Squamous Cell Carcinoma, General Concepts
Antonio L. Cubilla, MD
Alcides Chaux, MD
Elsa F. Velazquez, MD
TERMINOLOGY
Abbreviations
Squamous cell carcinoma (SCC)
Definitions
Malignant epithelial neoplasia showing keratinocytic differentiation
ANATOMY AND HISTOLOGY
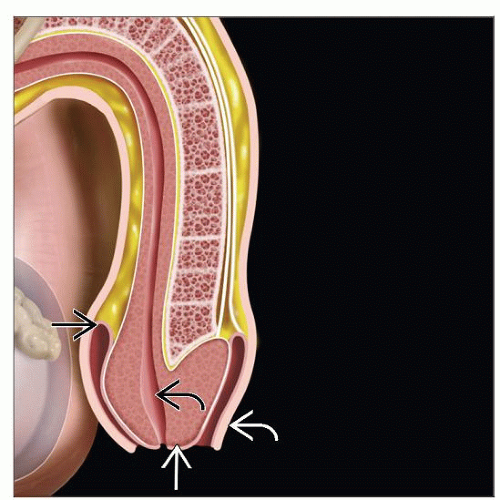
Anatomical Considerations
Penile anatomical regions are glans, foreskin, and shaft
Glans is distal, most cone-shaped region, formed by corpus spongiosum (CS) covered by squamous mucosa
Distal urethra opens up into meatus, a ventrally located slit-like orifice in glans
Glans corona separates glans from coronal sulcus
Coronal sulcus is cul-de-sac between glans and foreskin
Foreskin covers glans and presents mucosal (inner) and cutaneous (outer) surface
Frenulum connects foreskin to ventral portion of glans corona
Penile shaft is composed mainly by ventral column of corpus spongiosum and 2 dorsal columns of corpora cavernosa
Penile root anchors penis to perineal membrane and pubic arc
Histological Features
Glans, coronal sulcus, and inner foreskin are covered by nonkeratinized squamous epithelium overlying loose lamina propria
Penile erectile tissues comprising 2 corpora cavernosa (CC) and CS surrounding penile urethra form body of penile shaft
Irregular vascular spaces with intermingling elastic connective tissue form penile erectile tissues
Vascular spaces of CS are more widely spaced and irregular when compared with CC
CC present more densely packed vascular spaces with less intervening stroma
Tunica albuginea composed of dense connective tissue encompasses both CC and separates them from CS
CS is also covered by tunica albuginea
Outer foreskin and shaft are covered by skin
Bundles of dartos muscle extend underneath dermis throughout shaft and foreskin
EPIDEMIOLOGY
Age Range
Most frequent in 6th to 7th decades
Average age is 58 years
Incidence
SCC represents most common malignant tumor of penis
Wide range of geographical variation
Low incidence in USA and Europe
High incidence in South America, Africa, Asia
Natural History
Local invasion of penile anatomical levels
Extension to adjacent tissues
Scrotum, perineum, prostate
Metastasis to inguinal lymph nodes
Sentinel node(s), superficial and deep nodes
Metastasis to pelvic lymph nodes
Systemic dissemination (nonregional lymph nodes, visceral, and bone involvement)
Liver is most common site of metastatic dissemination followed by lungs and heart
Systemic dissemination presents in up to 1/3 of patients in high-risk regions
ETIOLOGY/PATHOGENESIS
HPV-Related
30-40% of all SCC are HPV-related
High-risk HPV predominates
HPV-16 is most common genotype encountered
HPV-18 is 2nd most common type
Other reported genotypes include 45, 52, and 74
Low-risk HPV infection is uncommon
Low-risk HPV reported are genotypes 6 and 11
Striking correlation of HPV presence and tumor morphology
Basaloid and condylomatous (warty) SCC are HPV-related in most cases
HPV incidence is low in usual, sarcomatoid, and papillary SCC
HPV-Unrelated
Verrucous, pseudohyperplastic, and cuniculatum SCC are typically HPV-negative tumors
Chronic inflammatory conditions (such as lichen sclerosus) are common in these cases
Risk Factors
Phimosis is major risk factor for penile cancer
Lack of neonatal circumcision
HPV infection (especially by high-risk genotypes)
History of genital warts
Poor hygiene
Smoking
Treatment with psoralen and ultraviolet A (PUVA) therapy
CLINICAL IMPLICATIONS
Clinical Presentation
Most penile SCCs originate from squamous mucosal surface of distal penis (glans, coronal sulcus, &/or foreskin)
Glans is most common affected site followed by inner foreskin and coronal sulcus
About 1/2 of penile carcinomas affect multiple anatomic compartments
SCC of penile shaft are exceedingly rare
Presence of painless tumoral mass is most frequent clinical presentation
Ulceration may be present
Urinary obstruction secondary to urethral tumoral extension is uncommon
Phimosis is found in 50% of cases
MACROSCOPIC FINDINGS
General Features
Patterns of growth include superficial spreading, vertical, verruciform, and multicentric
Superficial spreading
Broad horizontal/superficial extension with involvement of 1 or more anatomical compartments
Extensive in situ component with tumoral invasion usually confined to lamina propria
Vertical growth
Deeply infiltrative tumor with frank invasion of corpus spongiosum or corpus cavernosum
Verruciform
Exophytic cauliflower-like tumor mass usually invading only superficial anatomical levels
Multicentric
Presence of 2 or more independent foci of SCC
Mixed/combinations of any of aforementioned patterns may be seen
Superficial spreading tumors show intermediate risk for inguinal metastasis
Vertical growth tumors show higher rate of nodal involvement and poor outcome
Verruciform tumors may reach large sizes but tend to be localized and metastatic rate is low
In multicentric tumors, foci should be separately evaluated
Specimen Handling
Wide local excision specimen
Fix in 10% buffered formalin, preferably overnight
Measure and describe specimen, identifying and describing tumor
Photograph or diagram specimen
Ink entire surgical margin of specimen
Section specimen transverse to longest axis
Submit tumor entirely if < 3-4 cm and section at least 1 per cm, including grossly apparent deepest penetration and all margins (if not entirely submitted)
Circumcision specimen for tumor
Lightly stretch and pin specimen to flat surface
Fix in 10% buffered formalin, preferably overnight
Measure and describe specimen, identifying and describing tumor
Photograph or diagram specimen
Ink mucosal and cutaneous margins of resection with different colors
Section specimen transversally to its longest axis
Label each section from 1-12 clockwise
Submit entirely if < 3-4 cm, section at least 1 per cm, including grossly apparent deepest penetration and all margins (if not entirely submitted)
Partial/total penectomy specimen
Fix entire specimen in 10% buffered formalin, preferably overnight
When fixed, section specimen in 2 halves using meatus and anterior urethra as a guide
Do not probe urethra
If foreskin is not affected by tumor, separate leaving 3 mm margin from coronal sulcus and include as circumcision specimen
If foreskin is affected by tumor, do not remove
Photograph or diagram specimen, focusing on tumor invasion of anatomic levels
Section each 1/2 longitudinally to longest axis, at 3-5 mm intervals
Photograph (or diagram) and submit entirely section, depicting deepest anatomic level infiltrated by tumor
If tumor affects multiple anatomic compartments, at least 3 sections of each affected compartment should be submitted
Sections should always include adjacent nontumoral mucosa
Resection margins in partial penectomies are urethra and periurethral tissues; corpora cavernosa and skin of shaft should be appropriately submitted
Lymphadenectomy specimen
Fix in 10% buffered formalin, preferably overnight
Identify number and size of all lymph nodes
If feasible, record anatomic location of lymph nodes as upper inner quadrant, superficial and deep inguinal nodes
Submit all lymph nodes for histologic examination
MICROSCOPIC FINDINGS
General Features
Most penile cancers are SCCs, but there are several histological subtypes/variants
Each subtype is usually associated with defined clinical outcome and prognosis
Subtyping helps in management of therapy
Some variants are often treated more aggressively than others
Histological Subtypes
Subtyping should always be done following strict morphological criteria
Histological subtypes of penile SCC include
Usual
Verrucous
Papillary, not otherwise specified (NOS)
Warty (condylomatous)
Basaloid
Adenosquamous
Pseudoglandular (acantholytic, adenoid)
Cuniculatum
Pseudohyperplastic
Sarcomatoid
Mixed
Each histologic subtype often clinically behaves in distinctive fashion
Verruciform tumors and pseudohyperplastic carcinomas are associated with low risk for nodal metastasis
Tumors with high risk for nodal involvement include basaloid, sarcomatoid, adenosquamous, and poorly differentiated usual SCC
Low-grade usual SCC, some mixed tumors, and pleomorphic variants of warty carcinoma are in intermediate category
Correlation of Pattern of Growth and Histological Subtype
Verruciform tumors include warty (condylomatous), verrucous, papillary NOS, and cuniculatum carcinomas
Basaloid, high-grade usual type, and sarcomatoid SCCs (aggressive variants) usually present with vertical pattern of growth
Superficial spreading growth pattern is characteristic of low-grade variants of SCC
Multicentricity is more common in low-grade highly differentiated SCC variants, especially those located in foreskin (e.g., pseudohyperplastic SCC)
Mixed patterns of growth are usually observed in mixed low- and high-grade variants of SCC
Histological Grade
Important predictive factor of inguinal lymph node metastasis and outcome
Grading should always be done following strict morphologic criteria
Criteria for grading
Grade 1
Almost normal to slightly enlarged nuclei and abundant eosinophilic cytoplasm
Minimal basal/parabasal atypia and prominent keratinization
Grade 2
More disorganized growth compared to grade 1 lesions
Higher nuclear:cytoplasmic ratio, evident mitoses, and less prominent keratinization
Grade 3
Tumors composed of any proportion of anaplastic cells with evident nuclear pleomorphism
Heterogeneous tumors showing areas with different histologic grades are seen in up to 1/2 of all cases
Tumor grading should be performed considering highest grade component, regardless of its proportion
Depth of Invasion/Tumor Thickness
Depth of invasion measured from basal cell layer of adjacent normal epithelia to deepest point of infiltration
Thickness measured from nonnecrotic nonkeratinized tumor surface to its deepest point of infiltration
Depth and thickness are equally useful, except for verruciform tumors, for which depth of invasion should be preferred
In tumors measuring < 5 mm, there is minimal risk for nodal metastasis
In tumors measuring > 10 mm, there is high risk for nodal involvement
In tumors measuring 5-10 mm, histological grade and perineural invasion are helpful to estimate potential for nodal metastasis
Anatomic Level of Invasion and Pathologic Stage
Deepest anatomic level infiltrated by tumor should always be carefully determined
Anatomic levels in glans include
Squamous epithelium (level 0)
Lamina propria (level 1)
Corpus spongiosum (level 2)
Corpus cavernosum, including tunica albuginea (level 3)
Anatomic levels in foreskin include
Glans tumors are usually of higher grade and more deeply infiltrating
Superficial tumors invading lamina propria or superficial corpus spongiosum are associated with low risk for nodal metastasis
Tumors invading deep corpus spongiosum or corpora cavernosa are at high risk for nodal metastasis
Cancer specific mortality is 0%, 11%, and 20% for tumors invading lamina propria, corpus spongiosum, and corpora cavernosa, respectively
Tumors exclusive of foreskin show lower rate of nodal metastasis
Tumor staging is done considering deepest invasion of penile tissue (T), status of inguinal lymph nodes (N), and presence of distal metastasis (M)
Broad pushing nondestructive penetration is permitted in noninvasive verrucous carcinoma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree