes place as needed to maintain the amino acid pool in the blood and meet the body’s needs. Synthesis and control of blood levels of other materials, such as plasma proteins, clotting factors, or lipoproteins, is accomplished. Synthesis of cholesterol occurs in the liver for use in the production of steroid hormones, such as cortisol or the sex hormones, and bile salts.
Hormones, such as aldosterone and estrogen, are inactivated and prepared for excretion. Ammonia, a nitrogen waste resulting from protein metabolism in the intestine or liver, is removed from the blood and converted to urea, enabling it to be excreted by the kidneys. Drugs and alcohol are detoxified before excretion. The detoxification process makes such substances less harmful and increases the solubility of many substances, facilitating their excretion.
Damaged or old erythrocytes are removed from the blood to facilitate the recycling of iron and protein from hemoglobin (see Figs. 10-7 and 17-21). The liver serves as a blood reservoir because it is capable of releasing a large quantity of blood into the general circulation when blood volume is depleted.
The hepatocytes of the liver constantly produce bile, a mixture of water, bile salts, bile pigment (conjugated bilirubin), cholesterol, and electrolytes, including bicarbonate ions. Bile is vital for digestion and serves as a vehicle for the removal of bilirubin and excess cholesterol from the body. The bile salts, formed from cholesterol, are essential for the emulsification of fats and fat-soluble vitamins (vitamins A, D, E, and K) before they can be absorbed from the intestine. The majority of the bile salts are reabsorbed from the distal ileum and recycled to the liver through the enterohepatic circulation. Bicarbonate ions in bile assist in neutralizing gastric acid, increasing the pH of the small intestine so that intestinal and pancreatic enzymes can function.
Bile is an exocrine secretion, flowing through small canaliculi in the liver and draining into larger ducts until it reaches the right or left hepatic duct and then the common bile duct. A sphincter in this duct usually directs the flow of bile into the gallbladder for storage but may allow it to flow onward into the duodenum. After surgical removal of the gallbladder, the storage facility is lost, but bile is constantly secreted by the liver and small amounts continuously enter the duodenum.
Pancreas
The pancreas lies posterior to the stomach, with its larger end or “head” adjacent to the duodenum. The cells of the exocrine pancreas are arranged in lobules throughout the organ; they secrete digestive enzymes, electrolytes, and water into tiny ducts, which eventually drain into the main pancreatic duct that traverses the length of the pancreas. The pancreatic duct, carrying secretions from the exocrine pancreas, joins the common bile duct and then enters the duodenum.
The major proteolytic enzymes in pancreatic secretions are trypsin and chymotrypsin, carboxypeptidase, and ribonuclease (see Table 17-1). Also, pancreatic amylase aids in the digestion of carbohydrates and lipase helps to digest fats. The enzymes are secreted in inactive form and are activated after they enter the duodenum. A trypsin inhibitor is produced by the pancreatic cells to reduce the risk of enzyme activation within the pancreas. Pancreatic secretions also contain bicarbonate ion, which assists in the neutralization of hydrochloric acid in the duodenum.
Lower Gastrointestinal Tract
Small Intestine
The small intestine has three sections, the duodenum, the jejunum, and the ileum, moving in a proximal to distal direction. The contents move slowly along the tube, influenced by both mixing and propulsive movements of the wall. Digestion continues in the duodenum while many enzymes are added to the chyme and an alkaline pH is attained. The ileum is the major site of absorption of nutrients.
The significant feature of the small intestine is the presence of plicae circulares, transverse folds of the mucosa covered with villi and microvilli (see Fig. 17-32A). These numerous tiny projections greatly increase the absorptive surface area of the small intestine. Each villus is supplied with a capillary network, nerves, and a lacteal, which is a terminal lymphatic vessel that is essential for the absorption of lipids. At the base of the villi are the intestinal crypts, deep pockets from which new epithelial cells (simple columnar absorptive cells) arise. Cells in the crypts produce fluid with a pH of around 7; as well as enzymes such as enterokinase, which activate pancreatic proenzymes; and hormones, such as cholecystokinin. Other enzymes produced by the cells of the intestinal mucosa include peptidases, nucleosidases, lipase, sucrase, maltase, and lactase. Many goblet cells in the mucosa secrete large quantities of mucus into the intestine to protect the intestinal wall and buffer the acid chyme.
Large Intestine
The ileocecal valve marks the entry point from the ileum into the large intestine or colon. Hanging down at this point is a pouch, the cecum, from which the blind-ending appendix (vermiform appendix) extends. Moving superiorly from the cecum is the ascending colon, which becomes the transverse colon and then passes down the left side as the descending colon. This structure terminates as the sigmoid colon, rectum, and anal canal. The anus is the opening to the exterior.
Absorption of large amounts of water and electrolytes takes place in the colon. This “recycling” process is of critical importance in maintaining the fluid and acid-base balances in the body, because large volumes of fluids and ions, such as bicarbonate and sodium, are recovered from the added secretions and ingested fluids. General digestion and absorption of nutrients ceases in the colon. Resident bacteria assist in further breakdown of certain food materials (one cause of intestinal gas) and convert bilirubin to urobilinogen, which gives the feces the typical brown color. In the ileum, large masses of lymphoid tissue, called Peyer’s patches, limit the spread of these bacteria into the small intestine. Some of these bacteria are beneficial to the human host, synthesizing vitamin K, for example, which is required for the production of clotting factors, such as prothrombin and fibrinogen, in the liver.
Colonic movements are slow to allow absorption of fluid and formation of the solid feces. The transverse and descending colon are marked by mass movements, strong peristaltic contractions that occur several times daily. Large pouches, or haustra, in the colon wall allow for expansion as more solid material collects.
Feces consist primarily of fiber and other indigestible material, sloughed mucosal cells, and bacteria. Increased bulk or fiber in the intestine increases intestinal motility and the rate of passage, leading to a larger fecal mass and thus, more frequent defecation, or bowel movements.
The rectum stores the solid feces until sufficient distention of the rectal wall stimulates the defecation reflex as follows:
Neural and Hormonal Controls
Stimulation of the parasympathetic nervous system (PNS), primarily through the vagus nerve (cranial nerve X), results in increased motility, or peristalsis, and increased secretions in the digestive system (Table 17-2; see also Chapter 14). During the initial cephalic phase before eating, pleasant smells, thoughts, or the sight of food can effect PNS stimulation. Conversely, emotions such as fear or anger stimulate the sympathetic nervous system (SNS), which inhibits gastrointestinal activity. Sympathetic nervous system activity also causes vasoconstriction, leading to reduced secretions and regeneration of epithelial cells.
TABLE 17-2
Major Controls in the Digestive Tract and Their Effects
| Hormone | Source | Stimulus | Effects |
| Gastrin | Gastric cells | Food in the stomach Protein, caffeine, or high pH of chyme | Increases gastric secretions and motility and promotes gastric emptying |
| Cholecystokinin | Intestinal mucosal cells | Protein and fat in the duodenum | Inhibits gastric secretions and motility; stimulates pancreatic enzyme secretion; stimulates gallbladder contractions and release of bile |
| Secretin | Intestinal mucosal cells | Acidic chyme in the duodenum | Stimulates bile and pancreatic secretions with high bicarbonate content |
| Neural Controls | Source | Stimulus | Effects |
| Parasympathetic nervous system | Vagus nerve | Taste food | Increases secretions and peristalsis |
| Sympathetic nervous system | SNS | Stress | Decreases secretions and peristalsis Stimulates vasoconstriction in the mucosa |
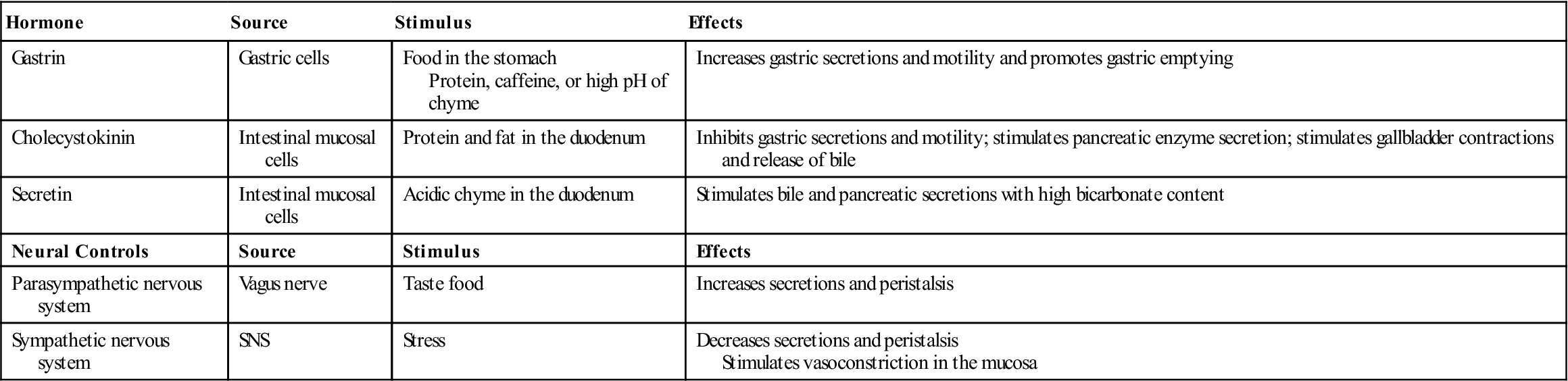
The PNS, through the facial (cranial nerve VII) and glossopharyngeal (cranial nerve IX) nerves, maintains a continuous flow of saliva in the mouth, which is essential to keep the tissues moist, effect a continuous cleansing action, and facilitate speech. A dry mouth for any reason leads to a sensation of thirst, a protection against dehydration. The sight, thought, or presence of food in the mouth stimulates increased salivary secretions, and these secretions usually continue for a time after swallowing, which is helpful in cleansing the mouth and teeth.
When food reaches the stomach, distention or stretching of the stomach and the increased pH caused by food intake activate the PNS, increasing peristalsis and gastric secretions. Peripheral nervous system stimulation also increases bile and pancreatic secretions. As digestion in the stomach progresses, peristaltic movements force small amounts of chyme, 2 to 3 mL at a time, into the duodenum. Depending on the amount and type of food involved, the stomach empties within 2 to 6 hours after a meal. Fluids pass through rapidly, whereas fats progress slowly. The presence of food in the intestine stimulates intestinal activity but inhibits gastric activity, through the enterogastric reflex, to prevent overloading of the duodenum and to allow sufficient time for intestinal digestion and absorption. Food passes through the small intestine at a fairly constant rate. After eating, a reflex increase in peristalsis around the ileocecal valve occurs, which moves the ileal contents into the cecum and colon. These anticipatory actions make the digestive tract into an efficient production line. Peristaltic movements in the colon are usually slow. The gastrocolic reflex stimulates a mass movement of the contents from the colon into the rectum when food enters the stomach.
Hormones play a major role in the process of digestion and absorption (see Table 17-2). Gastrin is secreted by mucosal cells in the pyloric antrum of the stomach in response to distention of the stomach or the presence of substances such as partially digested protein, alcohol, or caffeine in the stomach. Gastrin enters the blood and circulates, then returns to stimulate the gastric cells to increase secretions, increase gastric motility, and relax the pyloric and ileocecal sphincters, thus promoting stomach emptying.
In the presence of the chemical histamine that is released from local mast cells, stimulation of the parietal cells by the PNS or gastrin leads to increased secretion of hydrochloric acid. The histamine receptors on parietal cells are histamine2 (H2) receptors, not the histamine1 (H1) receptors on cells involved in allergic responses.
When chyme enters the duodenum, mucosal cells release hormones. Secretin and cholecystokinin (CCK) are two important ones. Secretin decreases gastric secretions and increases the bicarbonate ion content of pancreatic secretions and bile when the chyme is highly acidic. Cholecystokinin inhibits gastric emptying, stimulates pancreatic secretions with increased digestive enzymes, and stimulates contraction of the gallbladder to increase bile flow into the duodenum. Variations in the digestive secretions and the rate of flow of chyme through the tract depend on the amount and type of food entering the digestive tract. For example, gastric emptying is delayed when the duodenum is full or when a meal high in fat content is ingested.
Digestion and Absorption
Nutrients are broken down chemically into simple molecules that are absorbed along with electrolytes and water into the blood and transported to the liver through the hepatic portal system.
Complex carbohydrates, such as starches, are digested first in the mouth and then in the intestine. They are broken down by enzymes into simple sugars (monosaccharides) that are absorbed in the intestine, primarily in the jejunum and ileum. Glucose and galactose are absorbed by a co-transport mechanism with sodium that is already bound to a transport protein. Fructose is absorbed by facilitated diffusion. The process of active transport for sodium requires cellular energy (stored by adenosine triphosphate [ATP]), and therefore healthy cells with a good blood supply. On occasion, when a highly concentrated solution of glucose enters an empty stomach, glucose may diffuse quickly from the stomach into the blood. This rapid action can be effective in reversing hypoglycemia in a person with diabetes mellitus.
Proteins are first split into peptides, or short chains of amino acids, in the stomach and intestine and then further broken down by peptidases into amino acids, many of which are absorbed by a sodium co-transport system in the small intestine.
Lipids, or fats, primarily triglycerides, must first be emulsified (dispersed into tiny droplets) by bile (the bile salt component) in the small intestine; enzymes then act on the fats, forming monoglycerides and free fatty acids. These lipid-soluble molecules can diffuse across the cell membrane. Many recombine to form triglycerides again. Then, bound to protein, the lipids form chylomicrons, most of which diffuse into the lacteals or lymph capillaries in the microvilli. The lacteals join the lymphatic circulation, which empties into the general circulation. Eventually the lipids reach the liver or adipose cells. Short-chain fatty acids may diffuse directly into the blood. Fat-soluble vitamins (e.g., vitamins A, D, E, and K) or other lipid-soluble materials do not require digestion but are absorbed with the fats. If for any reason lipids are not absorbed, large molecules, such as fat-soluble vitamins, cannot be absorbed. For example, this problem may occur when individuals consume mineral oil as a laxative on a regular basis. Mineral oil remains in the intestine, and the fat-soluble vitamins are excreted with the oil.
Very small lipid-soluble molecules, such as alcohol, may be absorbed from the empty stomach into the blood by simple diffusion through the cell membranes. This promotes a high blood alcohol level within a short time after ingestion. The presence of food in the stomach delays such absorption.
Water-soluble vitamins (e.g., vitamins B and C) and minerals (e.g., iron, copper, and zinc) diffuse into the blood. Vitamin B12 must be bound to intrinsic factor before absorption. Electrolytes (Na+, K+, Cl−, HCO3−, and so on) may be absorbed by active transport or diffusion into the blood. Water is absorbed by osmosis. About 7000 mL of water is secreted into the digestive tract each day, and approximately 2300 mL is ingested in food and fluids. Of this amount, only 50 to 200 mL leaves the body in the feces. It is obvious that severe vomiting or diarrhea can quickly interrupt the recycling mechanism and affect fluid and electrolyte balance in the body.
Drugs are primarily absorbed in the intestine, although some small acidic molecules, such as aspirin, may be absorbed in the stomach. Other small molecules may be absorbed through the oral mucosa. Some drugs are broken down by digestive enzymes. The presence of certain foods or drugs, such as antacids, can interfere with absorption of other drugs. Large amounts of food in the stomach and intestine can also delay absorption of drugs.
Common Manifestations of Digestive System Disorders
Anorexia, Nausea, Vomiting, and Bulimia
The manifestations of anorexia, nausea and vomiting, may be signs of digestive system disorders or other conditions elsewhere in the body. For example, systemic infection, uremia (kidney failure), emotional responses such as fear, motion sickness, pressure in the brain, over-indulgence in food, drugs, or pain may initiate these signs. However, nausea and vomiting are common indicators of gastrointestinal disorders, and the characteristics of the vomitus and the vomiting pattern can be helpful in diagnosis. Vomiting is also considered a body defense because it removes noxious substances from the body. In addition, anorexia and vomiting can contribute to serious complications, such as dehydration, acidosis, and malnutrition.
Anorexia (loss of appetite) often precedes nausea and vomiting. Nausea is a generally unpleasant subjective feeling, which may be stimulated by distention, irritation, or inflammation in the digestive tract. Often, increased salivation, pallor, sweating, and tachycardia may occur with nausea and vomiting.
Vomiting, or emesis, is the forceful expulsion of chyme from the stomach and sometimes from the intestine. The vomiting center in the medulla coordinates the activities involved in vomiting (Fig. 17-3). The vomiting center is activated by many conditions, among which are:
• Distention or irritation in the digestive tract
• Stimuli from various parts of the brain in response to unpleasant sights or smells, or ischemia
• The vestibular apparatus of the inner ear (motion sickness)
• Increased intracranial pressure (see Chapter 14), causing sudden projectile vomiting without previous nausea or food intake
• Stimulation of the chemoreceptor trigger zone in the medulla by drugs, toxins, and chemicals
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree