Tension pneumothorax. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
•Chest X-ray (CXR): No mediastinal shift
•Small pneumothoraces can be observed
•Large or expanding pneumothoraces mandate a chest tube
•Tension pneumothorax
•Signs/symptoms
•Jugular venous distention (JVD)
•Tracheal shift
•Hypotension
•Narrowed pulse pressure
•The diagnosis is made clinically—treatment should NOT be delayed to obtain a CXR
•Treat with needle decompression followed by immediate chest tube placement
•Hemothorax
•Blood in the chest cavity
•Treat with a chest tube (use small tubes for air and large tubes for blood)
•Blood will organize and clot in 3 to 10 days and may no longer drain; surgical evacuation via thoracoscopy (VATS) may be required to remove the blood at that point
Indications for Thoracotomy Following Chest Tube Placement
•Immediate drainage of 1500 mL of blood after chest tube placement
•Continued drainage of 250 mL/hour over 4 hours
•Drainage of 2500 mL in 24 hours
•Bright red arterial blood (much less likely to cease spontaneously)
•Significant air leak resulting in hypoxemia
•Persistent hemothorax despite adequate drainage with two chest tubes
If hemothorax is suspected, place a large chest tube (32 to 36 French) to prevent clotting.
A 30-year-old male is brought to the emergency department (ED) by paramedics after sustaining several gunshot wounds to the chest. In the field, he has a heart rate of 120 and a systolic blood pressure of 80. He is intubated. Upon entry to the trauma bay, he becomes asystolic. What is the next step in management?
An immediate ED thoracotomy is indicated for a sudden loss of vital signs with penetrating trauma to the chest.
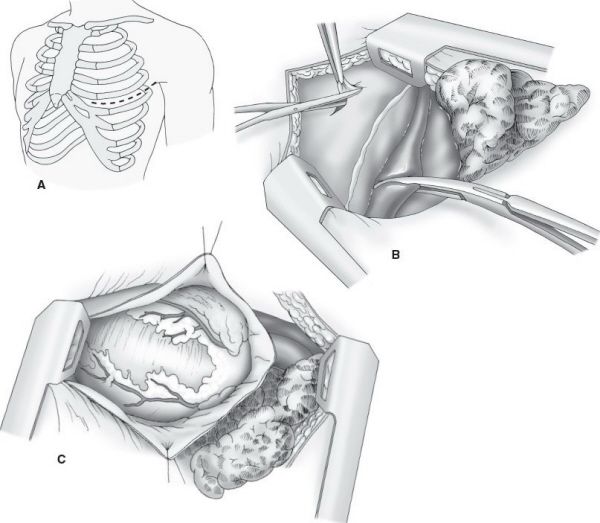
ED thoracotomy. (With permission from Fischer JE, Bland KI, Callery MP, et al., eds. Mastery of Surgery. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.)
Indications for Emergency Department Thoracotomy
•Penetrating torso trauma with witnessed loss of vital signs in transit or in ED
•Blunt torso trauma with loss of vital signs in the ED
•Thoracotomy procedure
•Identify the left fifth or sixth rib (just below the nipple line in men, just below the inframammary crease in women) and make an incision down to bone from the sternum to the posterior axillary line
•Carry incision through subcutaneous tissue and muscle to enter the pleural space
•Sweep the left lung away
•Bluntly dissect the mid-descending thoracic aorta circumferentially and place an aortic cross-clamp
•Make a large longitudinal pericardiotomy medial to the phrenic nerve and examine heart for injuries
•Temporize any cardiac wounds with a stitch, a Foley balloon, or your finger
•For an arrested heart, begin cardiac massage and go to the operating room
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


