Sex Cord Stromal Tumor, Mixed/Unclassified
Steven S. Shen, MD, PhD
Jae Y. Ro, MD, PhD
Key Facts
Terminology
Group of SCST with mixture of recognizable types
SCST with incomplete differentiation or undifferentiated spindle cells or mixed spindle and epithelioid cells
Clinical Issues
Extremely rare (< 1% of testicular neoplasms)
Macroscopic Features
Well-circumscribed, lobulated, white-yellow nodule
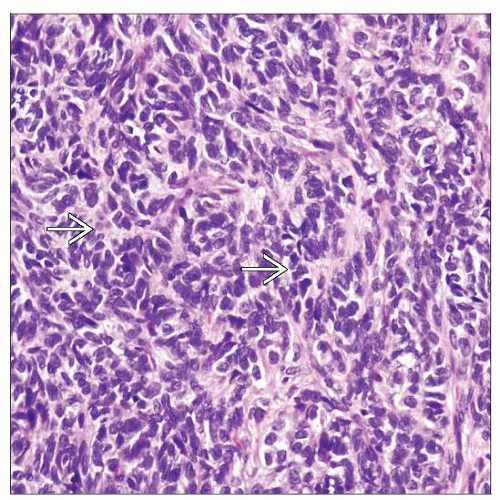
Microscopic Pathology
Mixture of growth patterns and mixture of recognizable SCST components (LCT, SCT, or GCT)
Mixture of epithelioid and undifferentiated spindle cell components
Epithelioid component forms solid or hollow tubules, irregular aggregates, or anastomosing trabeculae
Round to ovoid cells with eosinophilic, amphophilic, or vacuolated cytoplasm
Undifferentiated stromal cell component is usually hypercellular spindle cells and merged with fibrous stroma
Features that are seen more often in malignant tumors: Invasive growth, angiolymphatic invasion, nuclear atypia, mitotically active, and areas of necrosis
Ancillary Tests
Positive for vimentin, desmin, actin-sm, S100, CD99, cytokeratin (may be focal), inhibin and calcitonin (focal)
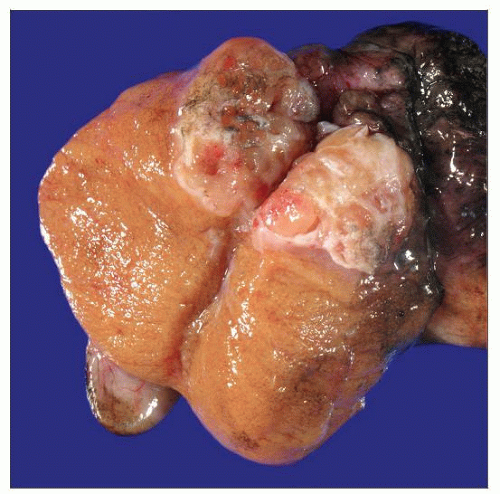 Gross photograph shows a well-circumscribed unclassified SCST. It has heterogeneous, soft, tan nodular areas with dense white fibrotic septae. SCSTs frequently do not replace the entire testis. |
TERMINOLOGY
Abbreviations
Sex cord stromal tumor (SCST), Leydig cell tumor (LCT), Sertoli cell tumor (SCT), granulosa cell tumor (GCT)
Definitions
Group of SCSTs with mixture of recognizable cell types or composed of incomplete or undifferentiated sex cord stromal cells
CLINICAL ISSUES
Epidemiology
Incidence
Extremely rare (< 1% of testicular neoplasms)
Age
All ages
More commonly seen in children (30% < 1 year old)
Presentation
Painless testicular enlargement
15% associated with gynecomastia
Treatment
Surgical approaches
Surgical resection is usually curative
Testis sparing partial orchiectomy may be possible
Radical orchiectomy with retroperitoneal lymph node dissection may be required for patients with clinical evidence of metastasis or high-risk pathologic features
Prognosis
Almost always benign in prepubertal children
May be malignant in adults (20%)
MACROSCOPIC FEATURES
General Features
Well-circumscribed, lobulated, white-yellow, nodular mass; similar to other SCST with no unique gross features
Cystic areas may be seen
Hemorrhage and necrosis are uncommon
MICROSCOPIC PATHOLOGY
Histologic Features
Mixture of recognizable SCST components (Leydig cell, Sertoli cell, or granulosa cell, rarely theca cells)
Mixture of undifferentiated or unclassifiable epithelioid and spindle cell components
Epithelioid component
Solid or hollow tubules, irregular aggregates, or anastomosing trabeculae (SCT)
Round to ovoid cells with eosinophilic, amphophilic, or vacuolated cytoplasm and prominent nucleoli (LCT)
Oval round cells with nuclear grooves, Call-Exner-like bodies (GCT)
Mixture of above mentioned recognizable SCST
Unclassified epithelioid cells with vesicular nuclei, occasional prominent nucleoli, rare mitotic figures
Signet ring cell SCST has been reported
Undifferentiated spindle cell component
Usually hypercellular spindle cells merged with fibrous stroma
Spindle cells may form fascicles
Spindle cells may have nuclear grooves
Cellular pleomorphism and mitotic figures are variable
Has been reported as a variant of granulosa cell tumor because of its immunohistochemical similarities
Features that are more commonly associated with malignant outcome: Invasive growth pattern, angiolymphatic invasion, nuclear atypia, mitotically active, and areas of necrosis
Predominant Pattern/Injury Type
Neoplastic; diffuse spindle cells, mixed epithelioid and spindle cells, or combined form of known SCSTs
Predominant Cell/Compartment Type
Sex cord stromal cells
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree