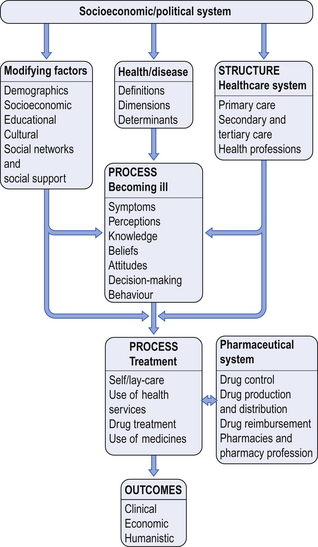
2 To develop a full understanding of the use of medicines by individuals and society and the role that pharmacy contributes to health care, an understanding of the sociology and psychology of health is required. These two factors are closely interwoven, and help the pharmacist to understand the influences on an individual’s behaviour in relation to their health and any illness they encounter. It is impossible in two chapters to provide a comprehensive review of all the aspects of health sociology and psychology that may be relevant to pharmacy. Instead, the aim is to highlight the relevant key areas that may lead the reader to explore the sociological and psychological literature in more detail; a good starting point is the books and articles on the topic that are included in the further reading (Appendix 4). An overall framework is presented in Figure 2.1. The WHO definition of health distinguishes between three aspects; physical, mental and social health, but very often healthcare systems use a narrower definition of health incorporating only physical and mental health to focus their resource allocation. The biomedical model of disease proposes that all diseases and illness can be explained by disturbed physiological processes. The disturbances may be caused by injury, biochemical changes and bacterial, viral or fungal infection. This model separates the physical from the psychological and sociological influences on health. The biomedical model has dominated healthcare processes for a significant period of time, but in more recent years, there has been a recognition that it is not possible, or helpful, to separate out the components of an individual’s life; the biopsychosocial model incorporates the interplay of biological, psychological and social aspects of a person’s life on their health. Stress can also affect an individual’s health through altered health-related behaviour. People experiencing high levels of stress often consume more alcohol, drugs and smoke more than those with less stress, and they also experience more accidents. These differences in social situations that produce an effect on health are referred to as ‘health inequalities’. Health inequalities within a society are often targeted with resources and interventions in order to try and produce population-wide improvements and equality in health (see Ch. 13).
Socio-behavioural aspects of health and illness
 The importance of social and behavioural sciences to pharmacy
The importance of social and behavioural sciences to pharmacy
 The meaning of health and illness
The meaning of health and illness
 Changing health-related behaviour and the related models
Changing health-related behaviour and the related models
 How people behave when they are ill
How people behave when they are ill
 Behavioural aspects of health care
Behavioural aspects of health care
Introduction
 Analysing the practice of pharmacy – helping to identify important questions relating to the use of medicines, pharmacy practice and the pharmacy profession
Analysing the practice of pharmacy – helping to identify important questions relating to the use of medicines, pharmacy practice and the pharmacy profession
 Providing conceptual and explanatory frameworks for understanding human behaviour in a social context
Providing conceptual and explanatory frameworks for understanding human behaviour in a social context
 Providing appropriate approaches to study the use of medicines and the practice of pharmacy.
Providing appropriate approaches to study the use of medicines and the practice of pharmacy.
Dimensions of health
Determinants and models of health
Behavioural determinants
Environmental determinants
Socioeconomic determinants
Interaction of different factors
 Psychosocial environment (e.g. personal relationships, housing)
Psychosocial environment (e.g. personal relationships, housing)
 Microphysical environment (e.g. chemicals and noise)
Microphysical environment (e.g. chemicals and noise)
 Work environment (e.g. work stress)
Work environment (e.g. work stress)
 Behavioural environment (e.g. smoking, alcohol use, exercise)
Behavioural environment (e.g. smoking, alcohol use, exercise)
 The political/economic climate (e.g. unemployment level)
The political/economic climate (e.g. unemployment level)
 The macro-physical environment (e.g. air quality)
The macro-physical environment (e.g. air quality)
 Social justice/equity (e.g. social security system)
Social justice/equity (e.g. social security system)
Process of illness
Becoming ill
 Health behaviour, which refers to ‘any activity undertaken by people believing themselves to be healthy for the purpose of preventing disease or detecting it at an asymptomatic stage’
Health behaviour, which refers to ‘any activity undertaken by people believing themselves to be healthy for the purpose of preventing disease or detecting it at an asymptomatic stage’
 Illness behaviour, which involves an activity undertaken by people experiencing illness, in order to determine their state of their health and receive appropriate treatment
Illness behaviour, which involves an activity undertaken by people experiencing illness, in order to determine their state of their health and receive appropriate treatment
 Sick-role behaviour, which refers to the activity that individuals, who consider themselves ill, undertake in order to get well.
Sick-role behaviour, which refers to the activity that individuals, who consider themselves ill, undertake in order to get well.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Socio-behavioural aspects of health and illness
Only gold members can continue reading. Log In or Register to continue