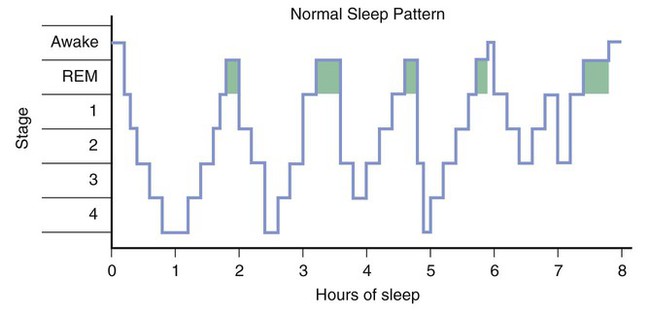
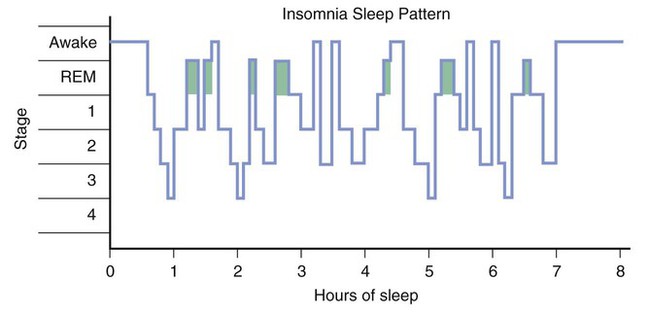
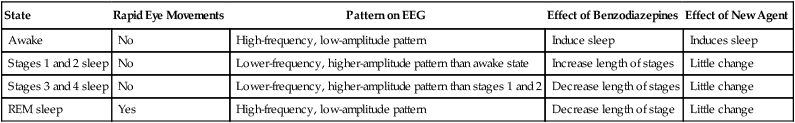
This chapter describes the pharmacologic properties of benzodiazepines, barbiturates, and other sedative-hypnotic and anxiolytic drugs that are used in the treatment of anxiety and sleep disorders. Because of their greater safety, fewer adverse effects, and the availability of an antagonist, the benzodiazepines have largely replaced the older barbiturates for these indications. Although ethanol (alcohol) has sedative-hypnotic effects, it is not used therapeutically for these purposes; its pharmacologic effects are described in Chapter 25. Panic disorder is characterized by acute episodes of severe anxiety with marked psychological and physiologic symptoms. During a panic attack, an individual may feel an impending sense of doom that is often accompanied by sweating, tachycardia, tremor, and other visceral symptoms. Patients with panic disorder often respond to drug therapy with a benzodiazepine or an antidepressant drug, such as a selective serotonin reuptake inhibitor (SSRI; see Chapter 22). Benzodiazepines may provide immediate relief from panic attacks during the early phase of therapy, and alprazolam and clonazepam are benzodiazepines that have been particularly useful in this regard. For long-term treatment, an SSRI antidepressant, such as fluoxetine, is often prescribed. Obsessive-compulsive disorder (OCD) is characterized by obsessions, which are recurring or persistent thoughts and impulses, and compulsions, defined as repetitive behaviors in response to obsessions. OCD can be treated effectively with an antidepressant drug (see Chapter 22) and psychotherapy. Generalized anxiety disorder (GAD) is characterized by chronic worry and apprehension concerning future events. Short-term therapy with a benzodiazepine may relieve acute symptoms and provide a useful bridge to psychotherapy. The severity of the disorder often fluctuates over time, and benzodiazepines may be effectively used on an intermittent basis to help patients deal with exacerbations of the disorder. Buspirone, a nonsedating anxiolytic, provides a useful alternative to benzodiazepines for the treatment of chronic anxiety states, because it produces little sedation and is not associated with tolerance or dependence. It must be taken for 3 or 4 weeks, however, before its anxiolytic effects are felt. SSRIs, such as paroxetine, and the serotonin and norepinephrine reuptake inhibitors (SNRIs) venlafaxine and duloxetine (see Chapter 22), are also used in the treatment of GAD. As an individual falls asleep, the high-frequency and low-amplitude activity of the alert state gradually diminishes during stages 1 and 2 and is replaced by the low-frequency and high-amplitude activity of slow-wave sleep (stages 3 and 4). Over time, the individual returns to stage 1 and eventually to the REM stage. REM sleep is also known as paradoxical sleep because the EEG pattern is similar to that in the awake state. A normal adult cycles through the sleep stages about every 90 minutes (Box 19-1). Sleep patterns change with age and are altered by sedative-hypnotic and other CNS drugs. Some patients with insomnia find it difficult to go to sleep or to stay asleep during the night, whereas others awaken too early in the morning. In general, the management of insomnia depends on whether the sleep disorder is caused by physiologic, psychological, or medical conditions. As shown in Box 19-1, the patterns of sleep stages in patients with insomnia are irregular and include longer latency to fall asleep and frequent awakenings. Other sleep disorders include hypersomnia (difficulty in awakening), narcolepsy (sleep attacks), enuresis (bedwetting during sleep), somnambulism (sleepwalking), sleep apnea (episodes of hypoventilation during sleep), and nightmares and night terrors. Most of these disorders are managed with a combination of psychotherapy and antidepressant drugs or CNS stimulants. Sodium oxybate (XYREM), a form of the abused drug γ-hydroxybutyrate, was recently approved for the treatment of cataplexy associated with narcoleptic attacks. CNS stimulants used to treat narcolepsy and other sleep disorders are discussed in Chapter 22. The sedative-hypnotic drugs include benzodiazepines, barbiturates, some antihistamines, and a few nonbenzodiazepine agents, such as zolpidem, zaleplon, eszopiclone, and ramelteon. The properties of these drugs are summarized in Table 19-1, and their adverse effects and drug interactions are listed in Table 19-2. TABLE 19-1 Pharmacokinetic Properties and Clinical Uses of Sedative-Hypnotic and Anxiolytic Drugs
Sedative-Hypnotic and Anxiolytic Drugs
Overview
Anxiety Disorders
Classification and Treatment of Anxiety Disorders
Panic Disorder
Obsessive-Compulsive Disorder
Generalized Anxiety Disorder
Sleep Disorders
Classification and Treatment of Sleep Disorders
Insomnia
Other Sleep Disorders
Sedative-Hypnotic Drugs
DRUG
ONSET OF ACTION*
DURATION OF ACTION*
ACTIVE METABOLITES
MAJOR CLINICAL USES
Benzodiazepines
Alprazolam
Fast
Medium
Yes
Anxiety, including panic disorder
Chlordiazepoxide
Fast; very fast (IV)
Long
Yes
Alcohol detoxification; anxiety
Clonazepam
Fast
Medium
No
Anxiety, including panic disorder; seizure disorders
Diazepam
Fast; very fast (IV)
Long
Yes
Alcohol detoxification; anxiety; muscle spasm; seizure disorders; spasticity
Estazolam
Fast
Medium
Yes
Insomnia
Flurazepam
Fast
Long
Yes
Insomnia
Lorazepam
Fast; very fast (IV)
Medium
No
Anxiety; seizure disorders
Midazolam
Very fast (IV)
Short (IV)
Yes
Anesthesia
Oxazepam
Fast
Short
No
Anxiety
Temazepam
Fast
Medium
No
Insomnia
Triazolam
Fast
Short
Yes
Insomnia
Barbiturates
Amobarbital
Fast
Medium
No
Insomnia
Pentobarbital
Fast
Short
No
Insomnia
Phenobarbital
Slow
Long
No
Seizure disorders
Thiopental
Very fast (IV)
Short (IV)
No
Induction of anesthesia
Antihistamines
Diphenhydramine
Fast
Medium
No
Insomnia
Hydroxyzine
Fast
Long
No
Anxiety; sedation
Other Sedative-Hypnotic Drugs
Zolpidem
Fast
Short
No
Insomnia
Zaleplon
Fast
Very short
No
Insomnia; midsleep awakenings
Eszopiclone
Fast
Short
No
Insomnia
Ramelteon
Slow
Short
Yes
Sleep-onset insomnia
Nonsedating Anxiolytic Drugs
Buspirone
Very slow
Long
No
Chronic anxiety
Propranolol
Fast
Medium
Yes
Situational or performance anxiety ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Sedative-Hypnotic and Anxiolytic Drugs
Only gold members can continue reading. Log In or Register to continue