http://evolve.elsevier.com/McCuistion/pharmacology
According to the Institute for Healthcare Informatics, spending on prescription medicines increased by 10.3% in the United States during 2014. A total of $373.9 billion is spent on prescription medications yearly. In 2014, over 4.3 billion prescriptions were filled in the United States. Recently, the Journal of Patient Safety published a study that concluded that as many as 440,000 people die each year from preventable medical errors.
The focus of this chapter is quality and safety. It involves a discussion of safety initiatives and interventions that include the “five-plus-five” rights of medication administration, the nurse’s rights when administering medications, the culture of safety, and The Joint Commission (TJC) Patient Safety Goals. Also included are high-alert drugs, look-alike and sound-alike drugs, and dosage forms to crush or not to crush. (See Chapter 8, which reviews the Quality and Safety Education for Nurses [QSEN] initiatives from www.qsen.org.)
“Five-Plus-Five” Rights of Medication Administration
The “five-plus-five” rights of medication administration are important goals for medication safety. The nurse following these guidelines will give (1) the right patient (2) the right drug in (3) the right dose via (4) the right route at (5) the right time. The “plus five” refers to the five additional rights that have been recommended: (1) right assessment, (2) right documentation, (3) the patient’s right to education, (4) right evaluation, and (5) the patient’s right to refuse. The original five rights and the subsequent additions are important; however, additional interventions are necessary to ensure the patient’s positive response to the administered drug. Although nurses work together with health care providers and pharmacists to provide safe medication practices, it is the nurse who works closely with the patient and follows the patient’s response to the medication. The rights and interventions necessary for safe drug administration will be reviewed in this chapter.
Right Patient
The right patient determination is essential. TJC requires two forms of identification before drug administration.
• Ask the patient to state his or her full name and birth date, and compare these with the patient’s identification (ID) band and the medication administration record (MAR).
• Many facilities have electronic health records (EHRs) that allow the nurse to directly scan the bar code from the patient’s ID band. Once the band is scanned, the nurse can see the patient’s medication record.
Additional nursing implications include the following:
• Most hospitals have color-coded ID bands that include bands coded for allergy, do not resuscitate (DNR), fall risk, and restricted extremity. Always check facility policies for the use of color-coded bands and their meanings.
• Verify the patient’s identification each time a medication is given.
• If the patient is an adult with a cognitive disorder or a child, verify the patient’s name with a family member. In the event a family member is unavailable and the patient is unable to self-identify, follow the facility’s policy. Many facilities have policies that include a photo ID on the band with the patient’s name and birth date affixed to the band.
• Distinguish between two patients with the same first or last name by placing “name-alert” stickers as warnings on the medical records.
Right Drug
The nurse must accurately determine the right drug prior to administration. When working with an EHR, once the bar code on the patient’s wristband has been scanned, the patient’s drug profile will appear on the computer screen. The nurse will then scan the patient’s medication label, and it will automatically validate the time, date, and the nurse administering the patient’s medication. If it is not the correct medication, the nurse will receive an alert and will be unable to proceed in the MAR until the correct medication is scanned.
Both federal and state legislation governs who can write a prescription order. Medication orders are prescribed by a licensed health care provider (HCP) under authority from the state to prescribe drugs. Those disciplines that have prescriptive authority are medical doctor (MD), dentist (doctor of dental surgery [DDS]), podiatrist (doctor of podiatric medicine [DPM]), certified nurse practitioner (CNP), advanced practice registered nurse (APRN), physician assistant (PA), veterinarian, chiropractor, and optometrist. In addition, medical clinical psychiatrists and pharmacists have prescriptive authority with strict guidelines set by the state. Prescriptions may be handwritten by the HCP, delivered as a telephone order (T/O) or verbal order (V/O), or directly entered into the patient’s EHR. Handwritten prescriptions are written on a provider’s legal prescription pad and are filled by a pharmacist.
Sometimes providers order medications by directly speaking to the nurse. All telephone orders or verbal orders for medications are either handwritten by the nurse taking the order or entered directly into a computer and “read back” to ensure accuracy. The nurse will write the name of the prescribing provider and will include that the order was read back, and affixing his or her signature to the order will complete it. After dictating a verbal order, the provider must sign it within 24 hours. If the order is a controlled medication, most facilities require two licensed nurses to listen to the order and sign it. Nursing students are not allowed to accept or take provider orders, but they may administer the medication after it has been verified by a registered nurse.
Many hospitals are implementing computerized physician order entry (CPOE) systems to handle HCP medication orders. This method of ordering medications can help decrease drug errors by decreasing transcription errors. HCPs using a CPOE will directly input the prescription into the patient’s EHR; the order is electronically signed by the HCP and is sent directly to the pharmacy, and it is recorded as part of the patient’s MAR. A strong safety feature is the ability to identify drug interactions with the patient’s current drugs and any newly prescribed medications.
The use of computerized ordering systems has added speed and a measure of safety to the order process. Orders can be written from virtually any location and can be sent electronically, but the computer will not process the order unless all necessary information is included. Because the order is computerized, illegible orders or signatures are prevented. Before the nurse can administer the medication, both the pharmacy and the nurse must validate the accuracy of the patient’s prescription order in the EHR.
The components of a drug order are as follows (Fig. 9.1):
• Patient name and birth date
• Date the order is written
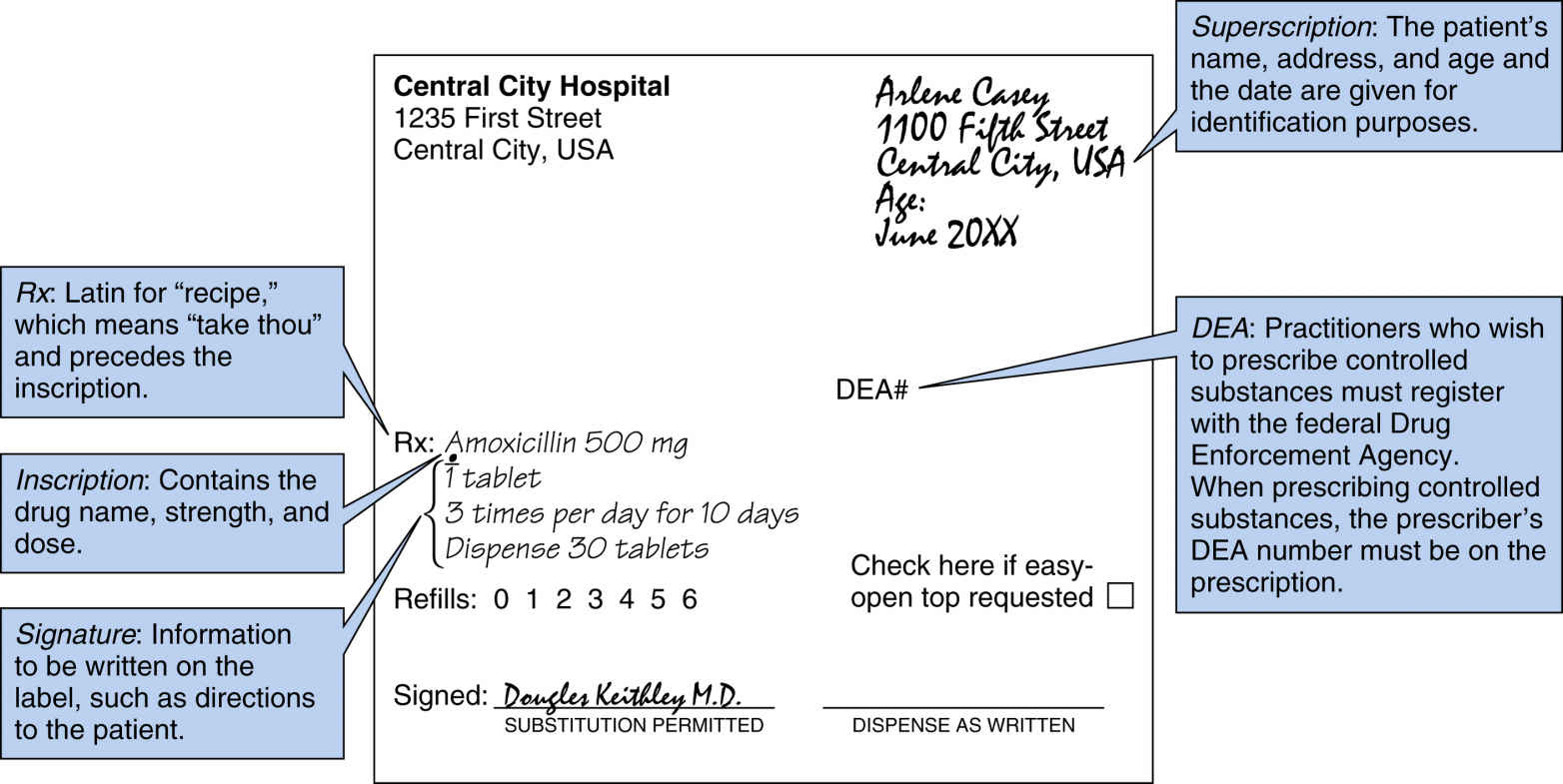
FIG. 9.1 Example of a Drug Order.
From Medical School Headquarters. (n.d.) Prescription writing 101. Retrieved from http://medicalschoolhq.net/prescription-writing-101
• Signature of licensed staff who took the T/O or V/O, if applicable
• HCPs who wish to prescribe controlled drugs must register with the federal Drug Enforcement Agency (DEA). When prescribing controlled substances, the HCP’s DEA number must be on the prescription.
• Drug name and strength
• Drug frequency or dose (e.g., once daily)
• Route of administration
• Duration of administration (e.g., × 7 days, × 3 doses, when applicable)
• Number of patient refills
• Number of pills to be dispensed
• Any special instructions for withholding or adjusting dosage based on nursing assessment, drug effectiveness, or laboratory results
It is the nurse’s responsibility to administer the drug as ordered by the provider, and if the drug order is incomplete, the drug should not be administered. Verification of a questionable order must be done in a timely manner. The HCP is usually contacted, and the conversation is documented. Nurses must become familiar with the components of a drug order and must question any incomplete or unclear orders. Nurses are legally liable if they give a prescribed drug and the dosage is incorrect, or if the drug is contraindicated for the patient’s health status. Once the drug has been administered, the nurse becomes liable for the predicted effects of that drug.
Medication administration is never considered just a process of “passing” drugs. Nurses must use critical thinking skills and assess whether the medication is correct for the patient’s diagnosis. The nurse must ask critical questions: Is the dose appropriate? What is the patient’s expected response? Also, the nurse must teach the patient about the drug’s side effects and when it is necessary for the patient to notify the HCP.
To avoid drug errors, the drug label should be read three times: (1) when you pick up the medication and remove it from the drug cabinet, (2) as you prepare the drug for administration, and (3) when you administer the drug.
Nursing interventions related to drug orders can ensure correct administration of medications:
• The nurse should verify the identity of the patient by comparing the name on the wristband with the name on the MAR for accuracy.
• Always use two patient identifiers, such as having patients repeat their name and date of birth.
• The nurse should be familiar with the patient’s health history and should have performed a head-to-toe assessment on the patient, including a complete set of vital signs.
• Always review the patient’s lab work prior to the administration of drugs.
• Read the drug order carefully. If the order is unclear, verify it with the HCP before administering the drug.
• Know the patient’s allergies.
• Know the reason the patient is to receive the medication.
• Check the drug label by identifying the drug name, the amount of the drug (tablet or volume), and its suitability for administration by the intended route.
• Check the dosage calculations.
• Know the date the medication was ordered and any ending date (e.g., for controlled substances and antibiotics and for limited or a specific number of doses). Some agencies have automatic stop orders that are generally facility specific. Examples of such orders include controlled drugs that need to be renewed every 48 hours, antibiotics to be renewed every 7 to 14 days, and cancellation of all medications when the patient goes to surgery.
• All orders—including first-dose, one-time, and as-needed (PRN) medication orders—should be checked against the original orders.
Right Dose
The right dose refers to verification by the nurse that the dose administered is the amount ordered and that it is safe for the patient for whom it is prescribed. The right dose is based on the patient’s physical status. Many medications require the patient’s weight in order to determine the right dose. Usually pediatrics, medical-surgical, and critical care situations require weight to complete the drug calculation and determine the correct dose (heparin and digoxin drip are examples of medications calculated according to weight). The nurse determines if the drug is safe to administer according to the drug’s pharmacodynamics (action) and the patient’s vital signs. Renal and hepatic functions are important considerations because many drugs are cleared through the kidneys and metabolized by the liver. Prior to drug administration, it is important that the nurse carefully review the patient’s most current lab results. A chemistry panel includes renal and liver function and sodium and potassium levels. Also, the nurse should review the hematology labs, which include a complete blood count (CBC), red blood cells (RBCs), hemoglobin, hematocrit, and platelets. It is most important that the nurse check the drug’s correct dose range in a reliable drug resource book or by consulting with a pharmacist. In most cases, the right dose for a specific patient is within the recommended range for the particular drug. Nurses must calculate each drug dose accurately.
Nurses use dimensional analysis or ratio and proportion when calculating a drug dose (see Chapter 11). Always recheck the drug calculation if the dose is within a fraction or if it is an extremely large dose. Consult another nurse or the pharmacist when in doubt.
Today, most drugs are dispensed through automated dispensing cabinets (ADCs), computerized drug storage cabinets that store and dispense medications near the point of care while controlling and tracking drug distribution. The patient’s drugs are stocked in the cabinet by the pharmacist and are accessed under the patient’s name, and the nurse is able to select and pull the patient’s drugs from the cabinet. This technology improves patient care by promoting accurate and quick access to medications, locked storage for all medications, and electronic tracking for controlled substances. Automation of drug administration saves time and decreases costs associated with drug administration.
Another method of dispensing drugs is the unit dose method, in which drugs are individually wrapped and labeled for single-dose use for each patient. The unit dose method has reduced dosage errors because no calculations are required. Some facilities still use a multidose vial from the ADC. If this occurs, the nurse will have to complete a calculation in order to retrieve the correct amount ordered by the physician from the vial. If there is any medication left in the vial, it is disposed of according to the facility’s policy for disposal of drugs.
An important nursing intervention related to the right dose includes calculating the drug dose correctly. If in doubt about the amount to be administered, consult with a nurse peer to validate the correct amount. In some settings, two registered nurses (RNs) are required to check the dosage for certain medications, such as insulin and heparin.
Right Time
The right time refers to the time the prescribed dose is ordered to be administered. Daily drug dosages are given at specified intervals, such as twice a day (bid), three times a day (tid), four times a day (qid), or every 6 hours (every 6hrs); this is so the plasma level of the drug is maintained at a therapeutic level. Every drug cannot be given exactly when ordered, therefore health care agencies have policies that specify a range of times within which drugs can be administered (check your agency’s policy). When a drug has a long half-life, it is usually given once a day. Drugs with a short half-life are given several times a day at specified intervals. Some drugs are given before meals, whereas others must be given with meals.
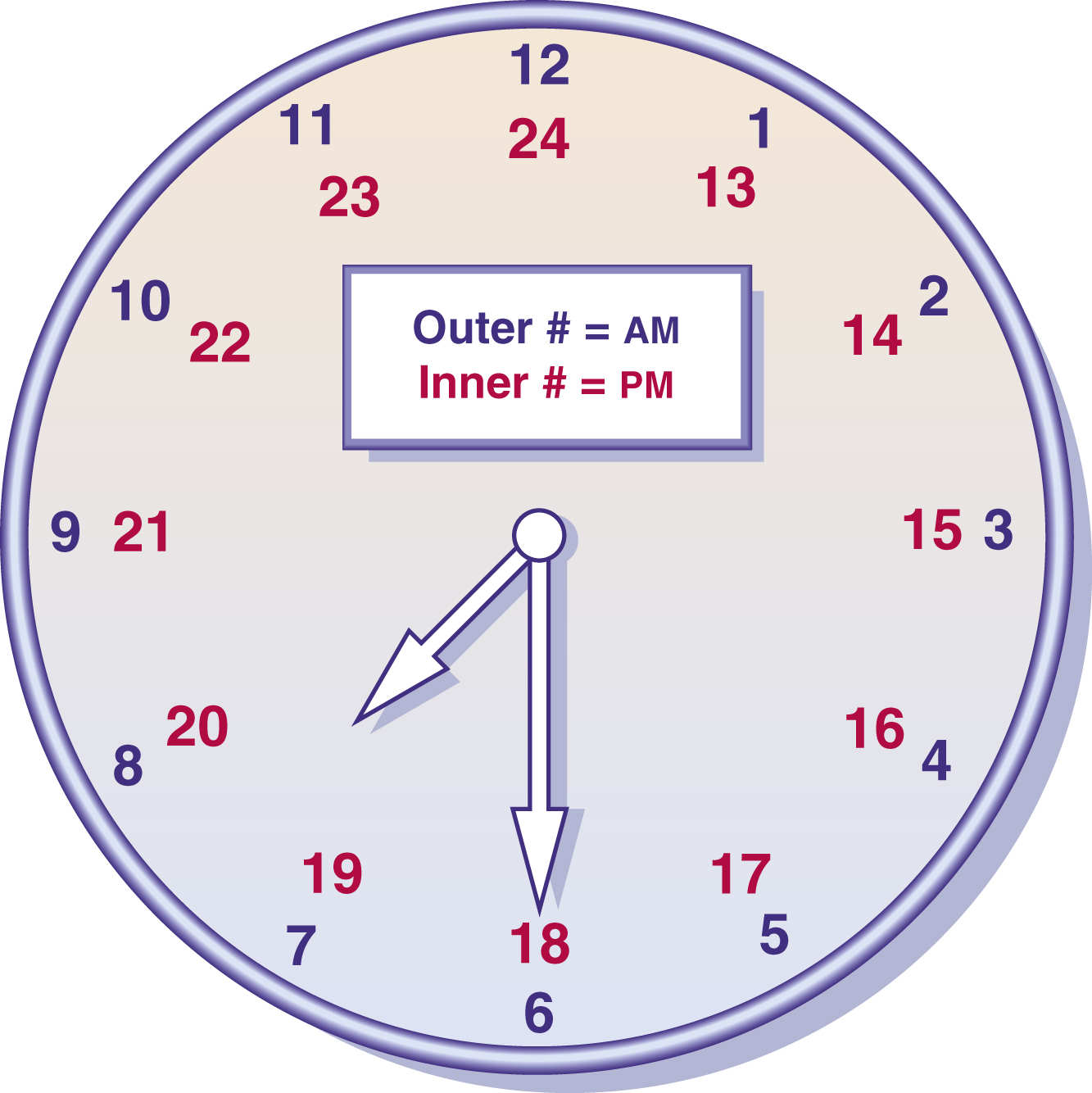
Use of military time, which is based on a 24-hour clock (Fig. 9.2), reduces administration errors and decreases documentation. Many nursing settings use military time rather than standard time. Nursing interventions related to the right time include the following:
• Administer drugs at the specified times (refer to agency policy).
• Administer drugs that are affected by food, such as tetracycline, 1 hour before or 2 hours after meals.
• Give food with drugs that can irritate the stomach (gastric mucosa)—for example, potassium and aspirin. Some medications are absorbed better after eating.
• Adjust the medication schedule to fit the patient’s lifestyle, activities, tolerances, or preferences as much as possible.
• Check whether the patient is scheduled for any diagnostic procedures that contraindicate the administration of medications, such as endoscopy or fasting blood tests. Determine whether the medication should be given before or after the test based on the policy.
• Check the expiration date. If the date has passed, discard the medication or return it to the pharmacy, depending on the policy.
• Patients who require dialysis usually have blood pressure medications stopped prior to dialysis because dialysis can decrease blood pressure. However, some doctors order the medications to be given prior to dialysis. If any questions arise, check with the HCP before proceeding.
Right Route
The right route is necessary for adequate or appropriate absorption. The right route is ordered by the health care provider and indicates the mechanism by which the medication enters the body. The more common routes of absorption include oral, with drug in the form of a liquid, elixir, suspension, pill, tablet, or capsule; sublingual, under the tongue for venous absorption; buccal, between the cheek and gum; via a feeding tube; topical, applied to the skin; by inhalation (aerosol sprays); via otic (eye), ophthalmic (ear), or nasal (spray) instillation; by suppository (rectal or vaginal); and through the five parenteral routes: (1) intradermal, (2) subcutaneous (subcut), (3) intramuscular (IM), (4) intravenous (IV), or (5) intraosseous (IO).
Nursing interventions related to the right route include the following:
• Assess the patient’s ability to swallow before administering oral medications; make sure the patient has not been ordered nothing by mouth (NPO).
• Do not crush or mix medications in other substances without consulting a pharmacist or a reliable drug reference. Do not mix medications in an infant’s formula feeding.
• If the medication must be mixed with another substance, explain this to the patient. For example, elderly patients may use applesauce or yogurt to mix their medications to make them easier to swallow. Medications should be administered one at a time in the substance.
• Best Practice Guidelines and TJC state that drugs must be identifiable up until the point of delivery. When administering many drugs at one time, it is not recommended to mix drugs together. The correct practice is to administer one pill at a time. When a patient has an enteral tube, it is important to follow these guidelines; this allows the nurse to flush the tube before and after each pill or liquid is administered to prevent the tube from clogging. In the event that a patient’s drug inadvertently falls to the ground, the nurse will be able to identify, discard, and replace the pill.
• Instruct the patient that medications must be swallowed with water and not juice, which can interfere with the absorption of certain medications; however, it is recommended that iron be taken with orange juice or vitamin C supplements to aid in the absorption of the iron.
• Use aseptic technique when administering drugs. Sterile technique is required with the parenteral routes.
• Administer drugs at the appropriate sites for the route.
• Stay with the patient until oral drugs have been swallowed.
Right Assessment
The right assessment requires the collection of appropriate baseline data before administration of a drug. Examples of assessment data include taking a complete set of vital signs and checking lab levels prior to drug administration. This may also include both apical heart rate and potassium level prior to administering digitalis; blood pressure level prior to administering an antihypertensive drug; blood glucose levels before insulin administration; or respirations with blood pressure prior to administering an opioid. It is also important for the nurse to identify high-risk patients, such as patients with medication allergies, patients on dialysis, those with liver disease, diabetic patients, cardiac and pulmonary patients, and the elderly and pediatric populations. If at-risk patients are identified, precautions can be taken to reduce risk.
Right Documentation
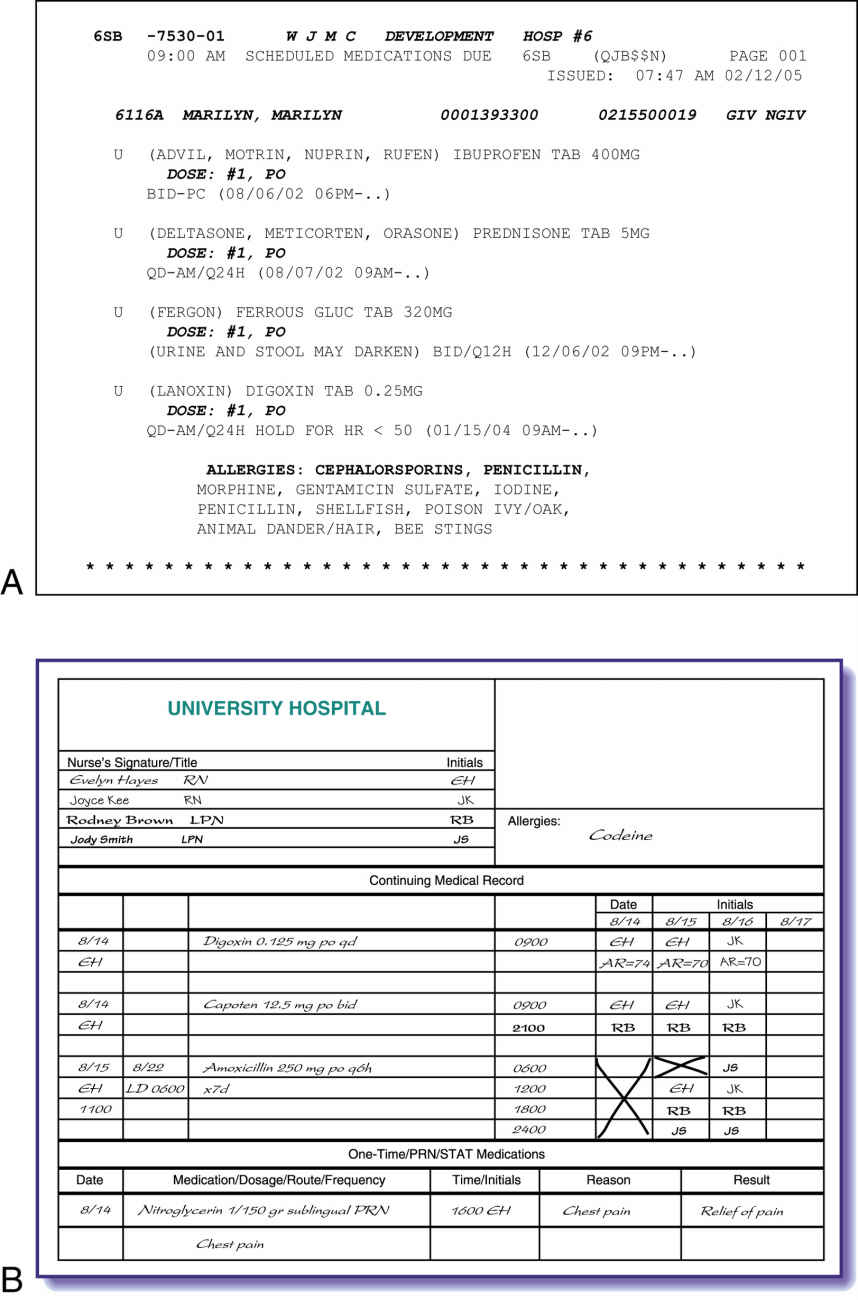
The right documentation requires the nurse to record immediately the appropriate information about the drug administered. Many systems are available for documenting drug administration. The most common is the paper medication administration record (MAR), which the pharmacy will furnish. Facility policies vary, but when nurses administer a drug, they place their initials next to the name of the drug on the paper MAR. The nurse’s initials verify that the medication was administered. Both paper and computerized MARs include information about the drug to be administered, including (1) the name of the drug, (2) the dose, (3) the route, (4) the time and date, and (5) the nurse’s initials or signature.
Now popular and becoming common in most facilities is computerized charting, in which the nurse enters a personal identification and password to gain entry into the system. By scanning the patient’s identification band (Fig. 9.3), which includes the patient’s bar code information, the nurse accesses the patient’s personal MAR with the emergency medical record (EMR) system. Once the nurse scans the bar code on the patient’s medication package, the administration is validated in the computerized MAR. The computerized system interfaces with other departments, including the pharmacy, laboratory, and sometimes the physician’s office.
Documentation of the patient’s response to the medication is required with a variety of medications such as (1) opioid and nonopioid analgesics (Ask, how effective was pain relief?); (2) sedatives (How effective was relaxation?); and (3) antiemetics (Was nausea/vomiting decreased or eliminated?). The nurse continues to assess the patient’s response to the medication (Was there any gastrointestinal irritation or skin sensitivity?) and documents this in the patient’s plan of care. Keep in mind that patient responses are not necessarily verbal; they could be physiologic (e.g., blood pressure decreasing in response to an antihypertensive). With the paper MAR and a pen, the nurse documents the response in the nursing notes. The computerized MAR allows for documentation of the patient’s response directly into the plan of care. Delay in charting may result in forgetting to chart the medication, and another nurse can inadvertently administer the drug, assuming it was not given because it was not charted. Therefore it is important to remember that drugs must be signed off on when the drug is administered. Graphic formats or computerized systems (Fig. 9.4) assist in the accurate and timely recording of drugs administered.
Right to Education
The right to education requires that patients receive accurate and thorough information about the drugs they are taking and how each drug relates to their particular condition. Patient teaching also includes why the patient is taking the drug, the expected result of the drug, possible side effects of the drug, any dietary restrictions or requirements, skill of administration with return demonstration, and laboratory test result monitoring. This right is a principle of informed consent, which is the individual having the necessary knowledge to make a decision. Informed patients and families are critical to preventing medication errors.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree