Prostate, General Concepts
Gladell P. Paner, MD
ANATOMIC FEATURES
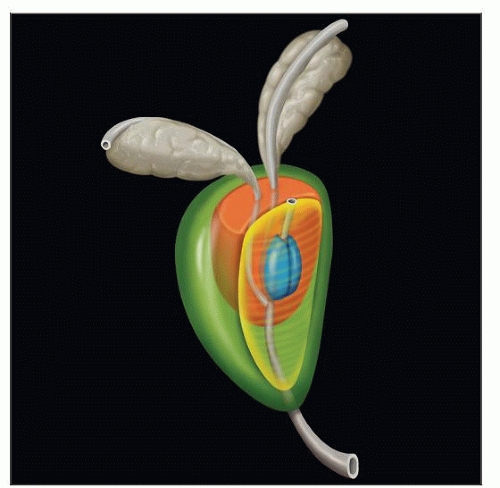
Prostate Gland
Exocrine compound tubulo-alveolar gland
Located in true pelvis
Surrounded by urinary bladder superiorly, transverse urogenital diaphragm inferiorly, inferior aspect of symphysis pubis anteriorly, and rectum posteriorly
Inverted conical shape: Base is broad superior region, and apex is tapered inferior region
Base contiguous with bladder neck superiorly and seminal vesicle attachment posteriorly
Apex blends with striated muscle of transverse urogenital diaphragm
Normal prostate in men (21-30 years old) weighs ˜ 20 g (range 14-26 g)
In adults, usually measures 4 x 3 x 2 cm
Widest at transverse dimension of base
McNeal anatomic model divides prostate into glandular and nonglandular components
Glandular component
Peripheral zone, central zone, transition zone, periurethral gland region
Nonglandular component
Anterior fibromuscular stroma, preprostatic sphincter, striated sphincter
Receives arterial supply from inferior vesical and middle rectal arteries, branches of internal iliac artery
Prostatic venous plexus lies partly within prostatic fascial sheath and drains into internal iliac vein
Primary lymphatics drain into regional lymph nodes in true pelvis
Hypogastric, obturator, internal and external iliac, and sacral lymph nodes
Prostatic Urethra
Approximately 3 cm in length and begins at internal urethral orifice at apex of bladder trigone
Courses through prostate, makes anteriorly concave 35° bend, ends as urethra penetrates fascia of urogenital diaphragm and enters perineum
Continues distally as membranous urethra
Posterior wall of prostatic urethra has several unique features related to prostatic secretory function
Contains a longitudinal ridge (urethral crest) lined by 2 adjacent grooves (prostatic sinuses)
Prostatic ductules enter urethra predominantly in sinuses with fewer entering along lateral aspects of crest
Urethral crest also has midline protuberance (verumontanum or colliculus seminalis)
Verumontanum (Colliculus Seminalis)
Protrusion of prostatic tissue from posterior wall of urethra at angulation, tapers distally as crista urethralis
Contains epithelium-lined blind sac (utricle) between openings of paired ejaculatory ducts
Ejaculatory Duct
Passes through central zone entering at cephalad aspect
Both ducts open into prostatic urethra at verumontanum, lateral to prostatic utricle
Seminal Vesicle
Attached to superior-posterior aspect of prostate and bladder base
Paired, highly coiled epithelial-lined tubes with irregular outpouchings
Small intraprostatic portion is seen
Excretory duct connects anteriorly with ampullary portion of vas deferens forming ejaculatory duct
In adults, average 6 x 2 cm and contains up to 5 mL milky fluid, which forms bulk of ejaculatory volume
Periprostatic Structures
Resected prostate may include adjoining tissues, such as adipose tissue, neurovascular bundle, paraganglia, Denonvilliers fascia, and lateral prostatic fascia
Potency-sparing prostatectomy preserves neurovascular bundle, site of cavernous nerves important for erection
SPECIMEN TYPES AND HANDLING
Needle Core Biopsy
Indication is for histologic diagnosis of prostate cancer and evaluation of mass lesion or hypoechoic region
Performed for elevated serum PSA level &/or abnormal digital rectal examination (DRE)
Performed almost universally via transrectal ultrasound (TRUS)-guided using 18-gauge needle as outpatient procedure
May also be performed perineally or transurethrally
Different prostate biopsy sampling schemes
Sextant biopsy (6 cores)
Use remains widespread despite becoming the less preferred technique
Samples bilateral base, midgland, and apex
Extended biopsy (10-12 cores)
Preferred initial diagnostic procedure
Demonstrated increased cancer detection rate without increase in morbidity
False-negativity rate of 5% (vs. ~ 25% for sextant biopsy)
Optimal extended biopsy includes standard sextant area plus cores that target mid and lateral peripheral zone
Transition zone biopsy is not usually recommended at initial biopsy due to low detection rate
Saturation biopsy (≥ 20 cores)
Does not improve cancer detection when performed as initial procedure
Considered in men with persistently elevated PSA and several prior negative biopsies
Includes biopsy of transition zone
Handling of biopsy specimen
If possible, avoid accessioning prostate biopsy specimens in sequence
Count and document number of cores per container
Ideally core(s) submitted in 1 container per site (> 3 is detrimental for evaluation)
Formalin fixative is preferred
Bouin solution is not preferred as it may enhance nucleoli in benign glands
Hematoxylin or other indelible dye makes tissue cores more visible when cutting paraffin blocks
Ideally, submit only 1-2 tissue cores per block to maximize tissue representation
More cores per block often leads to undesired tissue loss
Prospectively cut intervening unstained slides to ensure presence of atypical focus for adjunctive immunostains
Levels 1, 3, and 5 for H&E staining
Save unstained levels 2, 4, and 6 for potential immunohistochemistry (IHC) or H&E stains
Attempting immunostains on subsequent deeper levels more frequently results in loss of atypical focus
Multiple sections (ideally 3) should be present on each H&E slide to enhance sampling
Most of the tissue in the block from superficial to deep should be included in sections
Fine Needle Aspiration Biopsy
Rarely performed in USA
Advocates claim aspiration cytology is cheaper, faster, easier to use, and has less morbidity
Major drawback is lack of cancer architecture that precludes Gleason grading and distinction from HGPIN
Inability to provide important information for planning therapy and prognostication
Transurethral Resection of Prostate (TURP) or Subtotal Prostatectomy
TURP is surgical treatment of choice for benign prostatic hyperplasia (BPH)
Open simple prostatectomy may be performed for bulky BPH
Incidental prostate cancer encountered in ~ 10%
TURP specimen consists of elongated rubbery fragments called prostate chips
Includes transition zone and areas around proximal prostatic urethra
Handling of TURP specimen
Specimens ≤ 12 g: Submit entirely
For > 12 g: Submit initial 12 g (6-8 cassettes) and 1 cassette for every additional 5 g
Sensitivity for cancer detection may be increased by selectively submitting chips that are firm, yellow, or grossly suspicious for cancer
If incidental prostate cancer comprises < 5% of tissues examined, entire remaining tissue should be submitted
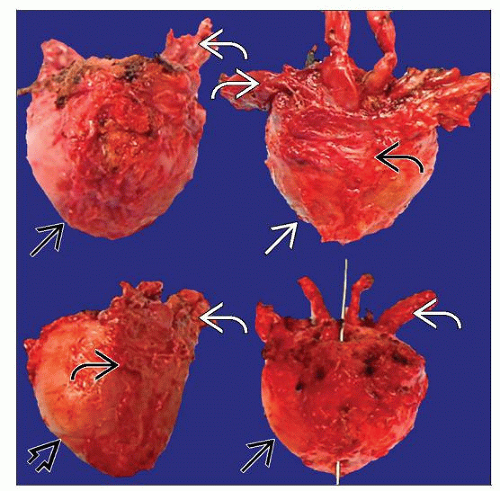
Radical Prostatectomy (RP)
Most common treatment for localized prostate cancer (cT1-T2), when life expectancy is > 10 years
Retropubic, laparoscopic, or robotic-assisted
Increasing popularity of robotic-assisted prostatectomy
˜ 40% of radical prostatectomies performed in USA in 2006 were robotic-assisted
Data comparing outcomes between surgical methods is starting to emerge
Handling of RP specimen
Weigh and measure specimen in 3 dimensions
Unless being sampled for research, fix in 10% buffered formalin for 18-24 hours
May use microwave-assisted technique to facilitate fixing
Ink entire outer surface using 2 colors to identify right and left sides
Apex, base, and seminal vesicles should be handled in standardized fashion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree