http://evolve.elsevier.com/McCuistion/pharmacology/
Upper respiratory infections (URIs) include the common cold, acute rhinitis, sinusitis, and acute pharyngitis. The common cold is the most prevalent type of URI. Adults have an average of 2 to 4 colds per year, and children have an average of 4 to 12 colds per year. Incidence is seasonally variable: approximately 50% of the population experiences a winter cold and 25% experiences a summer cold. A cold is not considered a life-threatening illness, but it does cause physical and mental discomfort and lost time at work and school. The common cold is an expensive illness in the United States—more than $60 billion is spent each year on over-the-counter (OTC) cold and cough preparations in addition to missed time at work and school.
Common Cold, Acute Rhinitis, and Allergic Rhinitis
The common cold is caused by the rhinovirus and affects primarily the nasopharyngeal tract. Acute rhinitis, acute inflammation of the mucous membranes of the nose, usually accompanies the common cold. Acute rhinitis is not the same as allergic rhinitis, often called hay fever, which is caused by pollen or a foreign substance such as animal dander. Nasal secretions increase in both acute and allergic rhinitis.
A cold is most contagious 1 to 4 days before the onset of symptoms (the incubation period) and during the first 3 days of the cold. Transmission occurs more frequently from touching contaminated surfaces and then touching the nose or mouth than it does from contact with viral droplets released by sneezing.
The groups of drugs used to manage cold symptoms include antihistamines (H1 blockers), decongestants (sympathomimetic amines), antitussives, and expectorants. These drugs can be used singly or in combination preparations.
Symptoms of the common cold include rhinorrhea (watery nasal discharge), nasal congestion, cough, and increased mucosal secretions. If a bacterial infection secondary to the cold occurs, infectious rhinitis may result, and nasal discharge becomes tenacious, mucoid, and yellow or yellow green. The nasal secretions are discolored by white blood cells and cellular debris that are by-products of the fight against the bacterial infection. Antibiotics used to treat bacterial respiratory infections are discussed in Chapter 26.
Antihistamines
Antihistamines, H1 blockers or H1 antagonists, compete with histamine for receptor sites and prevent a histamine response. The two types of histamine receptors, H1 and H2, cause different responses. When the H1 receptor is stimulated, the extravascular smooth muscles—including those lining the nasal cavity—are constricted. With stimulation of the H2 receptor, an increase in gastric secretions occurs, which is a cause of peptic ulcer (see Chapter 43). These two types of histamine receptors should not be confused. Antihistamines decrease nasopharyngeal secretions by blocking the H1 receptor.
Although antihistamines are commonly used as cold remedies, these agents can also treat allergic rhinitis. However, the antihistamines are not useful in an emergency situation such as anaphylaxis. Most antihistamines are rapidly absorbed in 15 minutes, but they are not potent enough to combat anaphylaxis.
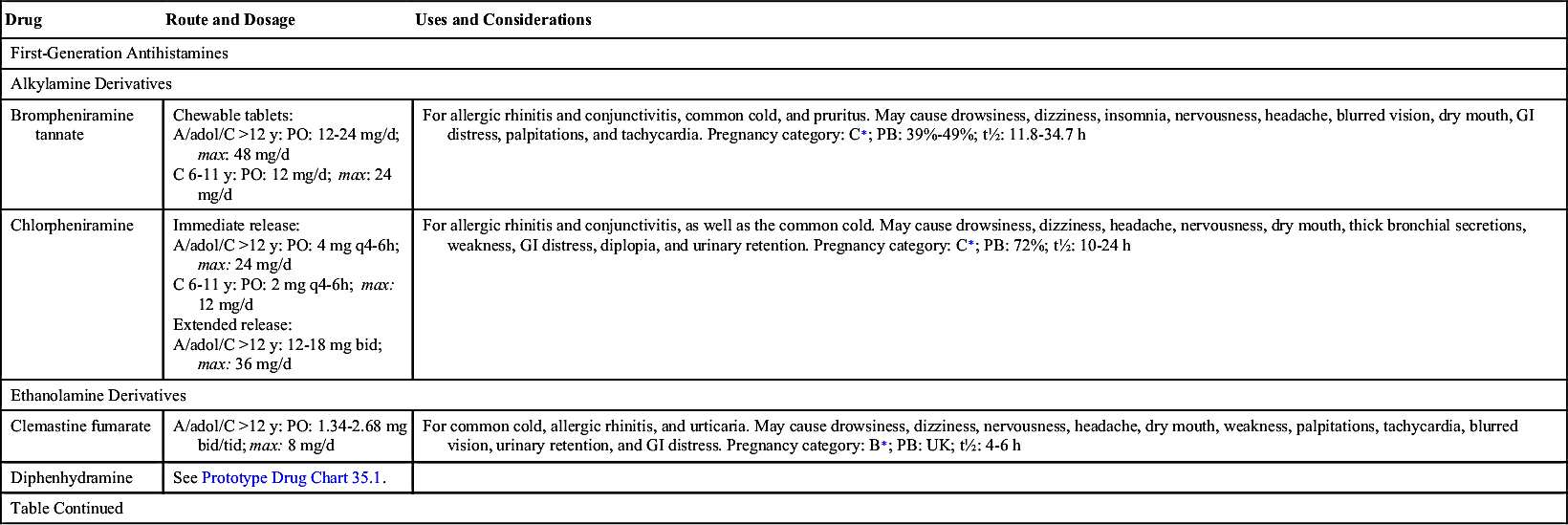
First-Generation Antihistamines
The antihistamine group can be divided into first and second generations. Most first-generation antihistamines cause drowsiness, dry mouth, and other anticholinergic symptoms, whereas second-generation antihistamines have fewer anticholinergic effects and a lower incidence of drowsiness. Many OTC cold remedies contain a first-generation antihistamine, which can cause drowsiness; therefore patients should be alerted not to drive or operate dangerous machinery when taking such medications. The anticholinergic properties of most antihistamines cause dryness of the mouth and decreased secretions, making them useful in treating rhinitis caused by the common cold. Antihistamines also decrease the nasal itching and tickling that cause sneezing.
The first-generation antihistamine diphenhydramine has been available for years and is frequently combined with other ingredients in cold remedy preparations. Its primary use is to treat rhinitis. Prototype Drug Chart 35.1 lists the pharmacologic behavior of diphenhydramine.
Pharmacokinetics
Diphenhydramine can be administered orally, intramuscularly (IM), or intravenously (IV). It is well absorbed from the gastrointestinal (GI) tract, but systemic absorption from topical use is minimal. It is highly protein bound (98%) and has an average half-life of 2 to 8 hours. Diphenhydramine is metabolized by the liver and is excreted as metabolites in the urine.
Pharmacodynamics
Diphenhydramine blocks the effects of histamine by competing for and occupying H1 receptor sites. It has anticholinergic effects and should not be used by patients with narrow-angle glaucoma. Drowsiness is a major side effect of the drug; in fact, it is sometimes used in sleep-aid products. Diphenhydramine is also used as an antitussive to alleviate cough. Its onset of action can occur in as few as 15 minutes when taken orally and IM. Intravenous administration results in an immediate onset of action. The duration of action is 4 to 7 hours.
Diphenhydramine can cause central nervous system (CNS) depression if taken with alcohol, narcotics, hypnotics, or barbiturates.
Side Effects of Most First-Generation Antihistamines
The most common side effects of first-generation antihistamines are drowsiness, dizziness, fatigue, and disturbed coordination. Skin rashes and anticholinergic symptoms such as dry mouth, urine retention, blurred vision, and wheezing may also occur.
Second-Generation Antihistamines
The second-generation antihistamines are frequently called nonsedating antihistamines because they have little to no sedative effect. In addition, these antihistamines cause fewer anticholinergic symptoms. Although a moderate amount of alcohol and other CNS depressants may be taken with second-generation antihistamines, many clinicians advise against such use.
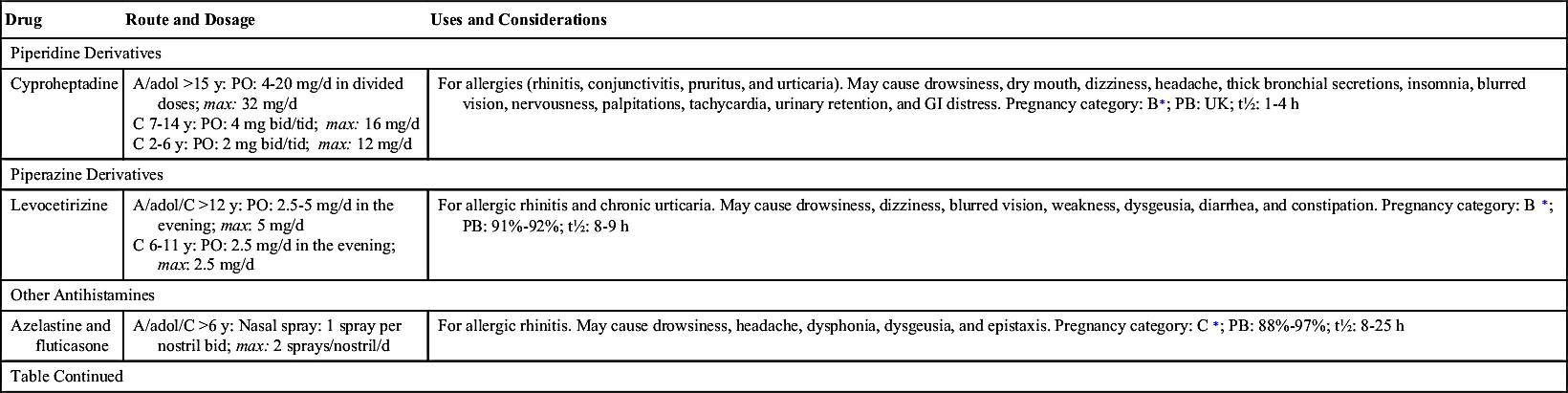
The second-generation antihistamines cetirizine, fexofenadine, and loratadine have half-lives between 7 and 30 hours. Azelastine is a second-generation antihistamine that has a half-life of 22 hours and is administered by nasal spray. Table 35.1 lists the first- and second-generation antihistamines used to treat allergic rhinitis.