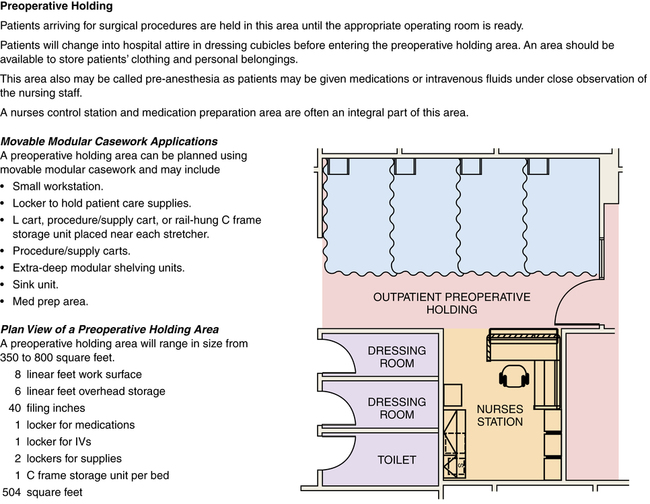
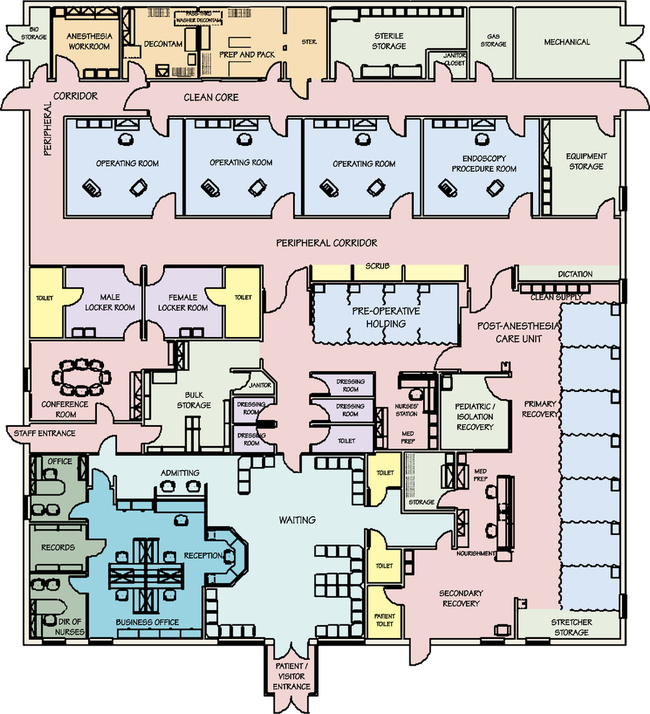
Chapter 11 After studying this chapter, the learner will be able to: • Compare the differences between hospital-based services and ambulatory surgery centers (ASCs). • Distinguish between activities in fixed and mobile surgery locations. Ambulatory surgery can be defined as surgical patient care performed with general, regional, or local anesthesia without overnight hospitalization. Some ASCs offer diagnostic testing and radiologic examinations, such as mammography. The following are organizations specifically for professional ambulatory surgical nurses: • American Society of PeriAnesthesia Nurses (ASPAN); www.aspan.org • American Academy of Ambulatory Care Nurses (AAACN); www.aaacn.org • Association of periOperative Registered Nurses (AORN); www.aorn.org AORN has established a specialty assembly for nurses who practice in the ambulatory setting. A chairperson and council are selected by the assembly membership to serve 3-year terms. AORN’s website has an ambulatory practice portal at www.aorn.org. • Preprocedural testing and assessment area (PAT center) • Changing and dressing room with lockers and toilets • Preoperative holding/preparation area • Postanesthesia care unit (PACU) or access to a PACU The decor of the ambulatory facility should be pleasing to enhance relaxation of the patient and family. Recliners are commonly available for postprocedure recovery. Many facilities have televisions with videocassette capability. Figure 11-1 depicts a sample floor plan that shows the various areas within an ASC. Priority patient parking areas should be conveniently located near the entrance to the facility, with parking spaces for disabled patients located nearest the entrance. • Hospital-based dedicated unit. Patients come to a self-contained unit that is located within or attached to the hospital but physically separate from the inpatient OR suite. • Hospital-based integrated unit. Ambulatory patients share the same OR suite and other hospital facilities with inpatients. The preoperative admission and holding area is shared. Ambulatory patients usually return to the same admission area for discharge after the procedure. • Office-based center. Patients come to a physician’s office that is equipped for surgery. Many private surgeons, dermatologists, periodontists, and podiatrists perform surgical procedures in their offices with a local anesthetic. This office-based center may accommodate one or more surgeons in the same specialty, or it may be a multiphysician, interdisciplinary clinic. Although these are not always attached to a hospital, they are not considered an ASC by FASA. Examples of ambulatory surgery centers by the definition of FASA are the following: • Hospital-affiliated satellite surgery center. Patients come to an ambulatory surgery center that is owned and operated by a larger facility but geographically separate from it. • Freestanding ambulatory surgery center. Patients come to a completely independent facility. Many of these facilities are owned and operated by physicians. The ASC should comply with standards set by the Accreditation Association for Ambulatory Health Care (AAAHC; www.aaahc.org), The Joint Commission (TJC; www.thejointcommission.org), the American Association for the Accreditation of Ambulatory Surgery Facilities (AAAASF; www.aaaasf.org), the Ambulatory Surgery Center Association (www.ascassociation.org), and the American Osteopathic Association (AOA; www.osteopathic.org). These five patient advocacy and consumer groups advise patients to select facilities carefully and to look for accreditation and credentialing by professional and governmental agencies. The 2011 updates for Ambulatory Care and Office-Based Surgery National Patient Safety Goalsa include the following: • Improve the accuracy of patient identification: Use a minimum of two patient identifiers (excluding the patient’s room number) when administering pharmacologic agents or blood, taking blood samples or specimens, or providing any treatments or procedures. • Improve communications among caregivers: All verbal orders or results should be read back to the person delivering the information. Standardize a list of all abbreviations, acronyms, and symbols that are not to be used within the organization. Improve the timeliness of information exchange between the reporter and receiver regarding test results and values. Standardize the hand-off report of patient care to qualified personnel between phases of care. • Improve medication safety: Standardize the numbers and concentrations of drugs within the facility, identify sound-alike/look-alike medications and limit their use to prevent error, and label all containers and delivery devices with the name and concentration of the drug. Discard any unlabeled medication containers. • Reduce the risk of health care–related infections: Comply with Centers for Disease Control and Prevention (CDC) recommendations for hand hygiene. All deaths or permanent injuries associated with health care–related infection are treated as sentinel events. • Identify and reconcile patient medications across the continuum of care: All home and hospital medications are identified and relayed to all caregivers in the hand-off report. • Reduce the risk of surgical fires: Staff education should include spark, fuel, and ignition sources, including oxygen concentration under drapes, as a source of surgical fire. • Compliance with structural standards • Establishment of policies and procedures that support competent standards of care • Appropriate credentialing of personnel Some facilities are prohibited from performing complicated laparoscopy because of the risk for injury to the patient. (More information can be found at the Federated Ambulatory Surgery Association website at www.fasa.org.) 1. General health status. Acceptable patients are in class I, II, or stable III of the physical status classification of the ASA. Patients are evaluated physically and emotionally to determine the possibility of complications during or after the surgical procedure. The Centers for Medicare and Medicaid Services (CMS) December 2010 ruleb requires three separate health assessments before a patient is placed on the OR bed. The three assessments include: a. A complete medical history and physical examination (H&P) no earlier than 30 days before the intended surgical procedure. The H&P must be redone if 30 days have passed. b. A physical assessment on arrival at the surgery center to validate that no changes have occurred since the H&P was performed. Care is taken when discussing private information in the ASC cubicles. Other patients can overhear conversation through the divider curtains. c. A preanesthesia evaluation to assess the safety of administration of anesthesia before the patient enters the OR. 2. Results of preoperative tests.4 Patients may have tests on admission the morning of the surgical procedure, but preferably these tests are performed before the scheduled surgery date so the results can be evaluated. This prevents cancellation on the day of surgery if test results are unsatisfactory. Test results are placed on the chart that accompanies the patient to the OR. Preoperative tests may include the following: a. Complete blood count (CBC) and urinalysis (usually included in basic laboratory tests) b. Pregnancy test, unless patient previously had a hysterectomy or oophorectomy c. Multichemistry profile for patients at higher risk d. Chest x-ray (may be required if clinically indicated) e. Electrocardiogram (ECG; may be required before general anesthesia for patients older than 35 years) 3. Willingness and psychological acceptance by patient and family. The patient should be willing and able to recuperate at home. Some patients lack adequate home care and may need other arrangements. • Recovery period: The surgeon should anticipate minimal or no postoperative complications. Patients in whom a prolonged period of nausea and vomiting is anticipated or in whom pain will not be relieved with oral analgesics are not ideal candidates for ambulatory surgery. • Reimbursement sources: Most third-party payers prefer less costly ambulatory surgery whenever a procedure can be safely performed in this setting. Patient safety and quality of care depend on patient screening and support systems. a. Make an appointment for preadmission assessment and testing. b. Take nothing by mouth (NPO) after midnight (or other specified hour) before admission unless ordered to do so by the surgeon. This includes medications, unless ordered. c. Perform any necessary physical preparation such as bathing with antimicrobial soap as ordered. d. Arrive at the facility by ____ am/pm. (Time depends on the scheduled time for the surgical procedure. A minimal wait at the facility helps to reduce preoperative anxiety. Patients are usually admitted at least 1 hour before the scheduled time of their surgical procedure. Figure 11-2 shows an ambulatory preoperative holding area.) e. Notify the surgeon immediately of a change in physical condition, such as a cold or fever. f. Wear loose and comfortable clothing, leave jewelry (including tongue and body piercings) and valuables at home, and remove makeup and nail polish. (This may include the removal of acrylic fingernails for some procedures if affixing the pulse oximeter to another location, such as the toe, is not an option.) a. Arrange for a responsible adult support person to take you home. (After some procedures, the patient may not be permitted to drive or leave unattended.) b. Do not ingest alcoholic beverages, drive a car, cook, or operate machinery for 24 hours if a sedative or general anesthetic has been administered. c. Delay important decision making until full recovery is attained. d. Take medications only as prescribed and maintain as regular a diet as tolerated. e. Shower or bathe daily unless instructed otherwise. This helps to relieve muscle tension and discomfort and keeps the wound clean. f. Call the surgeon if postoperative problems arise. g. Report to the nearest emergency department if your condition deteriorates.
Ambulatory surgery centers and alternative surgical locations
Ambulatory surgical setting
Ambulatory surgery programs
Accreditation of ambulatory facilities
Patient selection for ambulatory surgery
Preoperative patient care
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Ambulatory surgery centers and alternative surgical locations

 Website
Website