What is the normal pressure within the bile duct compared to the pancreatic duct?
The pancreatic duct has a higher resting pressure compared to the bile duct, which prevents bile reflux into the pancreatic duct. The pressure in both ductal systems increases following meals.
What are the pancreatic enzymes and hormones?
Exocrine Pancreas
•Amylase
•Responsible for the digestion of dietary carbohydrates consisting primarily of starch, sucrose, and lactose
•Secreted by the salivary glands (S-type amylase) and by the pancreas (P-type amylase)
•Digestion begins in the mouth where 30% to 40% of starch is converted to maltose, isomaltose, and dextrins before S-amylase is inactivated by gastric juice
•Pancreatic amylase completes the hydrolysis of the remaining starch in the jejunum
•Lipase
•Most sensitive marker of pancreatitis
•Amylase and lipase are secreted in their active forms, unlike trypsinogen and phospholipase A2, which are activated by duodenal enzymes
•Endocrine Pancreas
•Cells
•Alpha cells  Glucagon
Glucagon
•Beta cells  Insulin
Insulin
•Delta cells  VIP
VIP
•G-Cells  Gastrin
Gastrin
•GI hormones that increase pancreatic activity
•Secretin (released in response to a low duodenal pH)
•Cholecystokinin
•Acetylcholine (vagal stimulation) secretions
•Gastrin
•Serotonin (less important)
•GI hormones that decrease pancreatic activity
•Somatostatin
•Glucagon
Somatostatin (or its long-acting analogue octreotide) has many therapeutic applications including the treatment of diarrhea and flushing in carcinoid syndrome and the treatment of intestinal fistulas and variceal bleeding.
Secretin is the primary stimulant of pancreatic water and electrolyte secretion. The bicarbonate concentration in pancreatic secretions is increased when the pancreas is maximally stimulated due to carbonic anhydrase activity in the pancreatic duct.
A 6-month-old boy with Down syndrome presents with a gastric outlet obstruction. An annular pancreas is suspected. What is the best test to establish the diagnosis?
An upper GI contrast study is the diagnostic test of choice for an annular pancreas.
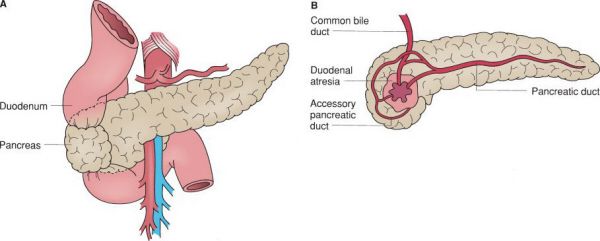
Annular pancreas. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
Annular Pancreas
•Pancreas encircling the second part of the duodenum
•Due to incomplete rotation of the ventral pancreatic bud
•Associated with trisomy 21
•An UGI is diagnostic
•Most patients are asymptomatic
•The treatment is a duodenojejunostomy and should be reserved for symptomatic patients
•The pancreas is NOT resected as the band around the duodenum frequently carries a pancreatic duct remnant
The treatment of symptomatic annular pancreas is bypass rather than resection.
A 31-year-old woman presents with recurrent epigastric pain radiating to her back and a history of pancreas divisum. What is the most likely cause of her symptoms?
In pancreas divisum, two separate ductal systems drain bile and pancreatic juice into the duodenum via a major and minor papilla. It is associated with recurrent episodes of acute pancreatitis.
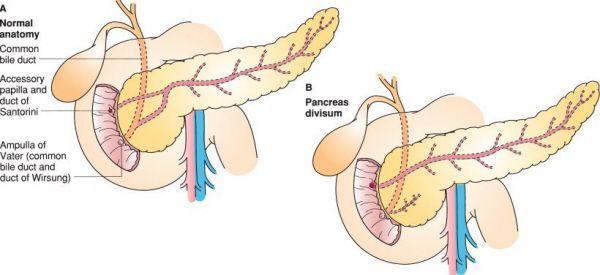
Pancreas divisum. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
•Failure of pancreatic duct fusion at the time of developmental rotation
•The smaller duct (duct of Santorini) often drains the majority of the pancreas in this condition
•Found in up to 11% of the population and often asymptomatic
•ERCP is the gold standard for diagnosis
•Demonstrates two non-communicating ductal systems
•Main treatment option is endoscopic sphincterotomy
Pancreas divisum is associated with recurrent episodes of acute pancreatitis and can lead to chronic pancreatitis, a condition in which the pancreatic gland is hardened and the ductal system is often dilated.
What is the most sensitive test for pancreatitis?
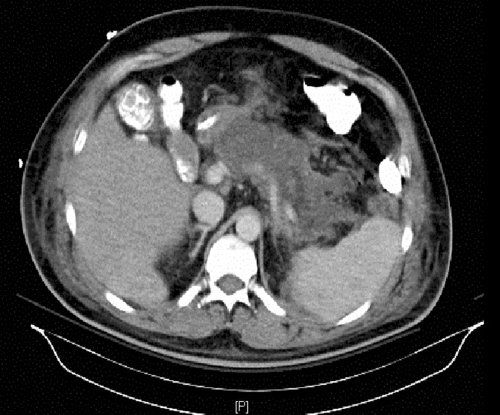
A CT scan with IV contrast is the best radiographic study for pancreatitis. Serum lipase is the most sensitive and specific lab test.
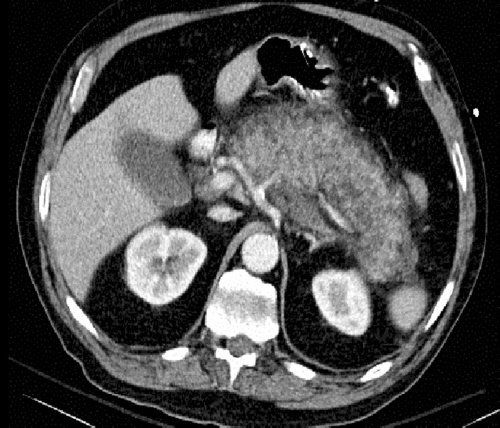
Acute pancreatitis on CT scan. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
Acute Pancreatitis
•Serum lipase is a more sensitive and specific test than amylase for acute pancreatitis
•Amylase is often elevated but returns to baseline values sooner than lipase
•Amylase levels can be elevated from other conditions
•Bowel obstruction
•Bowel necrosis
•Perforated duodenal ulcer
•Salivary tumors
•Amylase level may not correlate with the degree of the pancreatitis
•Pancreatitis can present with normal serum amylase levels for the following reasons:
•Amylase is rapidly cleared by the kidneys
•Pancreatic parenchyma can be destroyed in chronic pancreatitis (i.e., the pancreas has exhausted its enzymatic production capacity)
•Hyperlipidemia interferes with amylase determination
•ERCP is a poor test for pancreatitis and can induce or worsen pancreatitis 5% to 15% of the time
•Ranson criteria are not clinically useful for the following reasons:
•Ranson criteria only predict outcomes based on initial presentation: age, WBC, glucose, LDH, AST, BUN, PaO2, Ca, Hct, base deficit, and fluid sequestration
•It is limited by the 48-hour waiting period and the inability to recalculate the score throughout the patient’s clinical course
•Even low-grade pancreatitis can spontaneously lead to infected pancreatic necrosis and death
Elderly patients with new-onset pancreatitis have pancreatic cancer until proven otherwise.
A 35-year-old morbidly obese woman presents with pancreatitis. What is the most likely etiology?
Gallstones are the most common cause of acute pancreatitis in the United States.
Causes of Acute Pancreatitis
•Gallstones (35% to 45% of cases)
•Alcoholic pancreatitis (30% to 40%)
•Idiopathic/other (30% to 35%)
•ERCP, viruses, medications (antiretrovirals, azathioprine, and others)
•Trauma is a common cause of pancreatitis in children
A 41-year-old woman presents with new-onset epigastric and right upper quadrant pain. Her total bilirubin is 4.1, amylase 2500, and lipase 2800. Magnetic resonance cholangiopancreatography (MRCP) demonstrates common bile duct stones and pancreatitis. When should a cholecystectomy be performed?
The management of gallstone pancreatitis is conservative (supportive) until symptoms improve. Once the pancreatitis resolves, a laparoscopic cholecystectomy should be performed prior to discharge.
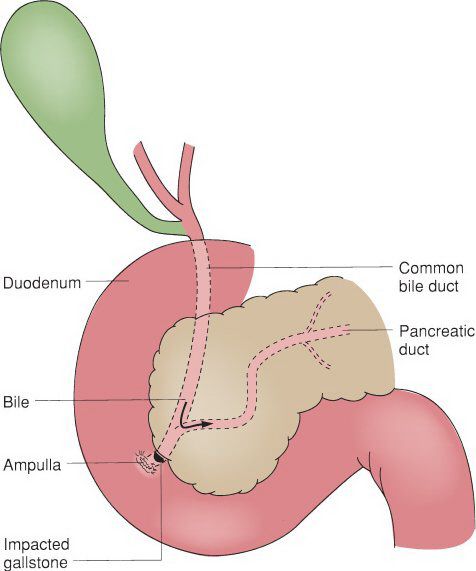
Gallstone in common bile duct leading to gallstone pancreatitis. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
•Pancreatitis caused by a stone passing through the common bile duct (CBD)
•Associated with increased liver function tests (LFTs), amylase, and lipase
•Following LFTs and clinically distinguishing biliary “colic” from pancreatitis symptoms can be useful in determining whether or not a stone has passed
•Transabdominal ultrasound is poor for looking at stones in the common bile duct, but it does identify CBD dilatation, a finding consistent with CBD stones
•A normal CBD diameter is 4 to 6 mm, with an increased normal limit for older patients (1 mm larger per decade over 50)
•The CBD is normally dilated post cholecystectomy (because the CBD accommodates for a missing gallbladder)
•MRCP is the screening test of choice for common bile duct stones
Laparoscopic cholecystectomy for gallstone pancreatitis should be performed during the same admission. Interval laparoscopic cholecystectomy should be avoided because of the high risk of recurrent gallstone pancreatitis.
A 47-year-old alcoholic presents with severe pancreatitis and signs of early sepsis. He is febrile and has a markedly increased white blood cell count, but is hemodynamically stable. What is the next diagnostic step in management?
A CT scan is critical for making the important diagnosis of necrotizing pancreatitis. Ascending cholangitis should also be considered with the above clinical picture. The total bilirubin is classically elevated in cholangitis.
Necrotizing pancreatitis on CT scan. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
Necrotizing Pancreatitis
•Hypoperfusion of the pancreas results in necrosis which can be sterile or infected
•Distinguishing sterile versus infected necrosis can be difficult
•Subtle or overt signs of sepsis often accompany infected necrosis
•Gas in the pancreas is pathognomonic for infected necrosis
•Infected necrosis requires operative necrosectomy or percutaneous drainage
•Sterile necrosis with clinical improvement should be managed nonoperatively
•Percutaneous drainage should not be performed as it can introduce bacteria and convert the sterile necrosis into infected necrosis
•A necrosectomy can be performed with several variations in management: Open packing, closed packing, repeat second-look laparotomies, and continuous lavage
•Treat infected necrosis with broad spectrum antibiotics (carbapenems)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


