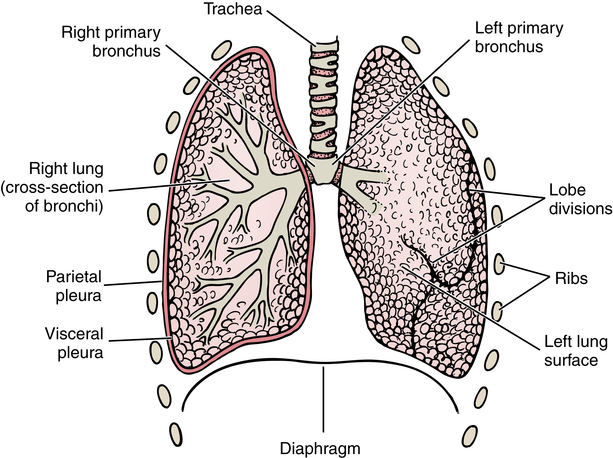
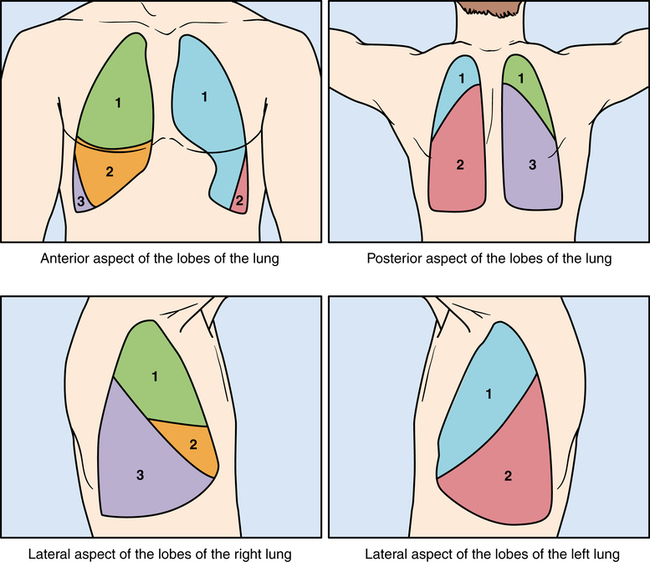
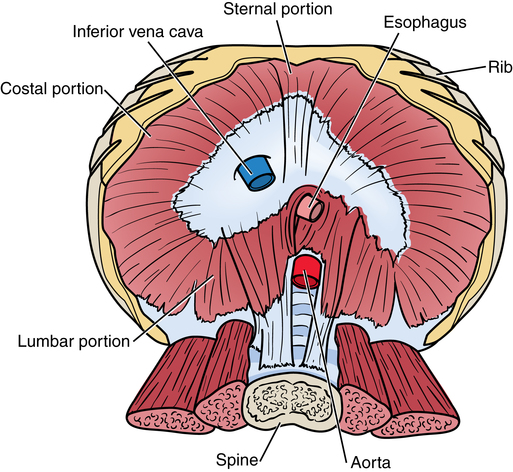
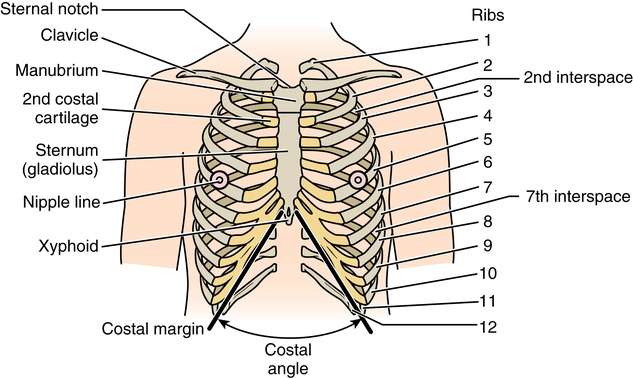
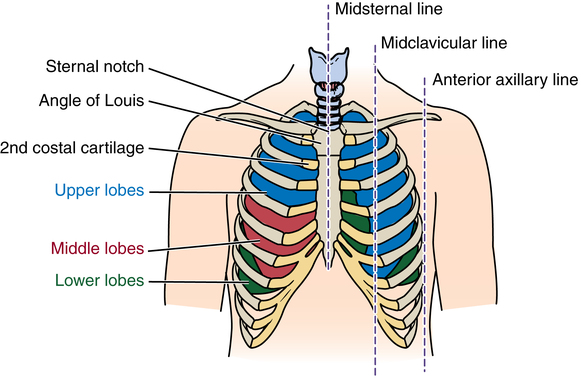
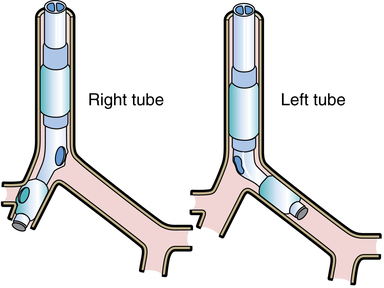
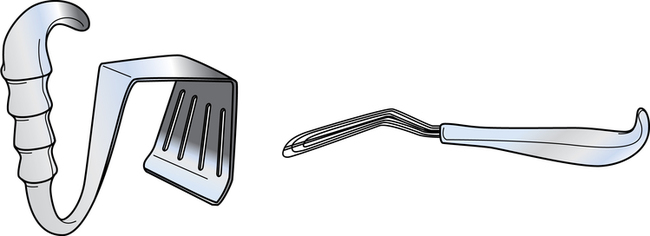
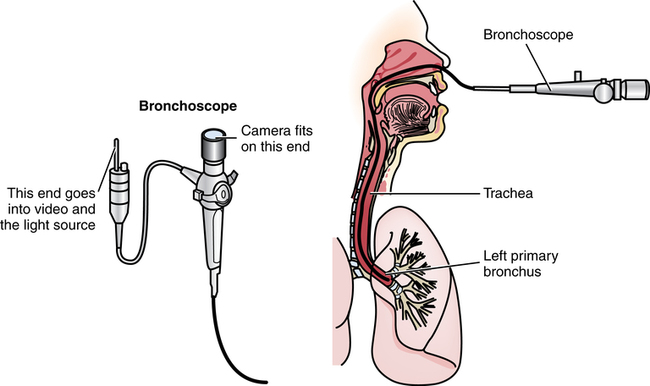
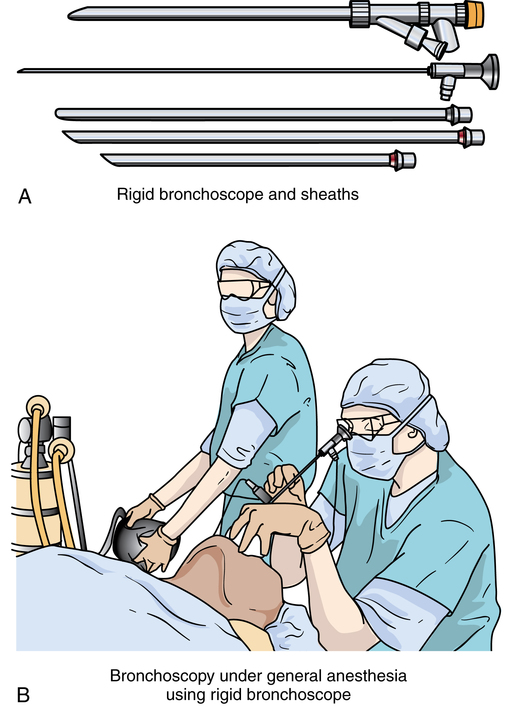
Chapter 42 After studying this chapter, the learner will be able to: • Identify the pertinent anatomy of the thoracic cavity. • Describe patient positioning for each type of thoracic incision. An essential balance must be maintained between atmospheric pressure outside the chest and internal pressures within the thoracic cavity to sustain the vital function of respiration. Knowledge of the anatomy and physiology of the chest and thoracic cavity is necessary for an understanding of thoracic surgery. The first seven ribs articulate anteriorly in the midline with the sternum, which is composed of three parts: the manubrium (superiorly), the gladiolus (medially), and the xiphoid process (inferiorly). Ribs one and two articulate with the clavicle and the manubrium. The manubrium and gladiolus join in a projection referred to as the angle of Lewis, a surgical landmark (Fig. 42-1). Ribs three through seven articulate with the gladiolus (the main sternal body) via the costal cartilage. The eighth, ninth, and tenth ribs are joined anteriorly to the cartilage of the rib above each; the eleventh and twelfth ribs have no anterior fixation. The surgical incisional lines of direction in Figure 42-2 bilaterally overlie the lobes of the lungs on a vertical axis, with the sternum (gladiolus) as the thoracic reference point. The lungs lie in the right and left pleural cavities (Fig. 42-3). The main function of these porous, spongy, conical organs is oxygenation of the blood with inspired air and expiration of carbon dioxide. The apex of each extends to the neck; the base rests on the superior surface of the diaphragm. The trachea divides at the carina into two main branches—the bronchi—leading to the right and left lungs. The right lung, with three lobes, is wider and broader than the left lung because the liver is positioned beneath the diaphragm directly below the base. The left lung has only two lobes and is thinner, longer, and narrower in shape. It shares space in the left side of the chest with the heart, which rests in an area of the left lung referred to as the cardiac notch (Fig. 42-4). The diaphragm is a half dome of muscular tissue composed of four embryonic segments: (1) dorsal mesentery, (2) septum transversum, (3) two pleuroperitoneal folds, and (4) cervical myotomes that border the inferior aspect of the thoracic cavity. It originates from the six lower ribs on each side and attaches to the xiphoid and the external and internal arcuate ligaments. Abnormal separation of any of these layers changes the pressure gradient between the peritoneal cavity and the thorax, causing a shift of intraabdominal organs cephalad into the chest.7 The esophagus, aorta, and vena cava pass from the thorax through the diaphragm into the abdominal cavity via three separate openings. Associated vessels and nerves, such as the vagus nerve, follow these three structures through the diaphragm to major organ systems (Fig. 42-5). Alterations of intrapleural pressure are of major concern because an uncontrolled opening in the thoracic wall and pressure change can be fatal.7 Uncontrolled increased positive pressure in one side causes a collapse of the lung on the other side. Referred to as a mediastinal shift, this reaction occurs with entrance of either air or fluid into the pleural cavity, compressing the opposite lung and causing dyspnea. When the mediastinum has moved its limit, it can no longer accommodate a great pressure change; the lung on the affected side collapses. Air in the pleural space between the parietal and visceral pleurae constitutes pneumothorax. Blood in the pleural space constitutes hemothorax. 1. Endotracheal anesthesia permits the lungs to expand and function even when subjected to atmospheric pressure. Administration of anesthesia under controlled positive pressure prevents physiologic imbalance and lung collapse in the presence of controlled pneumothorax. Use of a double-lumen endotracheal tube permits expansion of the unaffected lung and collapse of the lung on the surgical side (Fig. 42-6). At the conclusion of the surgical procedure, the affected lung is reexpanded by the anesthesia provider, and negative pressure in the chest is restored. Portable chest x-rays may be taken immediately to assess the status of the surgical area, pleural cavities, and lung reexpansion. 2. Instrumentation includes a basic laparotomy setup with the addition of thoracic instruments. These include bone instruments and a power saw (Fig. 42-7 shows rib strippers/rasps, shears, and an approximator/contractor); a large self-retaining chest retractor/rib spreader (Fig. 42-8); bronchus clamps and lung forceps (Fig. 42-9); and long instruments for work in a deep incision. Specialty retractors are used to hold lung tissue and displace the bones of the shoulder girdle (Fig. 42-10). 3. A variety of sutures may be used for soft tissues, vessels, and bone. The bronchus usually is closed with staples. 4. Sponges for hemostasis or blunt dissection are placed on long ring-handled forceps. Periosteal bleeding may be controlled by electrocoagulation. Bone wax may be needed to control bone marrow oozing. 5. Blood for transfusion should be available at all times. Hemorrhage is a major threat intraoperatively and postoperatively. Blood may be salvaged for autotransfusion by cell saver, and a postoperative drainage salvage reservoir and autotransfusion drain may be used. 6. The surgical field is potentially contaminated by secretions and contact with open air passages when a bronchus is opened and sutured. Used items and instruments are isolated in a discard basin. Maintenance of a dry field is important to prevent aspiration of blood and fluid, which predisposes the patient to postoperative pneumonia. 7. An airtight pleural cavity must be restored and negative pressure maintained for maximum pulmonary function postoperatively. Except after a few specific procedures, a sterile closed water-seal drainage system is essential. Chest tubes are inserted through a stab wound and anchored to the chest wall with suture and tape. Two or three tubes are sometimes inserted into the pleural space and connected to separate drainage systems (Fig. 42-11). The tube at the base of the pleural space is usually inserted at the seventh costal interspace, near the anterior axillary line, to evacuate fluid. An upper tube, if indicated, is inserted at the apex through the anterior chest wall at the third costal interspace to evacuate air leaking from the lung. Key points to remember include the following: a. Connections must be physically tight and securely taped at the time of dressing application. The taped connections should not obscure the observation of drainage. b. System components must be kept below the level of the patient’s body to prevent reentry of air or fluid from the drainage collection system into the pleural cavity. c. Tubes may be clamped before insertion and connection to the drainage system, depending on the surgeon’s preference. Tubes are not routinely clamped at other times unless this is specifically requested by the surgeon. Surgeon preference and the procedure determine the method of entrance into the thorax. Access may be gained by an anterior, lateral, or posterior approach, or a combination of these. Entrance through the ribcage may be intercostal between the ribs, through the periosteal bed of an unresected rib, or by rib resection. By incising near the top of a rib, the surgeon protects nerves and vessels that lie in the intercostal spaces. An intercostal approach may be used to drain an empyema pocket or mediastinal abscess or to obtain a biopsy specimen of lymph nodes or of a lung.6 • Diagnosis: Securing an uncontaminated secretion for culture, obtaining a biopsy specimen, or finding the cause of a cough or hemoptysis • Intervention: Removing a foreign body, excising a small tumor, applying medication, aspirating the bronchi, or providing an airway during performance of a tracheotomy Flexible bronchoscopy is used frequently for the patient with decreased range of neck motion. Flexible bronchoscopy can be performed via the nasopharynx or orally to the trachea and into the bronchial tree (Fig. 42-12). If the gag reflex can be controlled, oral rigid bronchoscopy can be performed with the patient under local anesthesia and intravenous sedation. General anesthesia may be necessary. The bronchoscope is inserted over the tongue and through the vocal cords to the trachea. The patient’s head is turned to the right to visualize the left bronchus and to the left for the right bronchus (Fig. 42-13).
Thoracic surgery
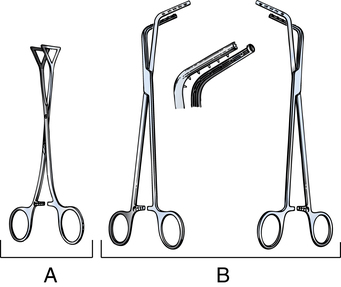
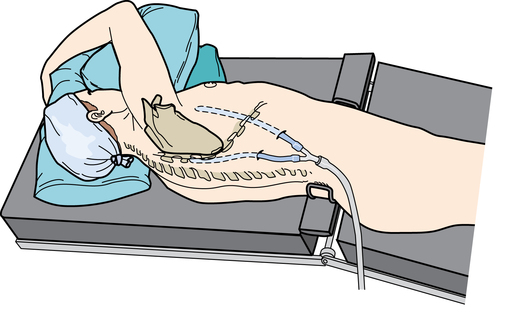
Anatomy and physiology of the thorax
Thoracic cavity
Lungs
Diaphragm
Physiology
Special features of thoracic surgery
Access to the thorax
Bronchoscopy
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic surgery

 Website
Website