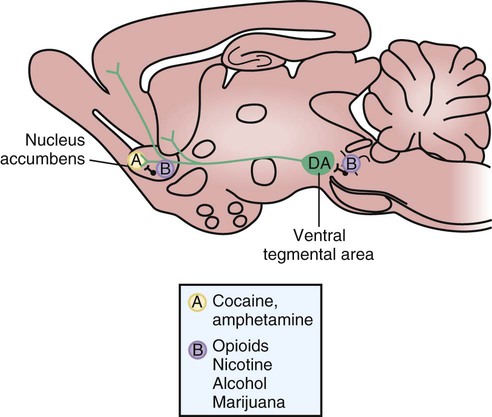
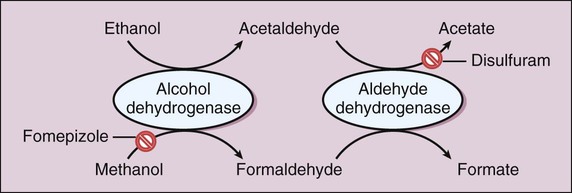
The peak of dopamine release in the nucleus accumbens occurs at the time of the drug’s peak effect on the central nervous system (CNS). The degree of short-term reinforcement of drug use is linked to the rate of increase of dopamine levels in the nucleus accumbens. This relationship appears to account for the propensity of some drugs to produce drug dependence. It also appears to explain the difference in reinforcement effects produced by different routes of administration of a particular drug. For example, the oral administration of an opioid or cocaine causes less reinforcement and psychological dependence than does the intravenous administration or inhalation of an equivalent dose of the same drug. The differences in effect are determined by the rate at which the drug is distributed to the brain and the rate at which dopamine levels in the nucleus accumbens are increased. Figure 25-1 illustrates the neuroanatomy and mechanisms of reinforcement for drugs of abuse. The psychoactive drugs that are used by some individuals for nonmedicinal purposes can be classified as CNS depressants, CNS stimulants, and miscellaneous agents, with the latter group including marijuana, hallucinogens, and phencyclidine (PCP). In many cases, individuals with a substance-abuse disorder are using legal or illegal substances as self-medication for comorbid disorders such as anxiety or depression. After describing the pharmacologic effects of these drugs and any clinical use that they may have, this chapter discusses the treatment of substance abuse. Tables 25-1, 25-2, and 25-3 provide information about the manifestations and treatment of drug intoxication and withdrawal. TABLE 25-1 Common Signs and Symptoms of Drug Intoxication TABLE 25-2 Emergency Treatment of Drug Intoxication TABLE 25-3 Common Signs and Symptoms of Drug Withdrawal *Because piloerection causes goose bumps or gooseflesh, patients withdrawing from opioids are sometimes described as “going cold turkey.” As shown in Figure 25-2, ethanol is primarily oxidized by alcohol dehydrogenase to form acetaldehyde and is then oxidized by acetaldehyde dehydrogenase to form acetate. The acetate derived from ethanol enters the citric acid cycle for further oxidation to carbon dioxide and water. The oxidation of ethanol uses significant quantities of nicotinamide adenine dinucleotide (NAD), and the depletion of NAD is responsible for some of the metabolic effects of ethanol that are described later. Ethanol at higher or chronic doses also undergoes oxidation by cytochrome P450 enzymes, namely the CYP2E1 isozyme. Unlike alcohol dehydrogenase metabolism, CYP2E1 metabolism is induced by long-term alcohol use, contributing to alcohol tolerance in heavy drinkers.
Drugs of Abuse
Overview
Drug Abuse
Drug Dependence
Psychological Dependence
Classification of Drugs of Abuse
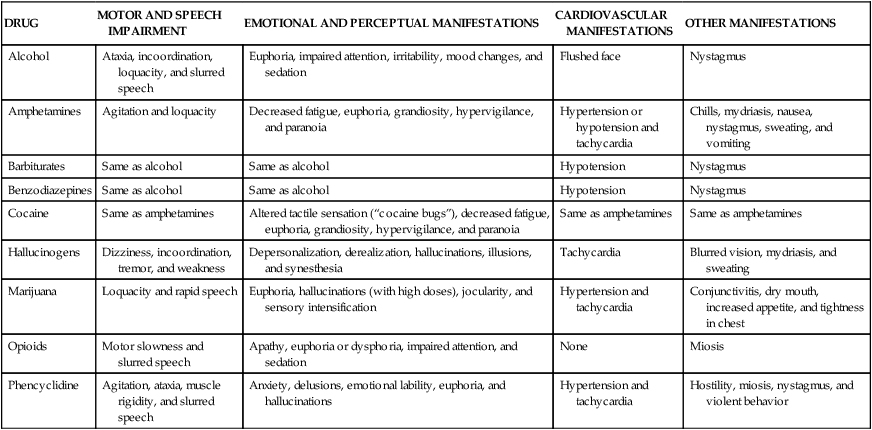
DRUG
MOTOR AND SPEECH IMPAIRMENT
EMOTIONAL AND PERCEPTUAL MANIFESTATIONS
CARDIOVASCULAR MANIFESTATIONS
OTHER MANIFESTATIONS
Alcohol
Ataxia, incoordination, loquacity, and slurred speech
Euphoria, impaired attention, irritability, mood changes, and sedation
Flushed face
Nystagmus
Amphetamines
Agitation and loquacity
Decreased fatigue, euphoria, grandiosity, hypervigilance, and paranoia
Hypertension or hypotension and tachycardia
Chills, mydriasis, nausea, nystagmus, sweating, and vomiting
Barbiturates
Same as alcohol
Same as alcohol
Hypotension
Nystagmus
Benzodiazepines
Same as alcohol
Same as alcohol
Hypotension
Nystagmus
Cocaine
Same as amphetamines
Altered tactile sensation (“cocaine bugs”), decreased fatigue, euphoria, grandiosity, hypervigilance, and paranoia
Same as amphetamines
Same as amphetamines
Hallucinogens
Dizziness, incoordination, tremor, and weakness
Depersonalization, derealization, hallucinations, illusions, and synesthesia
Tachycardia
Blurred vision, mydriasis, and sweating
Marijuana
Loquacity and rapid speech
Euphoria, hallucinations (with high doses), jocularity, and sensory intensification
Hypertension and tachycardia
Conjunctivitis, dry mouth, increased appetite, and tightness in chest
Opioids
Motor slowness and slurred speech
Apathy, euphoria or dysphoria, impaired attention, and sedation
None
Miosis
Phencyclidine
Agitation, ataxia, muscle rigidity, and slurred speech
Anxiety, delusions, emotional lability, euphoria, and hallucinations
Hypertension and tachycardia
Hostility, miosis, nystagmus, and violent behavior
DRUG
PHARMACOLOGIC TREATMENT
NONPHARMACOLOGIC TREATMENT
Alcohol
None
Support vital functions
Amphetamines
Lorazepam for agitation and haloperidol for psychosis
Monitor and support cardiac function
Barbiturates
None
Support vital functions
Benzodiazepines
Flumazenil
Support vital functions
Cocaine
Lorazepam for agitation or seizures
Support vital functions
Hallucinogens
Lorazepam for agitation
Give reassurance and support vital functions
Marijuana
Lorazepam for agitation
Give reassurance and support vital functions
Opioids
Naloxone
Support vital functions
Phencyclidine
Lorazepam for agitation and haloperidol for psychosis
Minimize sensory input
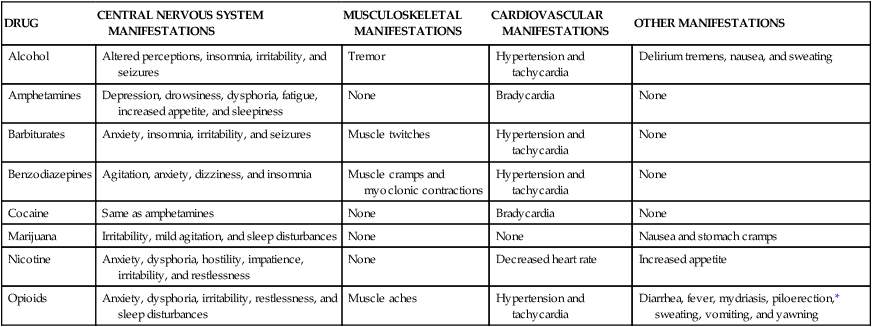
DRUG
CENTRAL NERVOUS SYSTEM MANIFESTATIONS
MUSCULOSKELETAL MANIFESTATIONS
CARDIOVASCULAR MANIFESTATIONS
OTHER MANIFESTATIONS
Alcohol
Altered perceptions, insomnia, irritability, and seizures
Tremor
Hypertension and tachycardia
Delirium tremens, nausea, and sweating
Amphetamines
Depression, drowsiness, dysphoria, fatigue, increased appetite, and sleepiness
None
Bradycardia
None
Barbiturates
Anxiety, insomnia, irritability, and seizures
Muscle twitches
Hypertension and tachycardia
None
Benzodiazepines
Agitation, anxiety, dizziness, and insomnia
Muscle cramps and myoclonic contractions
Hypertension and tachycardia
None
Cocaine
Same as amphetamines
None
Bradycardia
None
Marijuana
Irritability, mild agitation, and sleep disturbances
None
None
Nausea and stomach cramps
Nicotine
Anxiety, dysphoria, hostility, impatience, irritability, and restlessness
None
Decreased heart rate
Increased appetite
Opioids
Anxiety, dysphoria, irritability, restlessness, and sleep disturbances
Muscle aches
Hypertension and tachycardia
Diarrhea, fever, mydriasis, piloerection,* sweating, vomiting, and yawning
Central Nervous System Depressants
Alcohols and Glycols
Ethanol
Pharmacokinetics
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Drugs of Abuse
Only gold members can continue reading. Log In or Register to continue