Size and Multiple Foci
INTRODUCTION
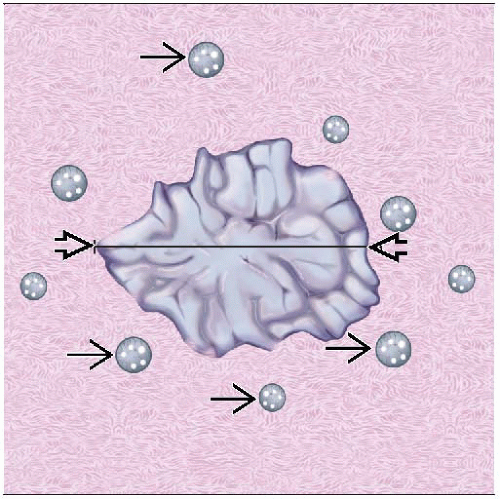
Size of Invasive Cancer
Important independent prognostic factor for both node-negative and node-positive patients
Size is defined as greatest linear dimension of an invasive carcinoma
Adjacent carcinoma in situ is not included in determination of size
Cancers grow at very different rates
Some cancers grow very slowly or appear stable in size for many years
Typically well-differentiated ER positive cancers
Other cancers grow rapidly
Most common in young women
In older women, may be detected as “interval cancers”: Cancers detected by palpation in time between mammographic screening
Typically poorly differentiated ER negative cancers
Typical size of cancers detected by palpation is 2-3 cm
Screening by patient self breast examination does not decrease number of breast cancer deaths
Suggests that by the time a carcinoma is palpable, carcinomas capable of metastasizing will have already done so
Nonpalpable invasive carcinomas detected by screening are much smaller in size
Average size of carcinomas associated with a mammographic density is about 1 cm
Average size of carcinomas detected as mammographic calcifications (without an evident mass) is 0.6 cm
More often well differentiated, tubular type, and ER positive
Screen-detected cancers have better prognosis than palpable cancers of same size
Important to carefully identify node-negative carcinomas ≤ 1 cm in size
These patients have an excellent prognosis and may not require systemic therapy
Majority of patients with carcinomas > 1 cm will be offered systemic therapy
Lymph node metastases are closely correlated with size
Likelihood of nodal metastases increases rapidly from cancer size 0-4 cm and then levels off at ˜ 70-90%
Some very large carcinomas do not metastasize to axillary lymph nodes
May metastasize using blood vessels or via lymphatics to internal mammary nodes
Some carcinomas reach very large size without metastasis, likely due to as yet unidentified biologic factors
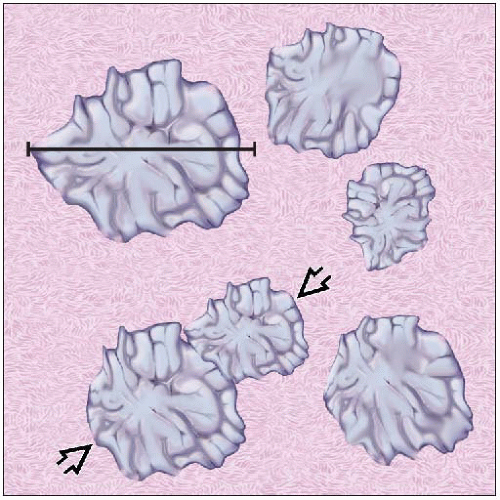
Multiple Invasive Cancers
10-40% of patients have more than 1 focus of invasive carcinoma in same breast at time of diagnosis
Incidence increases with more extensive imaging workup (including MRI) &/or detailed pathologic evaluation
MRI finds additional foci of cancer in 10-30% of patients
Patients with multiple cancers are more likely to have family history of breast carcinoma, have lobular carcinomas, and are at greater risk for contralateral carcinoma
Terms “multifocal” and “multicentric” have been used to describe cases of multiple cancers but have been defined in different ways
Do not always specify whether carcinoma in situ is included in the definition
Some definitions only include grossly identified invasive carcinomas, whereas others include microscopic carcinomas
Multifocal is generally defined as > 1 focus of invasive carcinoma within 1 quadrant
Multicentric has multiple definitions
≥ 2 foci in different quadrants of breast
≥ 2 foci a certain distance apart, which can be from 2-5 cm
Foci involving different ductal systems
≥ 2 biologically independent cancers
“Multicentric” and “multifocal” are not useful terms unless specifically defined
Difficult to apply to most pathology specimens
Do not address the underlying biology responsible for the multiple foci of invasion
Multiple invasive cancers are associated with greater incidence of lymph node metastases
Each cancer has an independent risk of metastasis; thus, overall risk is increased
Multiple foci of invasion do not diminish survival as compared to a single focus of invasion, if adjusted for number of lymph node metastases
5 etiologies for multiple foci of invasion
Extensive DCIS
Most common setting in which multiple invasive carcinomas arise
Carcinomas are usually very similar to each other with respect to grade, histologic type, and tumor markers
In unusual cases, there is marked heterogeneity in underlying DCIS leading to heterogeneity in associated invasive carcinomas
HER2 positive carcinomas are more commonly associated with extensive DCIS with multiple foci of invasion
Invasive carcinoma with extensive lymphvascular invasion (LVI) and intramammary metastases
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree