Video-assisted thoracoscopic surgery treatment of an empyema. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, et al., eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
Empyema
•Pus in the pleural space
•Characteristics of pleural fluid with empyema: pH < 7.0, glucose < 40 mg/dL, protein > 3 g/dL, LDH > 1,000 IU/L
•The most common etiology is pneumonia (called a parapneumonic effusion)
•Exudative phase (<24 hours): Treat with intravenous antibiotics and thoracentesis
•Fibropurulent phase (24 to 72 hours): Treat with intravenous antibiotics, chest tube thoracostomy, and consider intrapleural fibrinolytic agents (i.e., streptokinase)
•Organized phase (>72 hours): Treat with intravenous antibiotics, consider chest tube thoracostomy, and intrapleural fibrinolytic agents
•More likely to require video-assisted thoracoscopic surgery (VATS) or limited thoracotomy with rib resection
•Complicated cases will require decortication (i.e., removal of constricting peel over the lung) and a muscle transposition flap
Staphylococcus and Streptococcus are the most common organisms cultured from an empyema.

An 8-year-old student in primary school develops progressive wheezing unresponsive to inhaled nebulizers. Bronchopulmonary evaluation demonstrates a tracheal lesion. What is the most likely diagnosis?
Benign tracheal papilloma.
Benign Tracheal Papilloma
•Most common in children
•Usually multifocal
•Associated with human papilloma virus 6 and 11
•Treat with endoscopic laser ablation
•High tendency for recurrence
A 17-year-old man develops sudden shortness of breath while watching TV. He has no medical history of lung disease or recent trauma. A CXR demonstrates a large right pneumothorax. What is the most likely etiology?
A ruptured apical bleb is the most common etiology of a non-traumatic, non-iatrogenic pneumothorax.
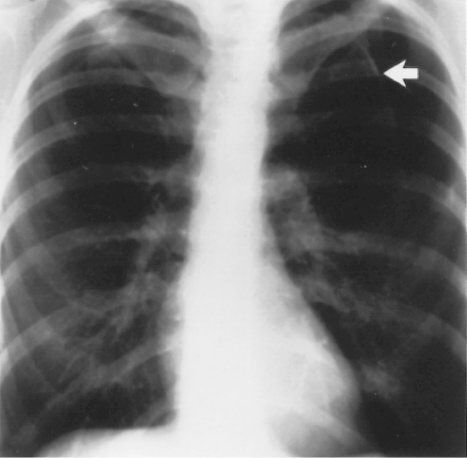
Pneumothorax. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, et al., eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
Primary Spontaneous Pneumothorax
•Occurs due to the rupture of small apical blebs (a bleb is <2 cm whereas a bulla is >2 cm in size).
•Typically occurs in tall, thin men between the ages of 20 to 35 years
•A physical exam should be directed to rule out Marfan disease
•Typically presents with chest pain and dyspnea
•Obtain a CT scan to establish the size of the pneumothorax and delineate associated parenchymal disease
•Indications for surgery
•Recurrence after first episode (most common indication)
•First episode, complicated by persistent air leak or hemothorax
•Failure of the lung to re-expand
•Tension pneumothorax on the first episode
•Bilateral pneumothorax on the first episode
•Absence of medical facilities in isolated regions
•Occupational hazard (i.e., pilot, deep sea diver, etc.)
A 39-year-old is in a motor vehicle accident. CXR reveals an incidental 2-cm pulmonary mass with popcorn calcifications. What is the most likely diagnosis?
Pulmonary hamartoma.
Pulmonary Hamartoma
•Round lesions located in the periphery of the lung
•Typically slow growing
•Represent 10% of all pulmonary nodules
•The majority are discovered incidentally, but they can also present with pneumonia, atelectasis, or hemoptysis
•Diagnosed by CXR (“popcorn” calcification), spiral CT, bronchoscopy, and FNA (fine needle aspiration)
•Treated with enucleation or wedge resection
A 64-year-old smoker is found to have a mass obstructing the left mainstem bronchus on radiographic studies. During bronchoscopic examination under general anesthesia, a biopsy specimen is taken. The patient immediately develops hemorrhage from this site. What is the next step in management?
Management of a Hemorrhagic Bronchial Biopsy Site
•Advance the bronchoscope to the mainstem bronchus proximal to the site of hemorrhage
•Advance the endotracheal tube over the bronchoscope to diminish spillage to the contralateral lung
•Working through the bronchoscope lumen, apply topical epinephrine (0.2 mg of epinephrine in 500 cc of lactated ringers)
•Consider cauterization, tamponade with epinephrine soaked gauze, or selective balloon tamponade
You have been carefully following a patient with an SPN in your thoracic surgery clinic. What is the most likely pathology of a lung nodule based on doubling time?
Doubling Time of Nodule Size
•<20 days, most likely infectious in nature
•20 to 400 days, most likely a pulmonary malignancy
•>400 days, likely a benign lung mass
Six weeks after extubation following a prolonged ICU course, a 28-year-old man reports shortness of breath on exertion. A CXR is normal. What is the most likely diagnosis?
Post-intubation stenosis.
Post-intubation Stenosis
•Presents as dyspnea on exertion 1 to 6 weeks after extubation
•Symptomatic with luminal narrowing of >50%
•Diagnosed by bronchoscopy and CT scan
•Treatments include dilation using rigid bronchoscopy, laser resection, internal stents, tracheal reconstruction, segmental resection and primary anastomosis, and permanent tracheostomy
What is the lifetime risk of developing lung cancer in smokers?
10%.
Tobacco Use
•25% of all Americans smoke
•The relative risk of smokers to non-smokers in developing lung cancer is 13
•90% of lung cancer is attributable to tobacco use
•The overall 5-year survival for lung cancer is 10%
•After lung cancer, the other most common cancer in smokers is head and neck cancer
A 72-year-old patient undergoes a tracheostomy and gastrostomy tube after a cerebrovascular accident. Three weeks later, while awaiting rehabilitation placement, he becomes acutely hypotensive and develops profuse bleeding from his tracheostomy site. What is the next step in management?
Place a finger in through the tracheostomy site and put pressure over the artery to control the bleeding. Then, as soon as possible, perform emergent intubation and proceed to the operating room for evaluation of a possible tracheoinnominate artery fistula.
Tracheoinnominate Artery Fistula
•Management centers on control of the airway, control of bleeding, and resuscitation of the patient
•Hyperinflate the tracheostomy balloon
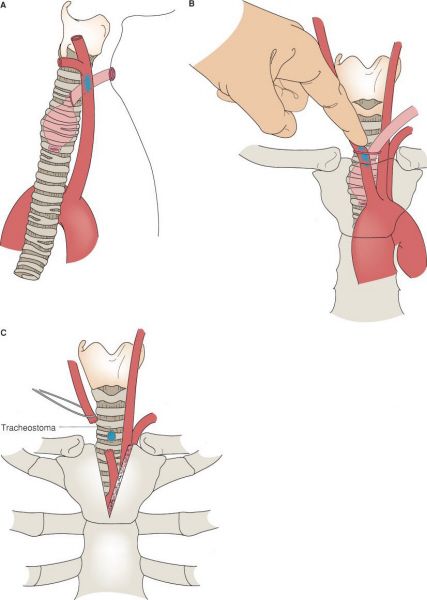
Management of a tracheoinnominate fistula. (A) Tracheal innominate artery anatomy. (B) Manually compress the innominate artery. (C) The innominate artery is typically divided with no reconstruction. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, et al., eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
•Place an endotracheal tube above the tracheostomy
•If hyperinflating the tracheostomy tube fails to control the bleeding, remove the tracheostomy tube, and manually compress the innominate artery while advancing the endotracheal tube
•Alternatively, use a rigid bronchoscope to compress the tracheostomy balloon against the innominate artery
•Once the bleeding is controlled, take the patient emergently to the operating suite for surgical repair of the tracheoinnominate fistula
•The innominate artery is typically divided with no reconstruction
An 18-year-old intoxicated college student presents to the emergency department after a motor vehicle crash. He is requiring 4 L of oxygen via nasal cannula and has paradoxical motion of his chest wall. What is the most likely diagnosis?
Flail chest.
Flail Chest
•Fracture of at least three ribs, each in a separate location resulting in paradoxical motion of a segment of chest wall
•Treatment should focus on pain control with a patient-controlled analgesia (intravenous or epidural) and aggressive pulmonary toilet
•Indications for surgery include failure to wean from mechanical ventilation and severe cosmetic deformity
•Surgically managed by internal fixation (wire sutures, intramedullary wires, Judet staples) or external fixation (metal plate)
A 58-year-old retired carpenter presents with facial flushing, right upper arm edema, dyspnea, and a cough. What is the most likely diagnosis?
Superior vena cava (SVC) syndrome.
Superior Vena Cava Syndrome
•Partial or complete obstruction of the SVC with possible intraluminal venous thrombosis
•More common in men between the ages of 50 and 70 years
•95% are due to malignancy
•Most common associated malignancy is small cell bronchogenic cancer
•Also associated with infectious, catheter-related, or other rare causes
•May present with facial fullness or flushing, headache, dyspnea, and cough
•Less common complaints include edema of the upper extremities, pain, dysphagia, and syncope
•Physical findings include prominent distended and tortuous venous systems in the face, neck, and upper trunk; facial cyanosis; and pleural effusion
•Once diagnosed by CT scan, a tissue diagnosis can be made by bronchoscopy, FNA biopsy, or mediastinotomy
•Surgical intervention is NOT recommended except in select individuals with a benign etiology
•Steroids can be temporizing
•Chemotherapy, radiation therapy, or both can effectively relieve the signs and symptoms arising from malignant disease
A 35-year-old female nurse’s aide presents to her primary care doctor with neck and shoulder pain with intermittent paresthesias in the medial aspects of her arm and her fourth and fifth fingers. Physical exam findings reveal that her symptoms can be reproduced by lifting her arms over her head. Chest radiograph and shoulder X-rays reveal a cervical rib. What is the next step in management?
Surgery is not the first step in the management of thoracic outlet syndrome. The patient should be placed on a physical therapy regimen prior to consideration for surgery.
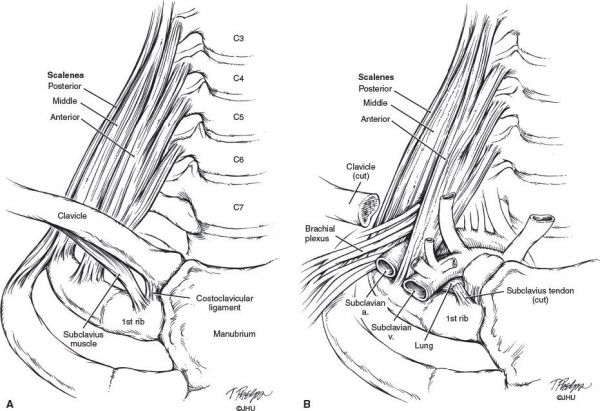
Anatomy of scalenes, brachial plexus, subclavian artery and vein, and first rib. (With permission from Fischer JE, Bland KI, Callery MP, et al., eds. Mastery of Surgery. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.)
Thoracic Outlet Syndrome
•Compression of the brachial plexus (90%), subclavian artery, or subclavian vein against the cervical rib, the anterior scalene, and/or the middle scalene muscle
•Cervical and chest radiographs can be diagnostic
•For concerns of arterial compression or venous compromise, vascular studies are indicated
•Medical management is typically 85% successful (exercise to improve posture and weight reduction to relieve pressure)
•Surgery typically entails rib resection and release of the scalene muscles
•Indications for surgery include
•Failure of conservative treatment
•Arterial complications (occlusion, aneurysm, or distal emboli)
•Venous thrombosis
Thoracic outlet syndrome is most commonly neurogenic (not vascular) and can often be treated medically.
A 51-year-old female develops progressive right-sided pleuritic chest pain. CXR and CT scan are suspicious for the presence of a pleural-based tumor. What is the most likely diagnosis?
Metastatic tumors (lung and breast) are the most common pleural tumors (90%). Mesothelioma is the most common primary malignant pleural tumor.
Malignant Mesothelioma
•
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


