decreased enterocyte integrity  bacterial translocation
bacterial translocation  sepsis
sepsis
•Enteroendocrine cells
•I cells—secrete CCK
•Stimulates gallbladder contraction and pancreatic enzyme secretion
•Stimulates sphincter of Oddi relaxation
•S cells—secretin
•Stimulates HCO2, pancreatic enzyme, and intestinal secretion
•Stimulated by duodenal acidification (pH <3)
•D cells—somatostatin
•Inhibits release of all GI hormones
•K cells—gastric inhibitory peptide
•Stimulates insulin secretion
•Inhibits gastric acid secretion
•Paneth cells
•In the bases of the crypts of Lieberkuhn
•Aid in phagocytosis and mucosal defense
•M cells
•Ag presenting cells in Peyer patches
•Brunner glands
•In the duodenum
•Produce alkaline solution to protect against gastric acid
Portions of the Small Intestine
•Duodenum
•Bulb (first portion)—90% of ulcers occur here
•Descending (second portion)—contains ampulla of Vater
•Transverse (third portion)
•Ascending (fourth portion)
•Descending and transverse portions are retroperitoneal
•third and fourth portions are the transition point at the acute angle between the aorta (posterior) and the superior mesenteric artery (SMA) (anterior)
•With a narrowing of this angle, can have SMA syndrome
•Jejunum
•Starts at the ligament of Treitz and is about 100 cm long
•Long vasa recta and circular muscle folds
•Maximum site of all absorption except for
•B12—terminal ileum
•Folate—terminal ileum
•Bile acids—terminal ileum
•Iron—Duodenum
•95% of NaCl and 90% of water absorbed in jejunum
•Ileum
•150 cm long
•Short vasa recta
•Blood supply to duodenum is celiac and SMA
•Blood supply to jejunum and ileum is SMA
Nutrient Absorption
•Water and electrolytes
•Sodium transport creates an osmotic gradient that drives water absorption
•Na, Cl, K, Ca, Mg, and Fe are absorbed in the small bowel
•Carbohydrate digestion
•Begins in the mouth with salivary amylase
•Continues with pancreatic amylase and disaccharidases
•Intestinal brush border has maltase, sucrase, dextrinase, and lactase
•Carbohydrates are broken down into glucose, galactose, and fructose
•Glucose and galactose
•Absorbed at brush border by secondary active transport via sodium co-transporter SGLUT1
•Fructose
•Absorbed at brush border by facilitated diffusion by GLUT5
•All then enter the bloodstream via GLUT-2 facilitated diffusion at the basolateral surface of the enterocytes
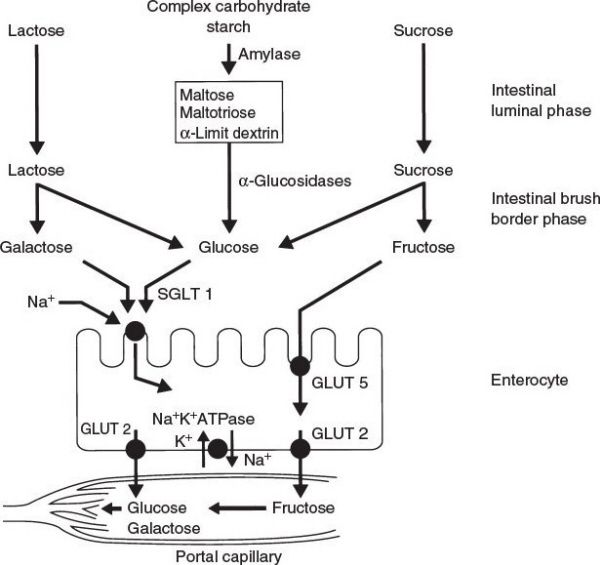
Carbohydrate metabolism. (With permission from O’Leary JP, Tabuenca A, eds. Physiologic Basis of Surgery. 4th ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2007.)
•Protein digestion
•Begins in stomach with pepsin
•Continues in small intestine with trypsin, chymotrypsin, and carboxypeptidase where proteins are broken down into amino acids and di- and tripeptides
•Amino acids are absorbed at the brush border by secondary active transport with Na
•Di- and tripeptides are absorbed at the brush border by secondary active transport with H
•They then enter the bloodstream via diffusion at the basolateral surface
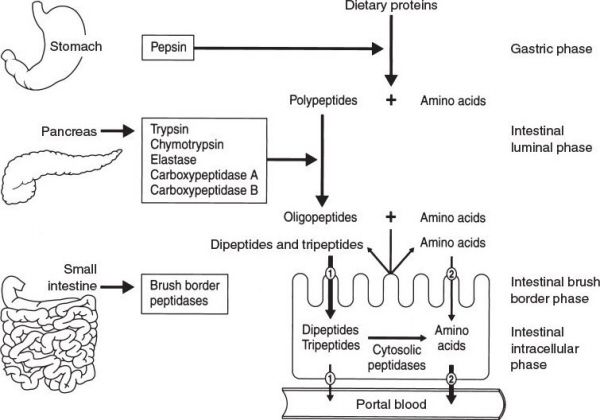
Protein metabolism. (With permission from O’Leary JP, Tabuenca A, eds. Physiologic Basis of Surgery. 4th ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2007.)
•Lipid digestion
•Triglycerides (TGs) are digested by lipases at the brush border to form monoglycerides and free fatty acids (FFAs)
•Micelles are then formed with the monoglycerides, FFAs, bile salts, phospholipids, and cholesterol
•Bile salts increase absorption area for fats, helping for micelles
•Fat soluble vitamins A, D, E, and K are also absorbed in micelles
•Micelles then enter the enterocyte by fusing with the membrane
•In the enterocytes, TGs reform
•TGs and cholesterol then form chylomicrons, which are transported to lymphatics (lacteals) via basolateral exocytosis
•Chylomicrons are 90% TGs, 10% phospholipid, cholesterol, and protein
•Long chain fatty acids are also released into lymphatics
•Medium and short chain fatty acids are released into portal vein (as with amino acids and carbohydrates)
•Lipoprotein lipase
•On the liver endothelium
•Clears chylomicrons and TAGs from blood and breaks them down into fatty acids and glycerol
•Fatty acids and glycerol are then are taken up by hepatocytes
•FFA-binding protein
•On liver endothelium
•Binds short and medium chain fatty acids
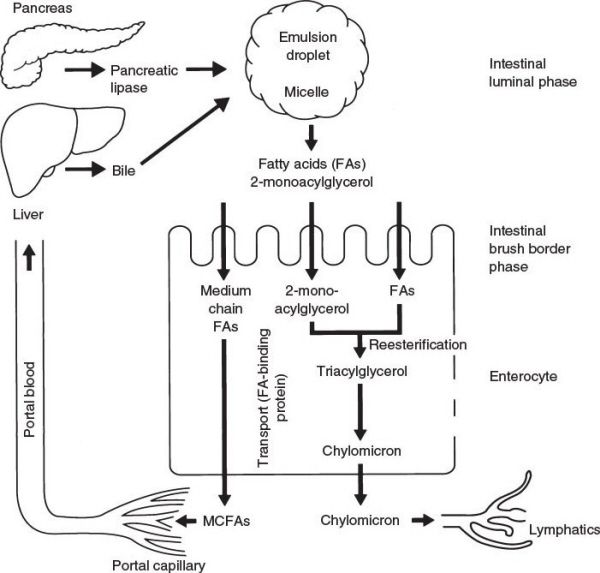
Lipid metabolism. (With permission from O’Leary JP, Tabuenca A, eds. Physiologic Basis of Surgery. 4th ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2007.)
Small Bowel Motility
•MMC
•Basic motility pattern resulting in the propagation of cellular debris, bacteria, and chyme
•Starts in the stomach and progresses through the small intestine over approximately 2 hours
•Phase I: Period of inactivity (60 to 75 minutes)
•Phase II: Period of increasing irregular bowel contractions (up to 60 minutes)
•Phase III: Period of maximal contractions, rapid spikes, and muscular contraction (5 to 10 minutes)
•Phase IV: Slowing of activity
•Motilin is the hormone that mediates the MMC
•Erythromycin acts as a motilin analogue and induces the MMC in the fasted state in humans
•Cyclic activity continues until interrupted by a meal
•After a meal, the MMC is replaced by 3 to 4 hours of rapid spiking activity, similar to Phase II
•Contractions occur throughout the intestine with a caudal spread
Small Bowel Immunity
•Largest immune organ in the body
•Gut-associated lymphoid tissue is composed of aggregated tissue (Peyer patches, lymph nodes, and lymphoid follicles) and free leukocytes
•B lymphocytes produce secretory IgA
The small bowel is the largest immune organ of the body, with a large role in antigen presentation. Secretory IgA is a key mediator of gut immune defenses.
A 50-year-old woman with a history of multiple previous pelvic operations presents to the emergency department with a 2-day history of abdominal pain, distention, nausea, vomiting, and reports no bowel movements for 36 hours. What is the first diagnostic test of choice?
An abdominal X-ray series (flat and upright) is the initial study for a suspected small bowel obstruction. A hernia is the most common cause of a small bowel obstruction in a patient without a history of previous abdominal operations.

AXR showing an SBO. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
Small Bowel Obstruction
•Caused by adhesions (most common cause), hernias, and tumors
•Other causes include volvulus, intussusception, Crohn’s disease, and radiation enteritis
•The most common cause in patients with a virgin abdomen is an incarcerated hernia
•It is important to check the groin for both inguinal and femoral hernias
•History of recent bowel movements
•Diarrhea can be a finding with obstruction
•No bowel movements for >3 days indicates obstruction or constipation
•Typical findings on an abdominal X-ray with flat and upright (or decubitus) views include air fluid levels and dilated small bowel
•The absence of gas in the colon or rectum can indicate a complete obstruction
•A CT scan is 90% sensitive and specific for diagnosing a small bowel obstruction and can isolate the obstruction site (transition point)
•Conservative management includes bowel rest and possible decompression using an NG tube
•Indications for surgery include signs of strangulation or perforation (progressive pain, peritoneal signs, fever, increasing white cell count) or a lack of improvement with conservative management
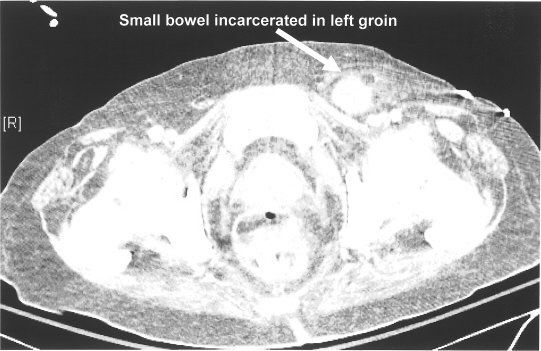
Incarcerated hernia. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
Bowel rest with an NG tube and IV fluids cures 80% of partial small bowel obstructions and 20% of complete small bowel obstructions.
A 67-year-old male who presented to the hospital with RUQ pain and jaundice and was found to have a common bile duct stone undergoes an endoscopic retrograde cholangiopancreatography (ERCP) and sphincterotomy. That evening, he develops worsening abdominal pain and peritonitis. A CT scan is performed and he is found to have retroperitoneal air. What is the next step in management?
Duodenal perforation occurs in 1% of ERCPs. If the patient is stable, they can be managed conservatively with NGT, IV antibiotics, serial abdominal exams, and bowel rest. If they become unstable or develop peritonitis, they should undergo an exploratory laparoscopy or laparotomy. In the majority of cases, the exact area of perforation is not visible at the time of exploration and wide drainage of the duodenum is usually sufficient to control the leak.
A 60-year-old man is recovering on postoperative day 6 following a low anterior colon resection. He develops nausea and emesis and has had no passage of flatus or stool since the operation. On CT scan, his bowel is diffusely dilated with no transition point. What possible factors may have contributed to his condition?
Postoperative ileus usually occurs in the first few hours after surgery and can persist for days to weeks. It is characterized by the lack of an abrupt transition point on imaging studies. It is caused by increased catecholamines, opiates, inhaled anesthetics, inflammation, surgical manipulation, electrolyte imbalance, and intra-abdominal infection. Patients with a history of prior surgery are more likely to develop a postoperative ileus because more bowel manipulation is often required. Laparoscopy is associated with lower rates of postoperative ileus.
Ileus
•Defined as a temporary inhibition of coordinated gastrointestinal motor function
•Common causes include major abdominal surgery, spinal surgery, spinal trauma, and opiates
•Treatment is with bowel rest and supportive therapy
•Postoperative ileus generally resolves 4 to 5 days following a laparotomy
•Laparoscopic surgery is associated with a shorter period of postoperative ileus
•Consider a mechanical obstruction in the differential diagnosis if the ileus does not resolve
•Parenteral nutrition may be indicated if the patient is NPO for >1 week
Return of function occurs in the small bowel first (usually within 1 to 2 days), followed by the stomach (usually within 2 to 3 days), then the colon (usually within 3 to 4 days).
A 79-year-old woman with symptoms of small bowel obstruction is found on an abdominal X-ray series (flat and upright) to have dilated small bowel loops, air in the biliary tree, and a large radiolucent round object in the right lower quadrant. What is the most likely diagnosis?
This patient has a gallstone ileus, which can occasionally be diagnosed on plain films and is caused by a fistula between the gallbladder and the bowel (typically the duodenum). Treatment is to surgically remove the impacted gallstone and, if the patient is stable, cholecystectomy and closure of the fistula.
Gallstone Ileus
•Bowel obstruction caused by a gallstone
•Classically occurs in elderly patients
•Caused by a fistula between the gallbladder and second portion of the duodenum
•Inflammation from cholecystitis causes erosion into the duodenum
•Can erode into the transverse colon, stomach, or jejunum, but this is rare
•Bouveret syndrome refers to gastric outlet obstruction due to a gallstone impacted in the duodenal bulb
•Treatment is removal of the stone from the terminal ileum and a cholecystectomy with duodenal closure
•A cholecystectomy and fistula closure in the setting of gallstone ileus with obstruction should only be undertaken if the patient is stable
•The cholecystectomy can be delayed if the patient is not stable
Up to 40% of patients with gallstone ileus will have a second stone. Always search for a second stone when exploring these patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


