• Leading cause of impaired vision and blindness in the United States; 4 million people have vision-impairing cataract, and 40,000 people in the country are blind because of cataracts. Cataract surgery is the most common major surgical procedure in the United States. • Classified by location and appearance of lens opacities, cause or significant contributing factor, and age of onset. • Causes and contributing factors: ocular disease, injury, surgery, systemic diseases (diabetes mellitus, galactosemia), toxin, ultraviolet and near-ultraviolet light, radiation exposure, and hereditary disease. • Transparency of lens decreases with age. Most elderly people have some degree of cataract formation, including progressive increase in size, weight, and density of lens throughout life. — Fibrous metaplasia of epithelium — Liquefaction of fibers resulting in Morgagnian globule formation (drops of fluid beneath capsule and between lens fibers) — Sclerosis (melding of fibers) • Topoanatomic classification of cataracts: — Anterior subcapsular cataract: fibrous metaplasia of lens epithelium (after iritis and adherence of iris to lens [posterior synechia]) — Anterior cortical cataract: liquefaction of lens fibers and Morgagnian globules in cortex anteriorly — Nuclear cataract: exaggeration of normal, aging-related, melding of fibers in nucleus — Posterior cortical cataract: liquefaction and globular degeneration of posterior lens cortex — Posterior subcapsular cataract: epithelial cells migrate posteriorly under capsule and form large, irregular nucleated cells • Etiology of cataract: inability to maintain normal homeostatic concentrations of sodium (Na+), potassium (K+), and calcium (Ca2+) within lens, the result of decreased Na+, K+ adenosine triphosphatase (ATPase) activity—a defect from free radical damage to sulfhydryl proteins in the lens, including Na+, K+-ATPase that contains a sulfhydryl component. • Normal protective mechanisms are unable to prevent free radical damage; the lens depends on superoxide dismutase (SOD), catalase, glutathione (GSH), and accessory antioxidants vitamins E and C and selenium (Se) to prevent free radical damage. • People with higher intake of vitamins C and E, Se, and carotenes have a much lower risk for cataracts. • Nutritional supplements—such as multiple vitamin/mineral formulas, vitamins C and E, B vitamins (B12, folic acid), vitamin A—also offer significant protection against nuclear and cortical cataracts. • Lutein: yellow-orange carotene that protects against macular degeneration and cataract formation. Like the macula, the lens concentrates lutein. Spinach (high in lutein) consumption is inversely related to cataract extraction. Intake of lutein is inversely associated with cataract extraction (20%-50% risk reduction). Lutein (15 mg) given three times per week for up to 2 years to patients with age-related cataracts improved visual acuity and glare sensitivity. • Vitamin C: high intake of vitamin C from dietary sources or supplements protects against cataract formation. Supplements can halt cataract progression and, in some cases, improve vision. Supplements reduced cataract development and number of surgeries required among cataract patients over a period of 11 years. Dosage necessary to increase vitamin C content of lens: 1000 mg. Vitamin C in blood is 0.5 mg/dL, but in adrenal and pituitary glands the level is 100 times this and in the liver, spleen, and lens of eye it is 20 times higher. Enormous amounts of energy are required to pull vitamin C out of blood against a tremendous gradient. Keeping blood vitamin C elevated with high dosing reduces the gradient. • Glutathione (GSH): GSH is a tripeptide composed of glycine, glutamic acid, and cysteine. It is in very high concentrations in lens. GSH is a key protective factor against intralenticular and extralenticular toxins and is an antioxidant. It maintains reduced sulfhydryl bonds within lens proteins. It is a coenzyme of various enzyme systems. GSH participates in amino acid transport with gamma-glutamyl transpeptidase. It also is involved in cation transport. GSH is diminished in virtually all forms of cataracts. • Ascorbic acid (AA) and GSH interactions: work in close conjunction as the most important host protective factor against induction of cataracts. • Selenium and vitamin E: antioxidants that function synergistically. GSH peroxidase is Se dependent. Se content in lens with cataract is 15% of normal. Se in serum and aqueous humor is much lower in cataract patients than in control subjects, but Se in the lens itself did not differ much in cataract patients and normal subjects. Decreased Se in aqueous humor is a major finding. Excess H2O2 (25 times normal) is in the aqueous humor of cataract patients and is associated with increased lipid peroxidation and altered lens permeability from damaged sodium-potassium pump. The lens is left unprotected against free radical and sun damage. Se-dependent GSH peroxidase breaks down H2O2. Vitamin E supplementation alone (500IU q.d.) does not retard progression of cataracts. Vitamin E (400IU) plus vitamin C (500 mg) and beta-carotene (15 mg) failed to affect the development or progression of cataracts in a 7-year trial. • Superoxide dismutase (SOD): activity in human lens is lower than in other tissues because of increased ascorbate and GSH. Progressive SOD decrease parallels cataract progression. Oral SOD supplements do not affect tissue SOD activity. Trace mineral cofactors of SOD that are greatly reduced in cataractous lens are preferred (copper, 90%; manganese, 50%; zinc, 90%). • Catalase: concentrated in epithelial portion of lens (anterior surface); very low levels are in the rest of lens. Primary function is to reduce (to water and oxygen) hydrogen peroxide formed from oxidation of ascorbate. • Tetrahydrobiopterin (BH4): pteridine compounds protect against cataract formation by preventing oxidation and damage by ultraviolet light. They prevent formation of high-molecular-weight proteins in lens. Tetrahydrobiopterin is a coenzyme in hydroxylation of monoamines (phenylalanine hydroxylase, tyrosine hydroxylase, tryptophan hydroxylase). Decreased pteridine-synthesizing enzymes and tetrahydrobiopterin are found in senile cataracts. Supplemental folic acid may help compensate.
Senile (Aging-Related) Cataracts
GENERAL CONSIDERATIONS
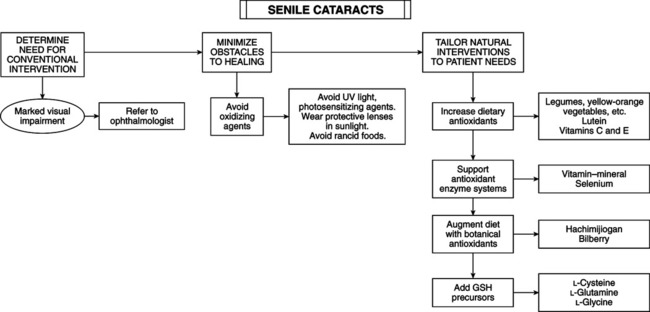
THERAPEUTIC CONSIDERATIONS
Antioxidants
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Senile (Aging-Related) Cataracts
