FNA of a thyroid nodule is performed with a fine gauge needle. This can be performed by palpation, but is best done under ultrasound guidance.
•History
•Family history (goiter, MEN, thyroid cancer)
•History of radiation
•Symptoms: Hyper/hypothyroid, compressive symptoms
•Physical exam
•Characteristics of the nodule and the gland
•Voice changes
•Lymph node status
•Diagnostic tests
•Ultrasound to document size and to look for additional nodules
•FNA, ideally under ultrasound guidance
•Thyroid scintigraphy if there is a concern of hyperthyroidism (suppressed TSH)
•Blood tests depending on history (T3/T4, TSH, thyroglobulin, thyroid antibodies, calcitonin, calcium)
•TSH is the only screening test needed in a patient without symptoms of hyper- or hypothyroidism
•If concern of clinical hyper- or hypothyroidism, free T4 is preferred to total T4 as it is not affected by levels of thyroid-binding globulin
An FNA can often distinguish benign from malignant tumors and is considered to be the gold standard initial test for the evaluation of thyroid nodules.
A 38-year-old woman is found to have a benign thyroid nodule upon FNA. What is the next step in management?
Observation is appropriate in the absence of symptoms.
Benign Thyroid Nodule
•Usually represents one of the following:
•Adenomatous or hyperplastic nodule
•Hashimoto thyroiditis
•Colloid cyst
•Follow with repeat imaging in 1 year
•Repeat FNA if nodule grows >2 mm in two dimensions
•Refer for surgery if symptomatic or if suspicion of malignancy
•T4 replacement only given to treat hypothyroidism (do not give to euthyroid patients)
What percent of FNAs performed for thyroid lesions are malignant?
5% are malignant and 75% are benign (20% are suspicious or nondiagnostic).
Malignant Thyroid Nodule
•Cancer type can sometimes be identified on FNA
•All malignant or suspicious results should be followed up with surgery
A patient with a thyroid goiter underwent thyroid function testing. What is a normal T4/T3 ratio?
A normal T4/T3 ratio is 10:1 or 20:1.
Thyroid Function Tests
•Measuring levels of thyroid-stimulating hormone (TSH) is the best test of thyroid function
•A normal T4:T3 ratio is 10:1 or 20:1 (although T3 is three times more active than T4)
•Thyroglobulin stores T3 and T4 in colloid
•Most T3 is made in the periphery by conversion from T4 (by peroxidases)
•The half-life of T3 is 1 to 3 days
•The half-life of T4 is 7 days
TSH levels provide the most sensitive indication of gland function.
A 44-year-old woman presents with an enlarged thyroid gland and pretibial edema. Lab tests reveal an undetectable level of TSH. What is the most likely diagnosis?
Graves’ disease presents with goiter and signs and symptoms of hyperthyroidism.
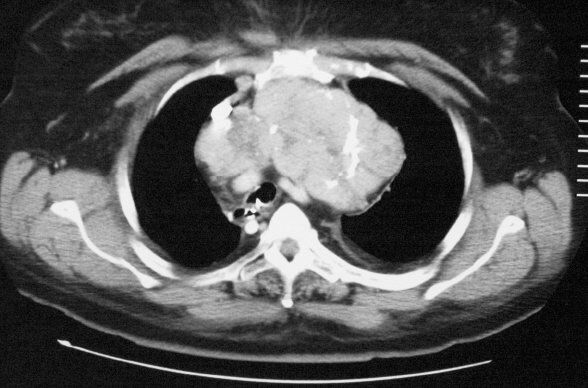
Large multinodular goiter with substernal component. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
Graves Disease
•The most common cause of hyperthyroidism
•Autoimmune IgG antibody to the TSH receptor
•Diagnosis
•Signs and symptoms include tremors, hyperreflexia, tachycardia, a-fib, thyroid enlargement, palpitation, nervousness, heat intolerance, pretibial edema, weight loss, and hair loss
•Exophthalmos is characteristic (and may not resolve with treatment)
•Labs show decreased or undetectable TSH, elevated T3, T4, and thyroid antibodies (TRAB—TSH receptor antibody, TSI—thyroid-stimulating immunoglobulins)
•A thyroid scan will reveal a diffuse goiter with high radiolabel uptake
•Obtain an ultrasound to rule out focal nodules—this is essential if cold nodules are identified on the uptake scan
Graves disease is the most common cause of hyperthyroidism.
A 33-year-old woman with Graves’ disease and severe ocular involvement has failed medical therapy. What is the next step in management?
Preoperative preparation with anti-thyroid medications (until euthyroid), beta blockade if needed, and Lugol’s solution, followed by thyroidectomy.
Treatment for Graves Disease
•Radioactive iodine is the most common therapy in the United States (except in children, pregnant women, and in those with Graves ocular disease)
•Good for patients in whom medication has failed but no clear surgical indication exists
•Pre-treat with anti-thyroid medications to establish a euthyroid state for 3 to 4 weeks if significant hyperthyroidism; discontinue medications 3 to 5 days prior to iodine treatment
•Oral iodine-131
•80-90% cure rate
•40% to 90% become hypothyroid after treatment
•Medical therapy: Propylthiouracil (PTU) and methimazole
•Inhibits the iodination of tyrosine residues in the thyroid
•If unable to wean medications off by 18 months, will likely need definitive management or lifelong treatment.
•Use PTU in the first trimester of pregnancy, otherwise utilize methimazole
•Can be associated with hepatotoxicity and agranulocytosis
•Surgery: Total (or subtotal) thyroidectomy
•Indications
•Children
•Women who want to become pregnant or are breastfeeding
•Need for rapid control (e.g., acute control of cardiac problems)
•Compressive symptoms
•If unable to rule out malignancy (suspicious nodule)
•Failure of medical management (especially in pregnancy)
•Non-compliant patients
•Patient preference for surgical management
•Pre-op preparation
•PTU or methimazole until euthyroid
•Lugol’s (iodine) solution for 10 to 15 days pre-op to decrease the friability and vascularity (Start after the patient is euthyroid!)
•β-blocker pre-op if significant tachycardia
Radioactive iodine may worsen Graves’ eye disease.
A 49-year-old woman with a goiter has vomiting and mental status changes following an elective hernia repair. On further evaluation, she is found to have a temperature of 39.2°C, a heart rate of 165 bpm, and manic symptoms. What is the next step in treatment?
Emergent medical therapy for a thyroid storm.
•A life-threatening condition
•Can occur following elective surgery in patients with uncontrolled or unrecognized hyperthyroidism
•Prevented by ensuring a euthyroid state before any surgery
•Treat with emergent
•Fluid resuscitation
•Anti-thyroid medications (PTU blocks the synthesis of thyroxine)
•Beta blockade
•Hypothermia
•Iodine solutions and steroids can also be used
What are the indications for operating on a benign goiter?
•Development of thyrotoxicosis
•Compressive symptoms
•Suspicion of malignancy
•Cosmetic concerns
A 40-year-old female presents with a tender and enlarged thyroid gland following a recent upper respiratory tract infection. What is the next step in management?
An ultrasound can help identify the need for urgent incision and drainage for a localized abscess. Both acute suppurative thyroiditis and subacute thyroiditis may present with unilateral tenderness following an upper respiratory tract infection.
The Tender Goiter
•Acute (suppurative) thyroiditis
•Due to bacterial infection—most commonly staph or strep
•Rare
•Presents with fever, redness, fluctuance, and elevated WBC
•Have normal thyroid function tests
•Ultrasound can localize the abscess
•Treatment is operative incision and drainage
•Subacute thyroiditis
•De Quervain thyroiditis
•Due to a viral infection
•Have a URI prodrome and a painful, enlarged thyroid
•Lab tests: ↑fT4, ↓TSH, and ↑ESR
•Treatment is nonsteroidal anti-inflammatory drugs and occasionally steroids
•Usually self-limited (2 to 3 weeks)
•Post-partum thyroiditis
•Autoimmune
•Patients are usually asymptomatic
•Lab tests: ↑fT4, ↓TSH, and normal ESR
•Treat symptoms of hyperthyroidism
•Chronic thyroiditis
•Hashimoto thyroiditis (see below)
•Riedel thyroiditis
•Autoimmune
•Symptoms: Woody, enlarged thyroid that can cause compressive symptoms of the airway or esophagus
•Associated with sclerosing cholangitis, retroperitoneal fibrosis, and other fibrotic diseases
•Diagnosis: Lymphocytic infiltration of thyroid
•Treatment
•Tamoxifen or steroids
•Surgery (isthmectomy or tracheostomy) for compressive symptoms
A 45-year-old woman with no significant medical history presents to your office complaining of excessive fatigue. Notably, 2 months ago, she had more energy than she had ever had and was having palpitations. At that time, she also lost 5 pounds. Then, over the last 2 months, she had a slow decline in her energy that was also associated with weight gain. Her mother has a history of systemic lupus erythematosus. What is the patient’s most likely diagnosis?
She has Hashimoto thyroiditis.
Hashimoto Thyroiditis
•The most common cause of hypothyroidism in adults
•Autoimmune disease affecting the thyroid
•Labs
•Anti-Tg and anti-thyroperoxidase antibodies
•Have both humoral and cell-mediated immune disease due to microsomal and thyroglobulin antibodies
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


