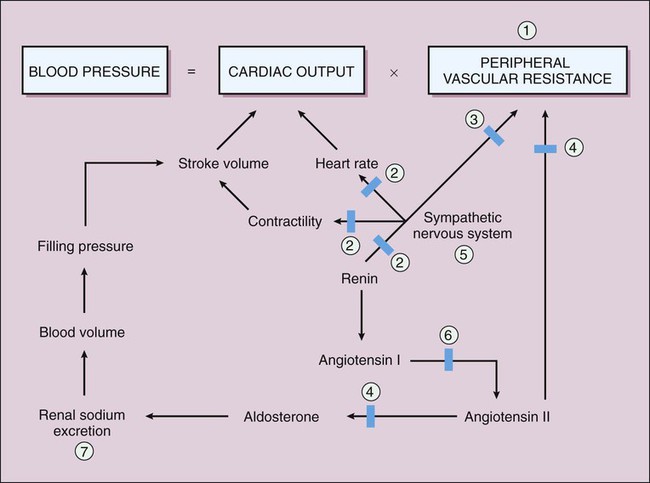
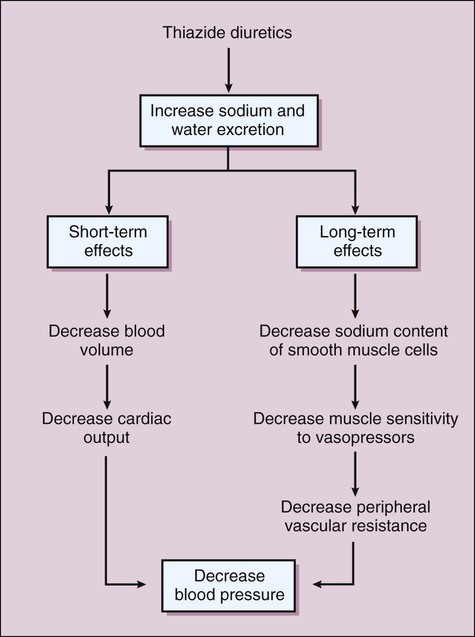
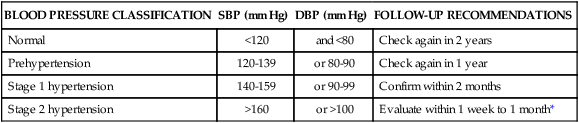
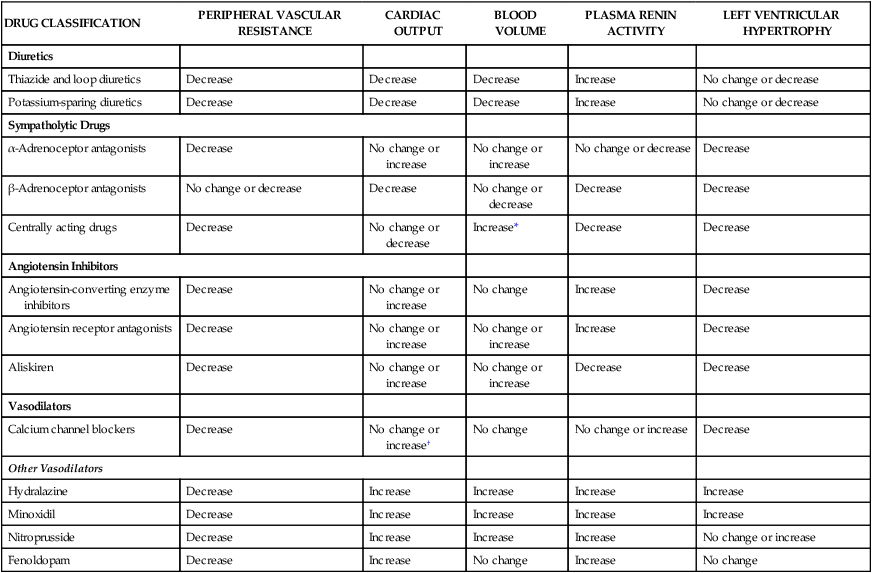
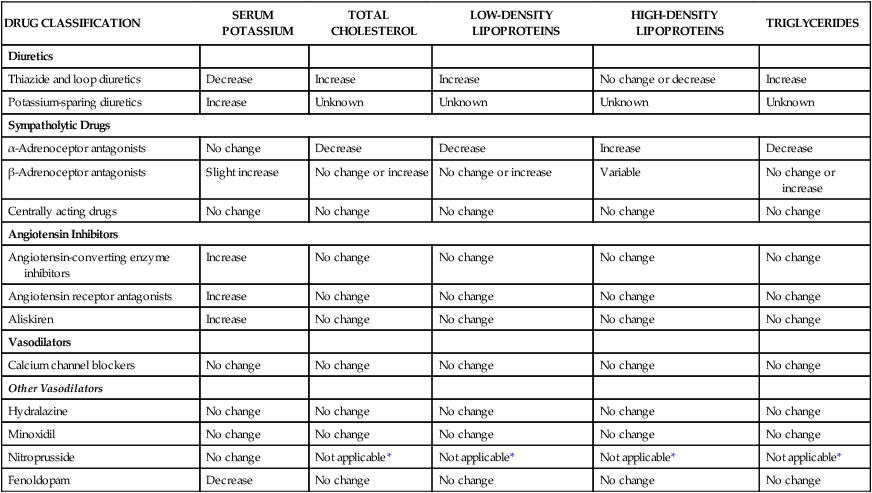
Blood pressure is classified as shown in Table 10-1. This classification uses the term prehypertension for those with blood pressures ranging from 120 to 139 mm Hg systolic, 80 to 89 mm Hg diastolic blood pressure, or both. This designation helps identify persons in whom early adoption of lifestyle changes that decrease blood pressure could prevent the progression of blood pressure to hypertensive levels (see later). These persons are not candidates for drug therapy unless they have diabetes and a trial of lifestyle changes fails to reduce their blood pressure to the desired level of 130/80 mm Hg or less for diabetics. TABLE 10-1 Classification of Blood Pressure for Adults and Follow-up Recommendations DBP, Diastolic blood pressure; SBP, systolic blood pressure. The four major categories of antihypertensive drugs are the diuretics, sympatholytic drugs, angiotensin inhibitors, and other vasodilators. These drugs lower blood pressure through actions exerted at one or more of the following sites: kidneys, sympathetic nervous system, renin-angiotensin-aldosterone axis, or vascular smooth muscle (Fig. 10-1). Antihypertensive drugs can be characterized in terms of their cardiovascular effects (Table 10-2) and their effects on serum potassium and cholesterol measurements (Table 10-3). They can also be characterized in terms of the compensatory mechanisms invoked by their hypotensive effect. Compensatory reactions serve to return blood pressure to the pretreatment level and include reflex tachycardia, fluid retention by the kidneys, and activation of the renin-angiotensin-aldosterone axis. Whereas most antihypertensive drugs are taken orally on a long-term basis, some are administered parenterally for the management of hypertensive emergencies. The treatment of this condition is discussed at the end of the chapter. TABLE 10-2 Cardiovascular Effects of Antihypertensive Drugs *An exception is guanfacine, which may cause no change in blood volume or decrease it slightly. †An exception is verapamil, which may increase or decrease cardiac output. TABLE 10-3 Pharmacologic Effects of Antihypertensive Drugs on Serum Potassium and Cholesterol Measurements *Nitroprusside is used only for short-term management of hypertension. Chapter 13 provides detailed information about the various classes of diuretics and their uses, mechanisms of action, and pharmacologic properties. The discussion here focuses on the diuretics most commonly used to treat hypertension: the thiazide and related diuretics, and the potassium-sparing diuretics. Thiazide and related diuretics reduce blood pressure by two mechanisms, both stemming from their ability to increase sodium and water excretion. When they are first administered to a patient, the drugs decrease blood volume and thereby decrease cardiac output (Fig. 10-2; see Table 10-2). With continued administration over weeks and months, they also decrease PVR, and this appears to account for much of their long-term antihypertensive effect. The decreased PVR may result from a reduction in the sodium content of arteriolar smooth muscle cells, which decreases muscle contraction in response to vasopressor agents such as norepinephrine and angiotensin. This relationship is supported by the finding that the effect of a thiazide on PVR is reduced if patients ingest enough dietary sodium to counteract the natriuretic effect of the drug.
Antihypertensive Drugs
Overview
Classification of Blood Pressure
BLOOD PRESSURE CLASSIFICATION
SBP (mm Hg)
DBP (mm Hg)
FOLLOW-UP RECOMMENDATIONS
Normal
<120
and <80
Check again in 2 years
Prehypertension
120-139
or 80-90
Check again in 1 year
Stage 1 hypertension
140-159
or 90-99
Confirm within 2 months
Stage 2 hypertension
>160
or >100
Evaluate within 1 week to 1 month*
Sites and Effects of Antihypertensive Drug Action
DRUG CLASSIFICATION
PERIPHERAL VASCULAR RESISTANCE
CARDIAC OUTPUT
BLOOD VOLUME
PLASMA RENIN ACTIVITY
LEFT VENTRICULAR HYPERTROPHY
Diuretics
Thiazide and loop diuretics
Decrease
Decrease
Decrease
Increase
No change or decrease
Potassium-sparing diuretics
Decrease
Decrease
Decrease
Increase
No change or decrease
Sympatholytic Drugs
α-Adrenoceptor antagonists
Decrease
No change or increase
No change or increase
No change or decrease
Decrease
β-Adrenoceptor antagonists
No change or decrease
Decrease
No change or decrease
Decrease
Decrease
Centrally acting drugs
Decrease
No change or decrease
Increase*
Decrease
Decrease
Angiotensin Inhibitors
Angiotensin-converting enzyme inhibitors
Decrease
No change or increase
No change
Increase
Decrease
Angiotensin receptor antagonists
Decrease
No change or increase
No change or increase
Increase
Decrease
Aliskiren
Decrease
No change or increase
No change or increase
Decrease
Decrease
Vasodilators
Calcium channel blockers
Decrease
No change or increase†
No change
No change or increase
Decrease
Other Vasodilators
Hydralazine
Decrease
Increase
Increase
Increase
Increase
Minoxidil
Decrease
Increase
Increase
Increase
Increase
Nitroprusside
Decrease
Increase
Increase
Increase
No change or increase
Fenoldopam
Decrease
Increase
No change
Increase
No change
DRUG CLASSIFICATION
SERUM POTASSIUM
TOTAL CHOLESTEROL
LOW-DENSITY LIPOPROTEINS
HIGH-DENSITY LIPOPROTEINS
TRIGLYCERIDES
Diuretics
Thiazide and loop diuretics
Decrease
Increase
Increase
No change or decrease
Increase
Potassium-sparing diuretics
Increase
Unknown
Unknown
Unknown
Unknown
Sympatholytic Drugs
α-Adrenoceptor antagonists
No change
Decrease
Decrease
Increase
Decrease
β-Adrenoceptor antagonists
Slight increase
No change or increase
No change or increase
Variable
No change or increase
Centrally acting drugs
No change
No change
No change
No change
No change
Angiotensin Inhibitors
Angiotensin-converting enzyme inhibitors
Increase
No change
No change
No change
No change
Angiotensin receptor antagonists
Increase
No change
No change
No change
No change
Aliskiren
Increase
No change
No change
No change
No change
Vasodilators
Calcium channel blockers
No change
No change
No change
No change
No change
Other Vasodilators
Hydralazine
No change
No change
No change
No change
No change
Minoxidil
No change
No change
No change
No change
No change
Nitroprusside
No change
Not applicable*
Not applicable*
Not applicable*
Not applicable*
Fenoldopam
Decrease
No change
No change
No change
No change
Diuretics
Thiazide and Related Diuretics
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Antihypertensive Drugs
Only gold members can continue reading. Log In or Register to continue