Fig. 5.1
Maxillary left central incisor, labial aspect. Arrowheads: cementoenamel junction; scale bar = 5 mm
There are two premolars per quadrant and are identified as first and second premolars. The first premolar is located distally from canine, and the second premolar is positioned distally from the first premolar. Premolar can be considered as a transitional tooth during chewing, or mastication. It has the properties of both the anterior canines and molars, and so food can be transferred from the canines to the premolars and finally to the molars for grinding, instead of directly from the canines to the molars [1]. Clinical (tooth) crown of the premolars roughly indicates to the visible in the mouth exposed beyond the gingiva. And clinical crown of premolars has occlusal surface, which occludes with or contacts an opposing surface of a tooth in the opposing jaw. The molar is placed distally from second premolar and the most posterior teeth in permanent dentition. From the anterior to posterior, it consists of first, second, and third molars per quadrant (Fig. 5.2). The figure of clinical crown is different between maxillary and mandible molars. The molars have plural cusps and complex occlusal surface. The third molar is also called wisdom tooth. It usually appears after adolescence. Wisdom teeth occasionally tend to be impacted in maxilla and mandible throughout life. The primary dentition consists of central incisors, lateral incisors, canines, first molars, and secondary molars. All of these are gradually replaced by a permanent counterpart except for the primary first and second molars. First molars and secondary molars are replaced by first premolars and secondary premolars [1].


Fig. 5.2
Mandibular right first molar, labial aspect. Arrowheads: cementoenamel junction; scale bar = 5 mm
The appearance of human tooth consists of (tooth) crown and (tooth) root. The term crown can be used in two ways, namely, anatomical crown and clinical crown. The clinical crown means any part of the tooth visible in the mouth. Similarly, the term root can be used in two ways, namely, anatomical root and clinical root. The clinical root means any part of a tooth not visible in the mouth. Although the major tissues of tooth are enamel, dentin, cementum, and dental pulp, the surface of tooth is generally covered with enamel and cementum. Crown is mainly covered with enamel, and root is mainly covered with cementum. The anatomical boundary between anatomical crown and anatomical root is identified with the cementoenamel junction (CEJ), that is, the line between the enamel and the cementum, and also known as the cervical line (Figs. 5.1 and 5.2). The types of teeth are mostly classified by the shape of tooth crown that is characterized by the appearance of enamel.
The surface area of the incisors used in eating is called an incisal edge, and the tip of crown of canine is called a cusp. Premolars and molars have occlusal surface, which comes in contact with those of the opposite jaw during occlusion. The occlusal surface is formed by cusps, ridges, and sulcus (Fig. 5.3). The cusp is an elevation on an occlusal surface, and the premolars and molars have more than two cusps. The ridge is linear, flat elevations on teeth [1]. The sulcus is a groove on the occlusal surface of a tooth. The roots of teeth are embedded in the maxilla or the mandible and are usually invisible in the mouth. Some teeth have one root, while others have multiple roots. Incisors, canines, and most premolars, except for maxillary first premolars, usually have one root. Maxillary first premolars and mandibular molars usually have two roots, and maxillary molars usually have three roots. The appearance of root is usually blunt and cone-shaped, and the tip of the root is called apex. Apical foramen is an opening at the apex of the root of a tooth, and the vascular, lymphatic, and neural structures are passed through this foramen between pulp and periodontal tissue.
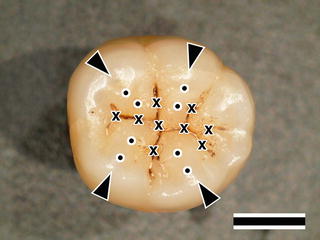
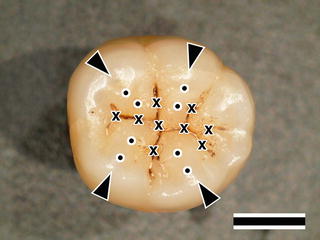
Fig. 5.3
Mandibular right first molar, occlusal aspect. Arrowheads: cusps, Cross: sulcus, Dots: ridges; scale bar = 5 mm
In vertical section of a tooth, pulp cavity, which is the central cavity of a tooth containing the pulp, is observed (Fig. 5.4). The pulp cavity is surrounded by dentin, and the appearance of pulp cavity is not similar to that of tooth. The wide pulp cavity of the tooth crown is called pulp chamber, and the root canal is a narrow part of the pulp cavity extending from the pulp chamber to the apical foramen. The dental pulp in nature occupies the pulp chamber. And the pulp in pulp chamber is called coronal pulp and that in root canal is called radicular pulp [1]. Because dentin is covered by enamel in crown and cementum in root, it is hardly occurred that dentin is directly exposed to the outside alone.
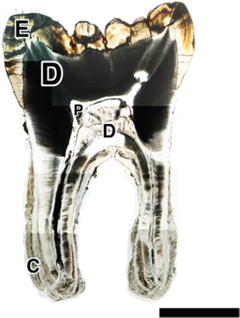
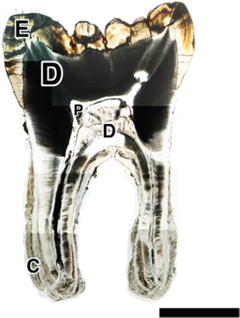
Fig. 5.4
Mesiodistal section of a mandibular first molar. C Cementum, D Dentin, E Enamel, P Pulp chamber, Bar = 5 mm
A tooth is embedded in (dental) alveolus, which is the sockets in the jaws, and the alveolar bone (alveolar process) is the thickened ridge of bone that contains the alveolus. Because a tooth root is not attached to an alveolus, there is a narrow space between them, which is called periodontal space. It contains a periodontal ligament, which is a fibrous connective tissue connecting the cementum on the root and alveolar bone. The periodontal ligament serves to hold the tooth in its socket and plays a role of periodontal mechanoreceptors. Gingiva consists of a mucosa (mucous membrane) that lies over the mandible and maxilla inside the mouth. It surrounds and supports the teeth and is tightly bound to the underlying alveolar bone, which helps resist the friction of food passing over them. Although the gingiva is penetrated by the tooth, the margin of the gingiva is attached to the surface of enamel (epithelial attachment) [2].
5.2 Enamel
5.2.1 Composition and Structure of Enamel
Tooth enamel is the only tissue of tooth, which is exposed to the oral cavity. It is the hardest substance in the human body, which covers a tooth crown and is formed by ameloblasts. It contains the highest percentage (>95 %) of minerals with very small amount of organic component (<1 %) and water [3]. Enamel has the semitransparent and milky-white appearance, and its color tends to vary from light yellow to grayish with aging. Because enamel is united to dentin by intervening with the dentinoenamel junction (DEJ), the appearance of a tooth is reflected by the color of dentin and any restorative dental material underneath the enamel. Within molars, the thickness of enamel is the largest near the cusps (up to approximately 2.5 mm) and then decreases to a minimum closest to the base of the crown [4]. The enamel has some outstanding mechanical properties with brittleness. The Vickers hardness ranges of enamel are from approximately 3 GPa to 6 GPa, and the elastic modulus ranges from 70 GPa to nearly 120 GPa [4]. It is a poor conductor for heat and electric current, displaying birefringence [5].
The tooth enamel is occupied by more than 95 wt% of inorganic compound, which primarily consists of calcium phosphate. Because its crystal structure is the same as that of apatite stone, hydroxyapatite (Ca10(PO4)6(OH)2) serves as a prototype of the inorganic component of enamel. Although biologic apatites that are involved in teeth and bones are analogues of geologic hydroxyapatite, the physical and chemical properties of the crystals in teeth and bones are different from those of geologic hydroxyapatite. Because they have highly disordered, non-stoichiometric structures with numerous point deficiencies, and carbonate substitutions, these structures refer to “bioapatite” as distinct from stoichiometric hydroxyapatite [6]. The hydroxyapatite crystallizes in the hexagonal crystal system, and the unit cell of hydroxyapatite comprises three axes, 0.942 nm on a- and b-axis and 0.688 nm in c-axis. The hydroxyapatite lattice contains two kinds of calcium positions: columnar and screw axes. The columnar calcium forms a series of hexagons, and the screw axis calcium is arranged in triangles around the central axis c. Because the apatite structure permits substantial variation in its structure, other atoms can substitute each one of these atoms; Ca2+ can be replaced by Na+ or Mg2+, PO4 3− can be replaced by CO3 2−, and OH− can be substituted by F− or Cl− [7].
The fundamental morphologic unit of enamel structure is enamel prism, and it is a structural unit approximately 4 μm in width and consists of numerous crystals of the hydroxyapatite (Fig. 5.5). The enamel prisms are arranged in a columnar fashion, extending from the dentinoenamel junction (DEJ), which is the interface between the dentin and enamel, to the enamel surface (Fig. 5.6). The enamel crystal composed of bundles of 40–60 nm wide apatite crystals with aspect ratios reaching up to 1:10,000 so demonstrates at least 100 μm long and is ~ 10× larger than those of bone or dentin [8]. The enamel prisms appear as a group of keyhole-shaped or tadpole-shaped structures, approximately 6–8 μm in diameter with the enlarged portion of the keyhole called the head and the narrow portion the tail [9]. The prisms have cross-striations that are corresponding periodic features visible in the light microscope as slight striations perpendicular to the axis of the prism at regular intervals of approximately 3–4 μm (range 2–8 μm). They are the result of a circadian rhythm in the metabolic activity of ameloblasts. Also, the crystals’ pattern of enamel is defined by both ameloblasts and Tomes’ processes, which are distal cytoplasmic processes of ameloblasts. The outer surface of enamel frequently lacks the normal arrangement of prisms (prismless enamel) but is arranged either in continuous layers parallel to the surface.
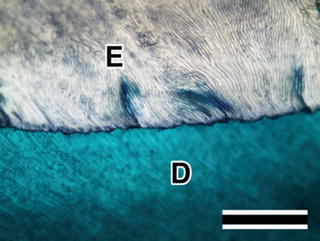
Fig. 5.5
Enamel prism. The enamel prisms are arranged in a columnar fashion and appear as a group of keyhole-shaped or ts structures. Villanueva bone stain; scale bar = 50 μm
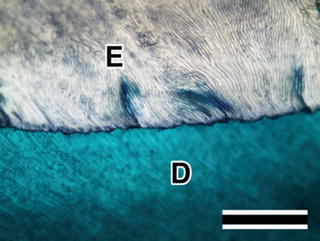
Fig. 5.6
Dentinoenamel junction (DEJ) is the plane of meeting between dentin (D) and enamel (E) on the crown of a tooth. Villanueva bone stain; scale bar = 100 μm
5.2.2 Formation of Enamel
The tooth germ has the potential of developing into a tooth and is a mass of tissue, including the enamel organ, dentinal papilla, and dental sac (dental follicle). The enamel organ is a mass of ectodermal cells derived from the dental lamina and develops the ameloblast layer of cells. Amelogenesis is the formation and development of dental enamel and is considered to have two stages, unlike the formation of bone or dentin having one stage. The first stage is known as the secretory stage, and the second is the maturation stage [10]. During the secretory stage, secretory ameloblast is synthesized and secretes enamel proteins (e.g., mainly amelogenin and enamelin) and provides an organic template form in which the enamel crystals grow [10]. As soon as this organic matrix is secreted, it becomes partially mineralized, and the full volume of enamel tissue bundles into prisms in this stage. In the maturation stage, secretory ameloblast is transformed to maturation ameloblast, and the selective loss of enamel proteins (mostly amelogenin) and water as well as massive influx of calcium and phosphates, which provides for growth of hydroxyapatite crystals of the inorganic component, is occurred. During the process, mineralization of the enamel is completed.
The inner enamel epithelium is innermost layer of enamel organ, and the dental papilla contains cells that develop into odontoblasts, and the junction between the dental papilla and inner enamel epithelium determines the crown shape of a tooth. The inner enamel epithelium, which is a layer of columnar cells located on the rim nearest the dental papilla of the enamel organ in a developing tooth, begins its differentiation first into differentiating ameloblast. Then, the differentiation of secretory ameloblast from differentiating ameloblast is completed by the formation of Tomes’ processes. Enamel deposition starts at the dentinoenamel boundary, on top of mineralized mantle dentin, which is the peripheral portion of dentin adjacent to the enamel [11]. It has been stated that amorphous calcium phosphate (ACP) plays a special role as a precursor to bioapatite and as a transient phase in biomineralization [12]. ACP can transform to DCPD (dicalcium phosphate dihydrate) or OCP (octacalcium phosphate) [13]. Also, non-apatitic calcium phosphates (e.g., ACP, DCPD, OCP) can transform to apatites and substituted apatites or other calcium phosphates by dissolution-precipitation processes in biologic systems [14]. The early mineralized enamel crystals appear thin ribbonlike structure [15]. In the secretory stage, secretory ameloblasts are polarized columnar cells with abundant rough endoplasmic reticulum, secretary granules, and Golgi apparatus and form full volume of enamel tissue in immature enamel.
The organic component of immature enamel is mainly composed of enamel proteins, although that of bone and dentin is mainly composed of type I collagen. The enamel proteins contain amelogenin, enamelin, ameloblastin, enamel proteinase, and so on. And amelogenin is the major structural protein of the enamel organic matrix and constitutes more than 90 % of the enamel’s protein content [16]. They are released into the surrounding area, and the ameloblast moves away from the interface with dentin during the synthesis of enamel. In secretory stage, Ca2+-ATPase is presented in the entire plasma membrane of the secretory ameloblasts, and it is involved in the excretion of Ca2+ to the extracellular fluid [17].
Transitional stage is situated between the secretory stage and the maturation stage, and the morphology of the ameloblasts is changed from secretory ameloblasts into maturation ameloblasts. The height of ameloblast is decreased, and protein synthesis is considerably reduced. Also, this stage is featured by a reduction in the number of ameloblasts through apoptosis.
The maturation stage is featured by selective loss of enamel proteins and water as well as massive influx of calcium and phosphates, which provides for growth of hydroxyapatite crystals of the inorganic component. Maturation ameloblasts include two distinctly different types, ruffle-ended and smooth-ended, depending on the morphology of their distal ends [17]. Because the ruffle-ended ameloblasts were dominant and have a distinct distribution of Ca2+-ATPase, they suppose to play an important role in enamel maturation [17]. During the maturation stage, rapid growth and thickening of the crystallites occur, which is associated with progressive degradation and eventual removal of the enamel extracellular matrix components mainly amelogenins [18]. Amelogenin is distributed in the sheath space, and enamelin mostly presents in the rod and inter-rod enamel. During the growth of the crystals, the sheath space decreases and removal of amelogenin has occurred, so a little amount of enamelin remains the crystal surface [18].
When the maturation stage is completed, the maturation ameloblasts lose their differentiation and become short cuboidal cells, namely, the reduced enamel epithelium. It remains on the surface of fully formed enamel until the tooth erupts and protects enamel from being in contact with connective tissue cells in the dental sac. The reduced enamel epithelium and the oral epithelium cooperatively form the dentogingival junction of the erupting tooth. When a tooth erupts and in the oral cavity, the enamel has not yet received post-eruptive maturation. At this point, the enamel is more porous with larger carbonated apatite concentration, a greater percentage of impurities (sodium, magnesium, etc.) in its composition, and more sensitive to demineralization [19]. In this stage, an ionic exchange may occur between the enamel and outer environment (saliva, oral biofilm) [20]. Because the saliva contains sufficiently high concentrations of calcium and phosphate, it makes the enamel surface more resistant to demineralization [20]. Because the thickness of crystallites increases and crystallites are closely joined and fused, intercrystalline spaces are narrowed [21].
5.3 Dentin-Pulp Complex
5.3.1 Composition and Structure of Dentin
Dentin is a highly mineralized tissue containing large quantities of collagen fibers in the matrix and the most amount of constituent of a tooth. Because dentin is covered by enamel on tooth crown and cementum on tooth root, it is invisible in the mouth [1]. And it is formed by odontoblasts and includes inside pulp cavity that contains dental pulp (Fig. 5.4). The color of dentin reflects that of a tooth crown, and its original color is light yellow and light brown and becomes dark shade with aging. When the complete degeneration of pulp has happened, its color turns to brownish and dark grayish, because the pigments are derived from degradation products of pulp and blood deposit in dentin. Dentin is an opaque tissue due to the presence of numerous dentinal tubules, and the thickness of dentin is approximately 3.5 mm [22]. The microhardness ranges of dentin are from approximately 0.25–0.8 GPa [23], and the Young’s moduli lie between 20 and 25 GP [24]. Dentin and enamel are bonded firmly, and it is considered that the elasticity of dentin protects the fracture of enamel. Dentin is composed of 70 % by weight mineral phase, 20 % by weight organic matrix, and 10 % by weight water [25]. It is less mineralized than enamel, but more than bone or cementum [25]. The thickness of these crystallites is approximately 5 nm [26]. The crystals in dentin are of similar size in bone, but enamel crystals are ~10 times larger in all dimensions [6]. The small crystal size, high degree of carbonate substitution, substantial OH deficiency, presence of lattice vacancies, and the resultant increased solubility make apatite in bone, dentin, cementum, and even enamel distinct from geologic hydroxyapatite [6].
The organic matrix is constituted by ~90 % of collagen, and the majority of it is type I, and about 3 % of the collagen fibrils are composed of type III and/or type V collagens. Collagen is an insoluble fibrous protein and is one of the most abundant proteins in the body [6]. And approximately 10 % of organic matrix is composed of noncollagenous molecules, such as dentin sialophosphoprotein (DSPP), dentin matrix protein-1 (DMP-1), and proteoglycans (PGs) [25]. These noncollagenous proteins are important for the control of dentin and bone mineralization [6]. Also, dentin is a poor conductor for heat and electric current and displays weak birefringence.
Dentin is classified into two different types, mantle dentin and circumpulpal dentin. Mantle dentin, 15–30 μm thick, is the outer layer of dentin and is adjacent to the enamel or cementum. It corresponds to an initial stage of odontogenesis [25] and has mainly an atubular layer with few thin and curved tubules [25]. The circumpulpal dentin situates inside the mantle dentin and forms the largest part of the dentin layer, and it is subdivided into intertubular dentin and peritubular dentin. Hence, it is generally accepted that the structure of circumpulpal dentin represents that of dentin. Odontoblasts are large columnar cells, which produce dentin, are aligned at the surface of the dental pulp, and still remain lifetime. They demonstrate two distinct parts: a cell body and a process. The cell bodies are polarized outside the mineralized tissue, and a long process generally occupies the lumen of dentin tubule. As odontoblasts develop to polarize, they produce an orthodentin that is a tubular-shaped dentin. Although dentin is not vascularized, it is supposed that few free nerve endings extend more than 100 μm into dentinal tubules [22]. Dentinal tubules are small canals that extend across entire width of dentin, from DEJ (dentinoenamel junction) or DCJ (dentinocemental junction) to the pulp (Fig. 5.7). The number of dentine tubules is about 18,000 tubules per mm2, and the diameter of tubules varies between 2.55 and 2.90 μm [27]. The diameters of dentinal tubules are different in location, and the diameter near the pulp is larger than that at the dentinoenamel junction. The most prominent part of the circumpulpal dentin is formed by intertubular dentin, and peritubular dentin is found around the lumen of the tubules [25]. Each tubule contains the cytoplasmic process of an odontoblast and is lined with a layer of peritubular dentin, which is more mineralized than surrounding intertubular dentin. Although the dentinal tubules run a straight course in the root, they run the S-shaped curvature in coronal dentine [28]. The approximately 250 μm-wide outer zones showed typical, terminal Y-branching of the dentinal tubules [28].
Fig. 5.7
Dentinal tubules. The dentinal tubules are small canals that extend across entire width of dentin, from dentinoenamel junction or dentinocemental junction to the pulp. Villanueva bone stain; scale bar = 50 μm
The formation of intertubular dentin provides three successive layers. The innermost layer is the cellular stratum that contains odontoblast cell bodies, the second one is the immature predentin layer, and the outermost one is the mineralized dentin [25]. And the interface between the immature predentin and the mineralized dentin is called mineralization front. Because the odontoblasts migrate toward the center of the tooth forming the odontoblast process, dentinogenesis (the formation of dentin) progresses toward the inside of the tooth. The immature predentin layer has a constant 15–20 μm thickness [25]. Radioautographic data and experiments using microtubule inhibitors suggest the occurrence of flux of forces in predentin and the active transport of collagen fibrils from the proximal to the distal predentin where the mineralization process occurs [25]. Dentin mineralization often initiates that the mineralized nodule is solely found in an immature noncalcified layer of predentin that is apart from the mineralization front. It means the mineralized nodule nucleates and develops the progress of calcification that is the deposit of calcium salts in a tissue. Consequently, the developed mineralized nodules are contacted with the mineralization front and fused with mineralized dentin.
As the formation of primary dentin that continues until the eruption of a tooth is completed, the tissue of dentin can restart or reconstitute its structure by several biological stimulations including addition of dentin or altered form of dentin. The former is secondary dentin and tertiary (restorative) dentin, and the latter is transparent (sclerotic) dentin. The secondary dentin begins to form by achieving the contacts between antagonistic cusps and continues throughout life [25]. However, there is not much difference between primary and secondary dentin [25]. The tertiary (restorative) dentin is a new dentin formed in response to stimuli associated with the normal aging process, such as tooth attrition, tooth abrasion, and pathological conditions including caries, injury, and cavity preparation [22]. Because the dentinal tubules in restorative dentin are highly curved and meander with short period, they are distinguished from those in primary dentin. The transparent dentin has some dentinal tubules becoming sclerotic or calcified with the appearance of translucency. However, these dentins are not remodeled as well as cementum, whereas the bone is remodeled [6].
The formation of dentin is initiated by differentiating from the neural crest cell-derived ectomesenchymal cells present in the dental papilla near inner enamel epithelium to odontoblast [29]. When odontoblasts are differentiated, they result in highly polarized cells with a columnar shape, about 50 μm in height [30]. They have all the organelles implicated in extracellular matrix synthesis, such as rough endoplasmic reticulum, Golgi apparatus, and immature and mature secretory vesicles, associated with lysosomal equipment. And they are connected by junctional complexes forming a densely packed palisade at the dentin-pulp interface, and each cell projects an odontoblastic process into the predentin/dentin matrix [30]. Odontoblasts are essentially dentin-secretory cells that produce predentin, an extracellular matrix formed by type I collagen as the major organic component (about 90 %), together with noncollagenous proteins including glycoproteins, proteoglycans, and dentin phosphoproteins [31]. Mature mineralized dentin is molded after the formation of predentin, and this process is involved in matrix vesicle-mediated mineral deposition [32]. Matrix vesicles are extracellular 100-nm-diameter membrane-invested particles selectively located within the matrix of bone, cartilage, and predentin and serve as the initial site of calcification in all skeletal tissues [32]. Alkaline phosphatase (ALP) is an enzyme known to be essential for mineralization. Because matrix vesicles are seeded in the selected areas, the subsequent mineralization is localized. In the initial stage, the generation of hydroxyapatite mineral crystals follows within the matrix vesicle membrane. This stage is controlled by phosphatases (including alkaline phosphatase) and Ca-binding molecules. In next stage, the breakdown of matrix vesicle membranes is occurred and exposed preformed hydroxyapatite to the extracellular fluid [32]. Consequently, numerous mineralized nodules derived from matrix vesicle-mediated mineral depositions are formed in the layer of predentin, and the mineralization progressed by fusion of these nodules with mineralized dentin. Primary dentin is formed at an appositional rate of about 4–8 μm per day, allowing the bulk of the tooth to be created within 2–3 years of continuous secretion [30]. After eruption of the tooth, the odontoblast phenotype is significantly changed to the mature odontoblast stage. Their secretory apparatus is reduced, and the autophagic vacuoles that are cytoplasmic degenerative debris engulfed by primary lysozymes are presented in cytoplasm. Also, the remaining cellular organelles are relocated to the base of the cell. In human teeth, this stage may persist for decades, but finally the odontoblast reduces cell size and flattens its shape [30].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


