Part 3 The lower limb
Introduction
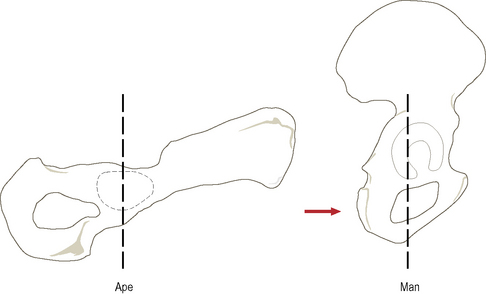
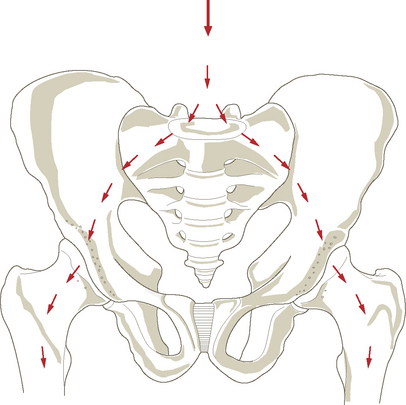
The pelvic girdle, formed by the right and left innominate articulating anteriorly at the symphysis pubis and posteriorly by the sacrum via the sacroiliac joint, connects the lower limb to the vertebral column. The sacroiliac joint provides great strength for weight transference from the trunk to the lower limb at the sacrifice of almost all mobility. The human ilium has developed so that it is no longer blade-like but is shortened and tightly curved backwards and outwards (Fig. 3.1), changing the actions of the gluteal muscles. These changes in the pelvis have resulted in a shift from it lying in an essentially horizontal to an essentially vertical position. This has enabled the trunk to be held vertically, but has necessitated a change in the orientation of the sacrum with respect to the ilium: the result is that the axis of the pelvic canal lies almost at right angles to the vertebral column. During evolution there has been a relative approximation of the sacral articular surface to the acetabulum which makes for greater stability in the transmission of the weight of the trunk to the hip joint. This increase in the magnitude has resulted in an increase in the contact area between sacrum and ilium relative to the area of the ilium as a whole. For the same reason the acetabulum and femoral head have also increased in relative size during evolution. The shortening of the ischium that has occurred is an adaptation for speed and rapid movements, which is of great importance in bipeds. Thus power of action has been sacrificed for speed.
It is the foot, however, which has undergone the greatest change during evolution (Fig. 3.2), reflecting not so much the evolution of a new function as a reduction in the original primate functions, with the foot changing from a grasping, tactile organ to a locomotor prop. Although some non-locomotor function is still possible, the foot has evolved from a generalized to a specialized organ. The joints of the human foot permit much less internal mobility – an adaptation to ground walking. In locomotion, the foot acts as a lever adding propulsive force to that of the leg, with the point of pivot being the subtalar joint. The forefoot has been shortened relative to the hindfoot, where the main thrust in walking is developed – the power capabilities are thus accentuated.
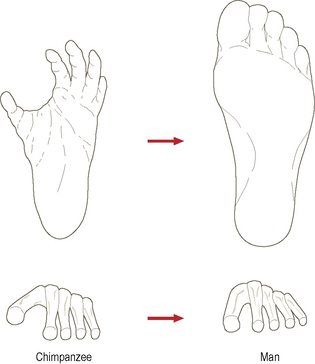
Figure 3.2 The evolutionary changes that have occurred within the foot during its adaptation to bipedalism.
An important consequence of the upright, bipedal posture is that the centre of gravity of the body has been brought towards the vertebral column, so that in humans it lies slightly behind and at about the same level as the hip joint, thus reducing the tendency of gravity to pull the trunk forward. The centre of gravity projection then passes anterior to the knee and ankle joints (see Fig. 3.4); at the knee the line of weight transmission passes towards the outside. Because of the angulation of the femur, during walking the foot, tibia and knee joint of each leg stay close to the line followed by the centre of gravity, and thus energy expenditure is minimal in maintaining the centre of gravity above the supporting limb. Balance is thus improved and there is more time for the free leg to swing forward promoting an increase in stride length. The alteration in the line of weight transmission is carried into the foot, where it passes to the inner side. However, it must be remembered that weight is also transmitted through the outside of the foot, bringing the entire foot into use as a stabilizing element.
Development of the musculoskeletal system
Mesodermal somites
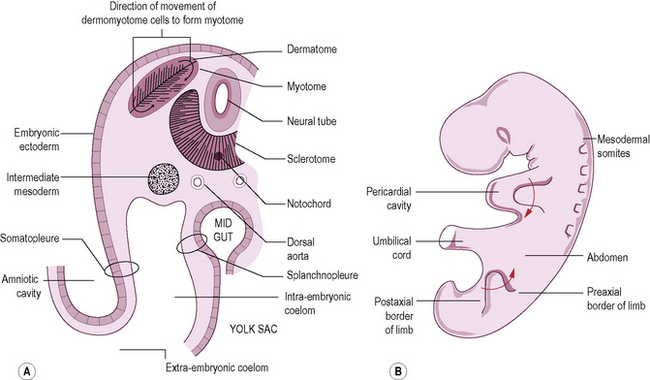
By the end of the third week after fertilization the paraxial mesoderm begins to divide into mesodermal somites which are easily recognizable during the fourth and fifth weeks (Fig. 3.3B). Eventually some 44 pairs of somites develop, although not all are present at the same time; however, the paraxial mesoderm at the cranial end of the embryo remains unsegmented. There are 4 occipital somites, followed by 8 cervical, 12 thoracic, 5 lumbar, 5 sacral and 8–10 coccygeal somites. The growth and migration of these somitic cells are responsible for the thickening of the body wall, as well as the development of bone and muscle. The deeper layers of the skin are also of somitic origin. Somite-derived tissue spreads medially to form the vertebrae, dorsally to form the musculature of the back, and ventrally into the body wall to form the ribs, and the intercostal and abdominal muscles.
Soon after its formation each somite becomes differentiated into three parts. The ventromedial part forms the sclerotome, which migrates medially towards the notochord and neural tube to take part in the formation of the vertebrae and ribs (Fig. 3.3A). The remainder of the somite is known as the dermomyotome. The cells of the dorsal and ventral edges proliferate and move medially to form the myotome, whose cells migrate widely and become differentiated into myoblasts (primitive muscle cells). The remaining thin layer of cells forms the dermatome, which spreads out to form the dermis of the skin.
Development of the limbs
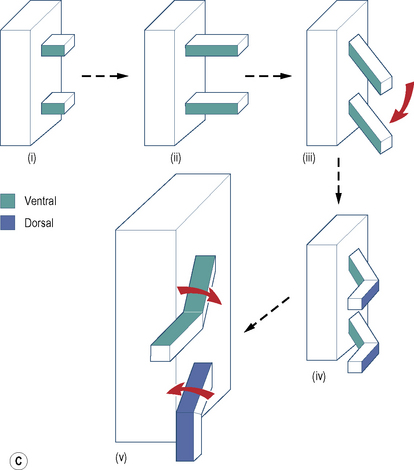
The limbs initially appear as flipper-like projections (the limb buds), with the forelimbs appearing first, between 24 and 26 days, each bud consisting of a mass of mesenchyme covered by ectoderm with a thickened ectodermal ridge at the tip; the ectodermal ridge controls normal development of the limb. Consequently, damage to it will result in some trauma to the limb. At the beginning of the second month the elbow and knee prominences project laterally and backwards. At about the same time, the hand and foot plates appear as flattened expansions at the end of the limb bud. Between 36 and 38 days, five radiating thickenings forming the fingers and toes can be distinguished; the webs between the thickenings disappear freeing the digits. Appropriate spinal nerves grow into the limbs in association with migration of the myotomes: C5, 6, 7, 8 and T1 for the upper limb, and L4, 5, S1, 2 and 3 for the lower limb. The limb bones differentiate from the mesenchyme of the bud. The limbs grow in such a way that they rotate in opposite directions, the upper limb laterally and the lower limb medially (Fig. 3.3C). Consequently, the thumb becomes the lateral digit of the hand while the great toe is the medial digit of the foot.
During development the lower limb bud appears as a swelling from the body wall (Fig. 3.3C(i)); the lower limb follows the upper limb in appearance and development. At first, each limb bud projects at right angles to the surface of the body, having ventral and dorsal surfaces, and cephalic (preaxial) and caudal (postaxial) borders (Fig. 3.3C(ii)). As the limb increases in length it becomes differentiated, during which time it is folded ventrally so that the ventral surface becomes medial (Fig. 3.3C(iii)), with the convexities of the elbow and knee directed laterally (Fig. 3.3C(iv)). At a later stage, the upper and lower limbs rotate in opposite directions such that the convexity of the knee is directed towards the cranial end of the body (Fig. 3.3C(v)). The ventral rami entering a limb bud pass anterior to the myotomes and eventually divide into dorsal and ventral divisions, which unite with the corresponding branches of the adjacent ventral rami to form the nerves of the dorsal and ventral aspects of the limb bud. These nerves will supply respectively the sheets of muscle and overlying skin of the dorsal (extensor) and ventral (flexor) surfaces of the limbs prior to their rotation into the adult pattern. During the folding and rotation of the limb and the migration of muscle masses, these nerve–muscle connections are maintained.
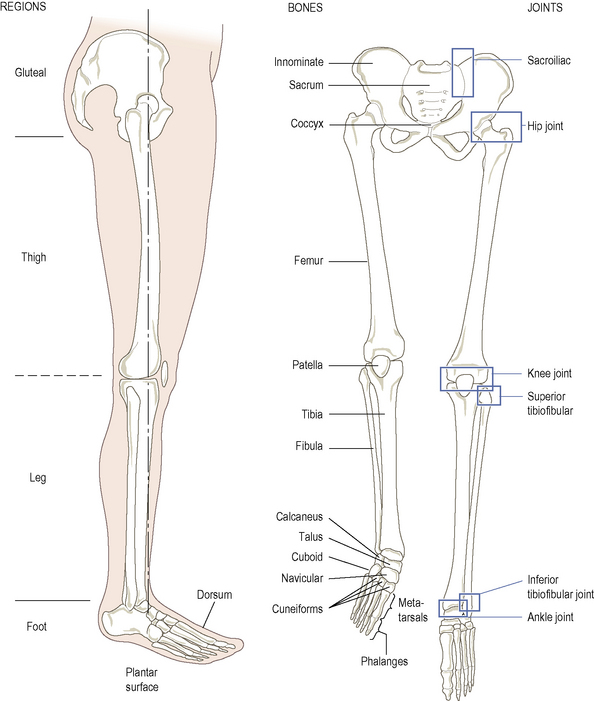
The uppermost limit of the lower limb is a line joining the iliac crest, inguinal ligament, symphysis pubis, ischiopubic ramus, ischial tuberosity, sacrotuberous ligament, and the dorsum of the sacrum and coccyx. The bulge of tissue running between the innominate and the upper part of the femur forms the buttock, but the region is usually named gluteal after the underlying muscles. The lower limb is divided into the thigh between the hip and knee, the leg between the knee and ankle, and the foot distal to the ankle joint. The foot is divided into the foot proper and the toes, and has a superior surface (dorsum) and an inferior (plantar) surface, which is the sole of the foot (Fig. 3.4).
The bones of the lower limb are those of the pelvic girdle (innominate and sacrum), the femur in the thigh, the medial tibia and lateral fibula in the leg, the seven tarsal bones and five metatarsals in the foot, and the phalanges of the toes – two in the big toe and three in each remaining toe (Fig. 3.4).
Bones
Pelvic girdle
Introduction
The pelvic girdle (Fig. 3.5) comprises the two innominates and sacrum; the ring of bone formed uniting the trunk and the lower limbs. A large, irregular bone, the innominate consists of two expanded triangular blades twisted 90° to each other in the region of the acetabulum; each blade is also twisted within itself. The innominate is formed from three separate bones, the ilium, ischium and pubis, which come together and fuse in the region of the acetabulum such that in the adult it appears as a single bone. The sacrum consists of five fused vertebrae and is roughly triangular. The coccyx, which is the remnant of the tail, consists of four fused coccygeal vertebrae. Each innominate articulates with the sacrum posteriorly by joints which are synovial anteriorly and fibrous posteriorly. Each innominate also articulates with its counterpart anteriorly at the pubic symphysis, by a secondary cartilaginous joint.
The pelvic girdle has several functions:
The pelvic girdle transmits the weight from the vertebral column to the lower limbs (Fig. 3.5), its bony and ligamentous components reflecting this function. There are some differences in the pelvis between females and males. In the female, these are due to adaptation for childbearing and the transmission of the relatively large fetal head during childbirth. The pelvis is essentially a basin, the upper part being known as the greater or false pelvis containing abdominal viscera. That part below the pelvic brim or pelvic inlet is the lesser or true pelvis. In the anatomical position, the pelvic inlet forms an angle of about 60° with the horizontal (Fig. 3.6). The acetabulum is directed laterally and inferiorly with the acetabular notch directed inferiorly. The anterior superior iliac spines and the pubic tubercles lie in the same vertical frontal plane. The lowest part of the sacrum lies above the level of the symphysis pubis.
The innominate (hip) bone
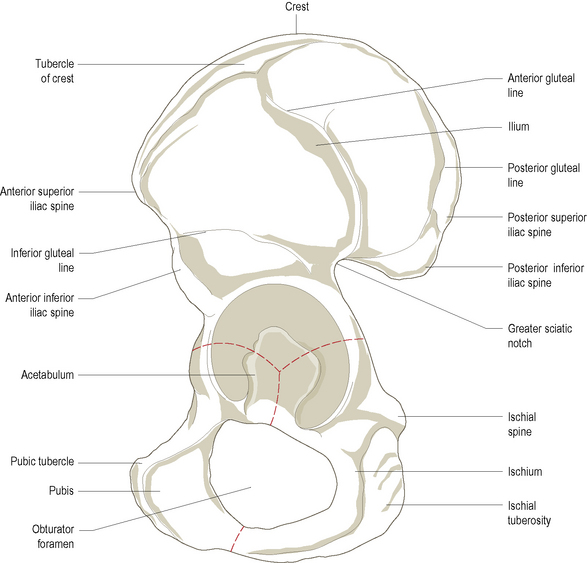
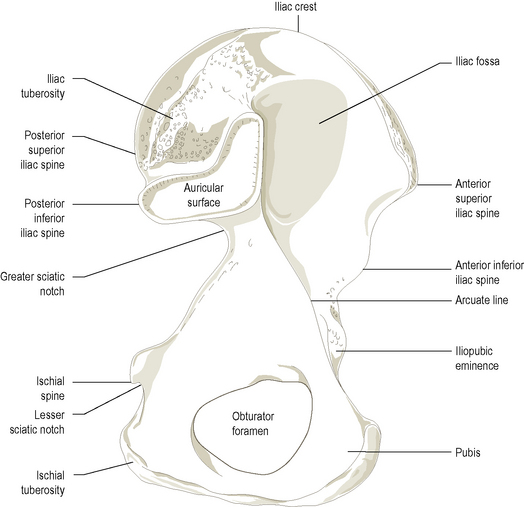
An irregularly shaped bone (Figs. 3.7 and 3.8) consisting of three bones fused together, the ilium, the pubis and the ischium.
The ilium
The upper broad blade for the attachment of ligaments and large muscles. It forms the pelvic brim between the hip joint and the articulation with the sacrum. The anterior two-thirds forms the iliac fossa medially, which is part of the lateral and posterior abdominal wall, and the gluteal surface laterally, for attachment of the gluteal muscles. The posterior one-third of the medial surface, which is thicker, carries the auricular surface for the articulation with the sacrum; behind this is a prolonged rough part, the iliac tuberosity, for the attachment of the strong sacroiliac ligaments which bear the body weight. The upper border is the iliac crest, which is convex superiorly as well as anteroposteriorly with the anterior part curved outwards. The iliac crest ends as the anterior superior iliac spine anteriorly and the posterior superior iliac spine posteriorly. Both spines and the whole of the crest can be palpated (p. 211). Behind the anterior spine on the outer border is the prominent tubercle of the crest. Below the anterior superior spine the anterior inferior iliac spine is separated by a shallow notch. Similarly, below the posterior superior spine the posterior inferior iliac spine is separated by a shallow notch; the two posterior spines are closer together than the two anterior spines. Below the posterior inferior spine is the deep greater sciatic notch. The iliac fossa is separated from the sacropelvic surface of the ilium by the arcuate line, which forms part of the pelvic brim. The anterior part of this line has an elevation, the iliopubic eminence, marking the junction of the ilium with the pubis. The part which participates in the formation of the acetabulum is the body of the ilium.
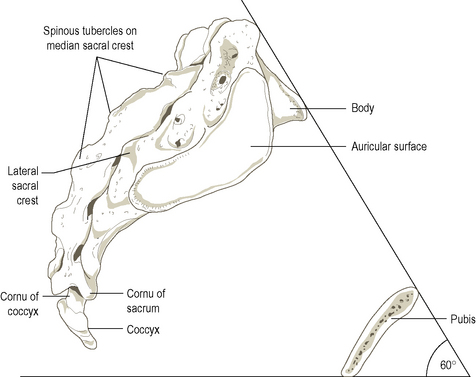
The sacrum
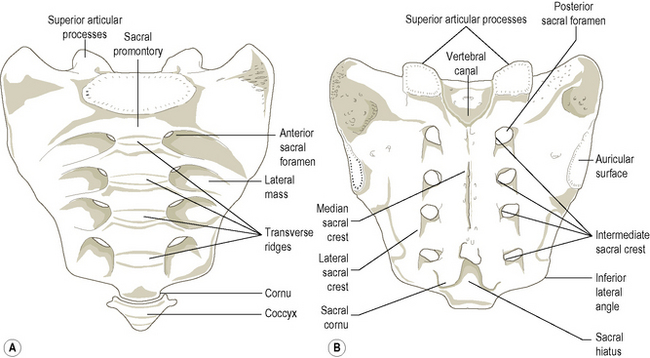
A triangular bone with the apex inferior, it consists of five fused vertebrae broadened by the incorporation of large costal elements and transverse processes into heavy lateral masses, which lie lateral to the transverse tubercles on the back of the sacrum extending between the anterior sacral foramina onto the front of the bone; the auricular surface lies entirely on the lateral mass. It is wedged between the posterior parts of the two innominates with which it articulates at the sacroiliac joints. The pelvic (anterior) surface (Fig. 3.9A) is concave and relatively smooth, being marked by four transverse ridges separating the original bodies of the five sacral vertebrae. Lateral to each ridge is the anterior sacral foramen, representing the anterior part of the intervertebral foramen; the foramina are directed laterally and anteriorly.
The dorsal surface (Fig. 3.9B) is convex and highly irregular with posterior sacral foramina, medial to which the vertebral canal is closed over by the fused laminae. However, the spinous processes and laminae of the fourth and fifth sacral vertebrae are usually absent, leaving the vertebral canal open. This is the sacral hiatus, an inferior entrance to the vertebral canal, which may be used, for example during labour, to introduce an anaesthetic agent to block the sacral nerves. Posteriorly, in the midline, the reduced spinous processes form the median sacral crest. Lateral to the posterior sacral foramina are the prominent lateral sacral crests, representing the transverse processes, which provide attachment for the dorsal sacroiliac ligaments, and inferiorly for the sacrotuberous and sacrospinous ligaments. Medial to the posterior sacral foramina are the indistinct intermediate sacral crests, representing the fused articular processes. The superior articular processes of the first sacral vertebra are large and oval, being supported by short heavy pedicles. Their facets, for articulation with the inferior articular surfaces of the fifth lumbar vertebra, are concave from side to side and face posteromedially. The tubercles of the inferior articular processes of the fifth sacral vertebra form the sacral cornua and are connected to the cornua of the coccyx.
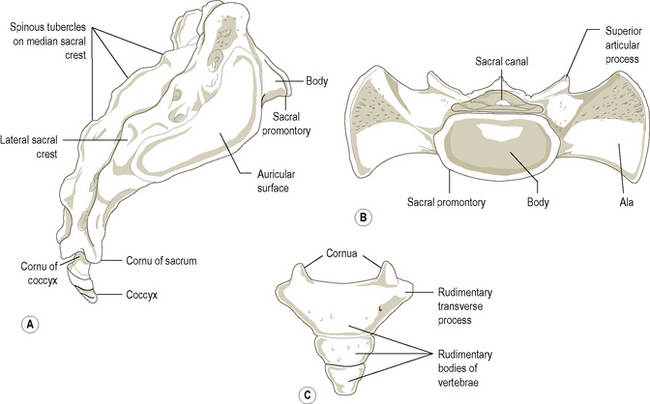
The lateral surface (Fig. 3.10A) is triangular, being narrower below. The upper part is divided into an anterior smoother pitted auricular surface, covered in cartilage, for articulation with a similar area on the ilium. The rougher posterior area has three deep impressions for attachment of the powerful posterior sacroiliac ligaments. The superior surface (Fig. 3.10B) faces anterosuperiorly and has a central oval area which is the upper surface of the first sacral vertebra; it is separated from the fifth lumbar vertebra by a thick intervertebral disc. Its anterior projecting border is the sacral promontory. On each side of the body of the sacrum is the ala, formed by the fusion of the costal and transverse processes of the first sacral vertebra. When articulated with the innominate, the ala of the sacrum is continuous with the ala of the ilium.
The coccyx
It usually consists of four fused vertebrae forming a single piece or two pieces of bone (Fig. 3.10C), which mainly represent the bodies. The pelvic surface is concave and relatively smooth, while on the posterior surface the rudimentary articular processes are present as a row of tubercles. Superiorly the larger pair form the coccygeal cornua which articulate with the sacral cornua, and enclose the fifth sacral intervertebral foramen. The posterior wall of the vertebral canal of the coccyx is absent so that the sacral hiatus continues downwards over the back of the coccyx.
The femur
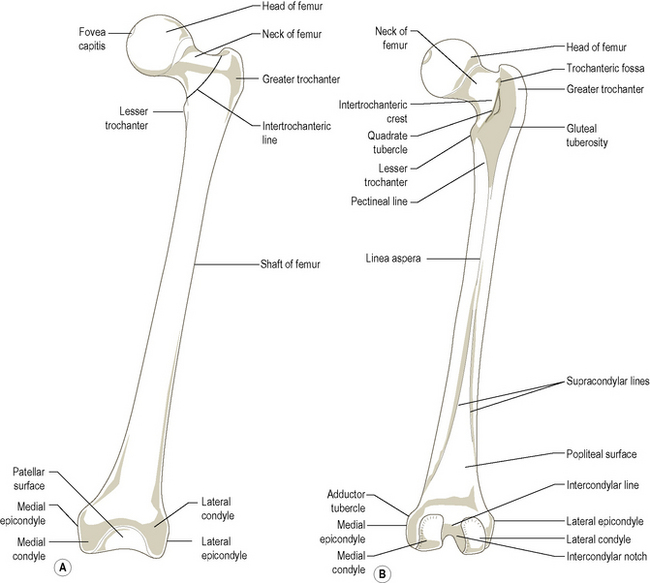
The longest and strongest bone in the body (Fig. 3.11), it transmits body weight from the ilium to the upper end of the tibia. It has a shaft and two extremities.
Ossification
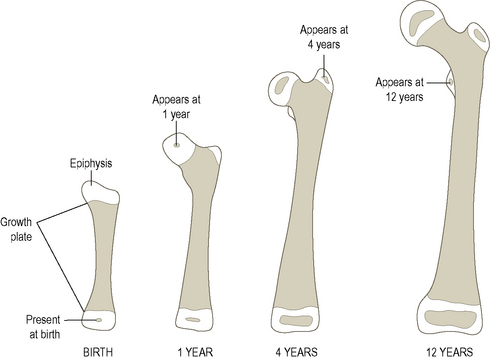
The primary ossification centre for the shaft appears at 7 weeks in utero. At birth, growth plates separate the bony shaft from the upper and lower cartilaginous epiphyses (Fig. 3.12). A secondary ossification centre appears in the lower epiphysis shortly before birth. Secondary ossification centres appear in the upper epiphysis for the head at 1 year and in the greater trochanter at 4 years (Fig. 3.12). The last secondary ossification centre appears in the cartilaginous lesser trochanter at 12 years. The upper epiphysis fuses with the shaft at about the 18th year, the last to do so being the head. The lower epiphysis fuses with the shaft at about 20 years. The neck of the femur is ossified as part of the body (shaft) and not from the upper epiphysis.
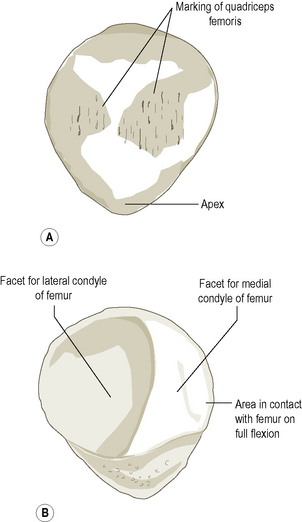
The patella
A triangular sesamoid bone (Fig. 3.13) formed in the tendon of quadriceps femoris, with its apex pointing inferiorly and its base uppermost. It is flattened from front to back, having anterior and posterior surfaces and superior, lateral and medial borders.
The tibia
A long bone (Fig. 3.14), which transmits body weight from the medial and lateral condyles of the femur to the foot. It is the larger of the two bones of the leg, being situated medial to the fibula. It consists of a shaft and two extremities, the upper extremity being much larger than the lower.
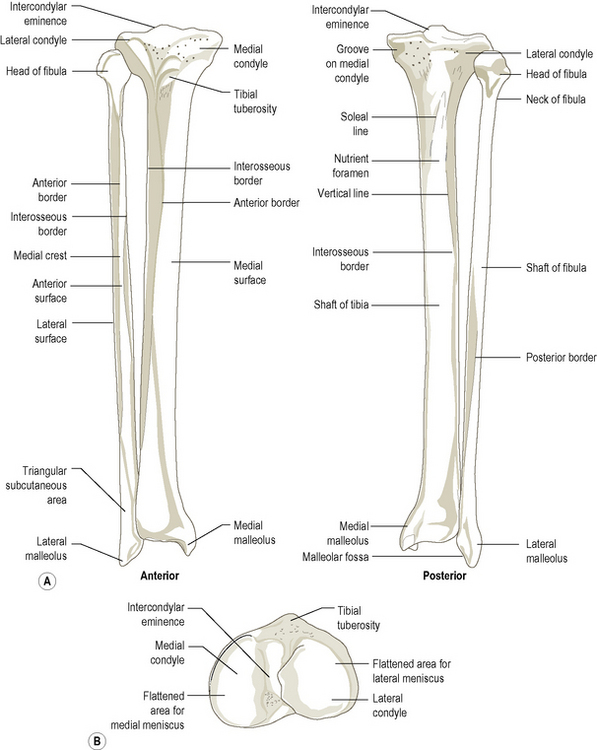
Figure 3.14 (A) Right tibia and fibula, anterior view and posterior view, (B) right tibia, superior view.