Respiratory System Disorders
Learning Objectives
After studying this chapter, the student is expected to:
1. Describe the common upper respiratory tract infections.
2. Explain how secondary bacterial infections occur in the respiratory tract.
3. Compare the different types of pneumonia.
4. Differentiate the effects of primary from secondary tuberculosis.
5. Describe the pathophysiology and complications of cystic fibrosis.
6. Describe the etiology and pathophysiology of bronchogenic carcinoma.
7. Describe the possible outcomes of aspiration.
8. Compare the types of asthma and describe the pathophysiology and manifestations of an acute attack.
9. Compare emphysema and chronic bronchitis.
10. Explain how bronchiectasis develops as a secondary problem and also its manifestations.
11. Describe the causes of pulmonary edema and explain how it affects oxygen levels.
12. Compare the effects of small, moderate, and large-sized pulmonary emboli.
13. Describe the causes of atelectasis and the resulting effects on ventilation and oxygen levels.
14. Explain the effects of pleural effusion on ventilation.
15. Compare the types of pneumothorax.
16. Explain how a flail chest injury affects ventilation, oxygen levels, and circulation.
17. Describe the pathophysiology and signs of infant respiratory distress syndrome.
18. Describe the possible causes of adult respiratory distress syndrome and the pathophysiology.
19. Describe the etiology and changes in blood gases with acute respiratory failure.
20. Explain the cause of sleep apnea and describe the effects and complications of this disorder.
Key Terms
apnea
bifurcation
bronchodilation
caseation
clubbing
cohesion
empyema
eupnea
expectorant
hemoptysis
hypercapnia
hypoxemia
paroxysmal nocturnal dyspnea
proteases
pulsus paradoxus
rales
rhonchi
sputum
steatorrhea
stridor
surface tension
wheezing
Review of Structures of the Respiratory System
Purpose and General Organization
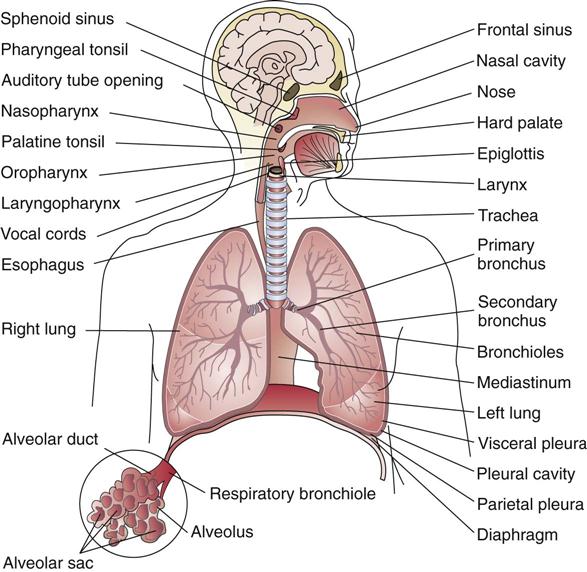
The respiratory system provides the mechanisms for transporting oxygen from the air into the blood and for removing carbon dioxide from the blood. Oxygen is essential for cell metabolism, and the respiratory system is the only means of acquiring oxygen. Carbon dioxide is a waste material resulting from cell metabolism, and it influences the acid-base balance in body fluids.
The respiratory system consists of two anatomic areas. The upper respiratory tract is made up of the passageways that conduct air between the atmosphere and the lungs, and the lower respiratory tract consists of the trachea, bronchial tree, and the lungs, where gas exchange takes place. In addition, the pulmonary circulation, the muscles required for ventilation, and the nervous system, which plays a role in controlling respiratory function, are integral to the function of the respiratory system.
Structures in the Respiratory System
The Upper Respiratory Tract
When air is inhaled into the respiratory system, it first enters the nasal passages, passing over the conchae or turbinates, where it is warmed and moistened by the highly vascular mucosa. Foreign material is filtered out by the mucous secretions and hairs before the air enters the delicate lung tissue. Opening off the nasal cavity through small canals are four pairs of paranasal sinuses, which are small cavities in the skull bones (Fig. 13-1). The presence of the hollow sinuses reduces the weight of the facial bones and adds resonance to the voice. They are named according to the bones in which they are located—the frontal, ethmoid, sphenoid, and maxillary sinuses.
The sinuses are lined by a continuation of the respiratory mucosa. The respiratory mucosa consists of pseudostratified ciliated columnar epithelium, which includes mucus-secreting goblet cells. The resultant mucous blanket “traps” foreign particles, and the cilia “sweep” the mucus and debris up and out of the respiratory tract. This process is referred to as “ciliary escalator.” Excessive amounts of mucus or particles stimulate a sneeze or a cough, which assists in expelling unwanted material away from the lungs. Smoking impairs the function of the cilia, and the irritation caused by smoke leads to replacement of ciliated epithelium by squamous cells, thereby removing this protective mechanism.
The airflow continues through the nasopharynx and larynx into the trachea. On the posterior wall of the nasopharynx are located the pharyngeal tonsils or adenoids, which consist of lymphoid tissue, another defense against the inhalation of foreign material. If these tonsils become enlarged owing to infection, they can obstruct the flow of air through the nasopharynx, leading to mouth breathing. When air passes through the mouth directly into the respiratory tract, it is not warmed, moistened, and filtered properly before it reaches the delicate lung tissue. The tissues of the mouth become dry and irritated, and there is a risk of increased dental caries as normal salivary cleansing function is lost. The palatine tonsils, popularly called the tonsils, are lymphoid tissue located in the posterior portion of the oral cavity (see Fig. 17-2 in Chapter 17). Also opening off the nasopharynx are the two auditory (eustachian) tubes, which connect to the middle ear cavities. The continuation of the respiratory mucosa into the sinuses and middle ear creates a predisposition to the spread of infection from the upper respiratory tract. The upper respiratory tract has a resident flora, whereas the lungs are sterile, containing no microorganisms.
The pharynx, where the nasopharynx joins the oropharynx, serves as a common passage for air and food and descends to the point of separation of the esophagus and trachea. When infection is present, the inflammation and swelling in the area causes sore throat and painful swallowing. In the airway, the cartilaginous epiglottis protects the opening into the larynx, or voice box, by flipping up or down during swallowing or ventilation.
The larynx consists of various cartilages and their associated muscles. The largest is the thyroid cartilage, which forms the “Adam’s apple,” a structure that may protrude in the anterior neck area. There are two pairs of vocal cords, which are infoldings of the mucous membrane: the upper, or “false,” pair, and the lower pair, comprising the true vocal cords. The glottis refers to the true vocal cords and the space between them. When air is expired through the larynx, the true vocal cords vibrate, producing the sound of the voice. Other structures affect the characteristics of this sound, including the mouth, tongue, pharynx, and sinuses. The vocal cords, when approximated, prevent food from entering the trachea and lungs.
As inspired air is tracked downward through the larynx, it flows into the trachea, or windpipe. The wall of the trachea contains 16 to 20 hyaline cartilage rings, fibroelastic tissue, and smooth muscle tissue. The trachea is flexible enough to allow bending and elongation. The cartilage rings prevent the collapse of the trachea and keep the airway open even with the pressure changes. The posterior wall of the trachea is not rigid, thus allowing the esophagus to expand as swallowed food moves through it.
The Lower Respiratory Tract
At the lower end of the trachea, inhaled air proceeds into the right or left primary bronchus. The right bronchus is larger and straighter and therefore is the more likely destination for any aspirated material. The point at which the bronchus enters the lung is the hilum. Each major or primary bronchus then branches into many smaller (secondary) bronchi and then into bronchioles, forming an inverted bronchial “tree.” As the bronchi become smaller, the cartilaginous rings are replaced by irregular plates of cartilage. As the bronchi divide into bronchioles, supportive cartilage is no longer present. The smooth muscle contracts or relaxes to adjust the diameter of the bronchioles. Bronchodilation results when sympathetic stimulation relaxes the smooth muscle, dilating or enlarging the bronchioles. Many elastic fibers are present in the lung tissue, enabling the expansion and recoil of the lungs during ventilation. The respiratory mucosa thins and changes from pseudostratified columnar to simple columnar and then to simple cuboidal epithelium in the terminal and respiratory bronchioles.
Air in the bronchioles then flows into the alveolar ducts and alveoli, or air sacs, which resemble a cluster of grapes. The alveoli are formed by a single layer of simple squamous epithelial tissue, which promotes the diffusion of gases into the blood, the end-point for inspired air (see Fig. 13-5). The respiratory membrane is the combined alveolar and capillary wall, a very thin membrane, through which gas exchange takes place. There are millions of alveoli, and the capillaries of the pulmonary circulation are in close contact, providing a very large surface area for the diffusion of gases. The alveoli contain macrophages (alveolar macrophages), whose function is to remove any foreign material that penetrates to this level. However some substances can escape any action by macrophages.
The inside surfaces of the alveoli are coated with a very small amount of fluid containing surfactant, produced by specialized cells in the alveolar wall. Surfactant has a detergent action that reduces surface tension of the alveolar fluid (the tendency for fluid to reduce its surface area by forming droplets), facilitating inspiration and preventing total collapse of the alveoli during expiration. When inspiration is complete, the process of expiration reverses airflow in the passageways, forcing air out of the alveoli and up the bronchi, trachea, and nose.
The lungs are cone-shaped structures positioned on either side of the heart. The mediastinum is the region in the center of the chest, which contains the heart, the major blood vessels, the esophagus, and the trachea. The dome-shaped muscular diaphragm forms the inferior boundary. The right lung is divided into three lobes and the left lung into two lobes because of the position of the heart, and each lobe is then divided into segments. The lung tissue (lungs, bronchi, and pleurae) is nourished by the bronchial arteries, which branch from the thoracic aorta.
Each lung is covered by its own double-walled sac, the pleural membrane. The visceral pleura is attached to the outer surface of the lung and then doubles back to form the parietal pleura, which lines the inside of the thoracic cavity, adhering to the chest wall and the diaphragm. The visceral pleura lies closely against the parietal pleura, separated only by very small amounts of fluid in the pleural cavity or space, which is considered only a potential space. The slightly negative pressure (less than atmospheric pressure) in the pleural cavity also assists in holding the pleura in close approximation and promoting lung expansion. The pleural fluid provides lubrication during respiratory movements and a force that provides cohesion, or “sticking together” (high surface tension), between the two pleural layers during inspiration.
The thorax, consisting of ribs, vertebrae, and sternum (breastbone) provides a rigid protective wall for the lungs. The upper seven pairs of ribs (true ribs) articulate with the vertebrae and are attached to the sternum by costal (hyaline) cartilage. The next three pairs of ribs are “false” ribs, which are connected to the costal cartilage of the seventh rib, not directly to the sternum. The last two ribs (also false), the eleventh and twelfth pairs, are attached only to vertebrae and are therefore called floating ribs. Between the ribs are located the external and internal intercostal muscles, which move the thoracic structures during ventilation.
Ventilation
The Process of Inspiration and Expiration
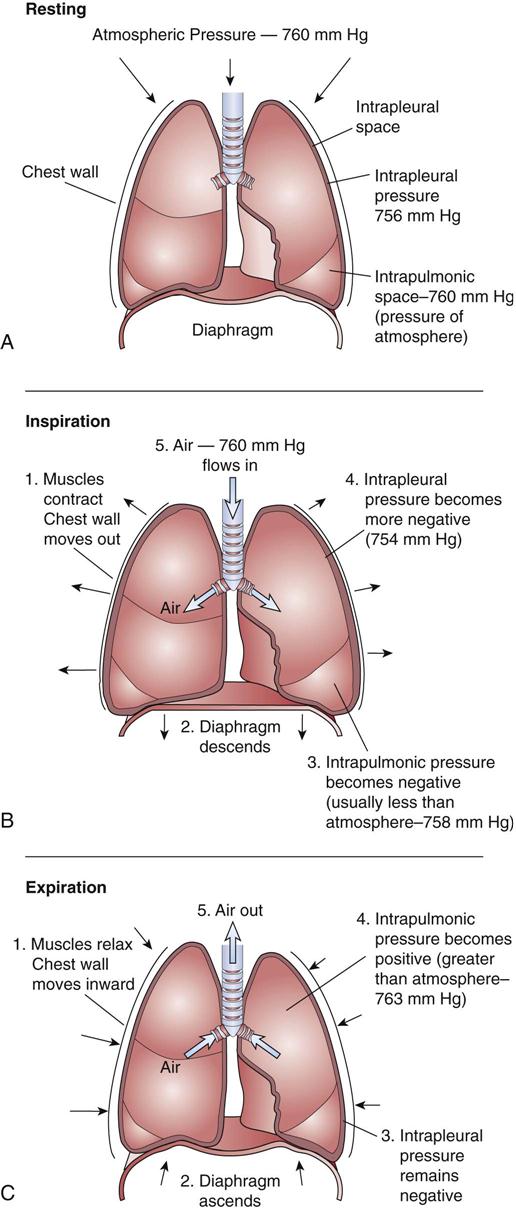
Airflow during inspiration and expiration depends on a pressure gradient, with air always moving from a high pressure area to a low pressure area (flow is one way only!). If atmospheric pressure is higher than air pressure inside the lungs, air will move from the atmosphere into the lungs (inspiration). For expiration to occur, pressure must be higher in the lungs than in the atmosphere. These pressure changes in the lungs result from alterations in the size of the thoracic cavity. As the size of the thoracic cavity decreases, the pressure inside the cavity increases (Boyle’s law).
A sequence of events is responsible for the change in size of the thorax and the changes in airflow with inspiration and expiration:
Forced inspiration or expiration requires additional energy and muscular activity. In forced inspiration the sternocleidomastoid, scalene, pectoralis minor, and serratus muscles contract to increase the elevation of the ribs and sternum. During forceful expiration the abdominal muscles contract to increase upward pressure on the diaphragm, and the intercostal muscles contract, pulling the ribs and sternum down and inward.
Compliance is the term used to refer to the ability of the lungs to expand. Compliance depends largely on the elasticity of the tissues, but can also be affected by other factors, such as alveolar surface tension and the shape, size, and flexibility of the thorax.
Changes in ventilation occur during pregnancy (see Chapter 22) and with aging (see Chapter 24).
Pulmonary Volumes
Pulmonary volumes are a measure of ventilatory capacity in that they measure the air moving in and out of the lungs with normal or forced inspiration and expiration (Fig. 13-3). Pulmonary volumes can change with disease processes and are helpful in monitoring a patient’s progress or response to treatment. For example, impaired expiration can cause an increase in residual volume and therefore increased carbon dioxide levels in body fluids. Some of the basic volumes are summarized in Table 13-1.
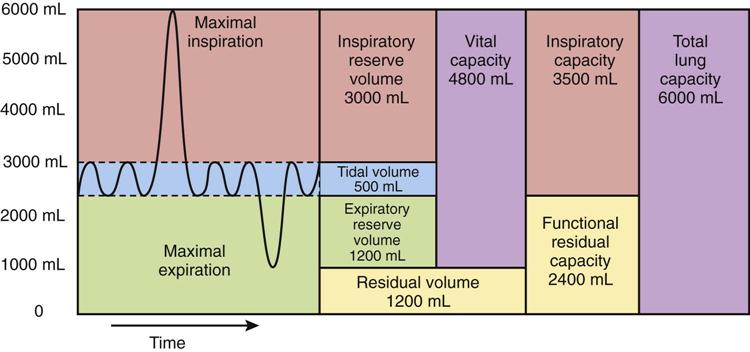
TABLE 13-1
| Name | Volume | Meaning |
| Tidal volume (TV) | 500 mL | Amount of air entering lungs with each normal breath |
| Residual volume (RV) | 1200 mL | Amount of air remaining in the lungs after forced expiration |
| Inspiratory reserve (IRV) | 3000 mL | Maximal amount of air that can be inhaled in excess of normal quiet inspiration |
| Expiratory reserve (ERV) | 1100 mL | Maximal volume of air expired following a passive expiration |
| Vital capacity (VC) | 4600 mL | Maximal amount of air expired following a maximal inspiration |
| Total lung capacity (TLC) | 5800 mL | Total volume of air in the lungs after maximal inspiration |
Control of Ventilation
The primary control centers for breathing are located in the medulla and the pons. The inspiratory center in the medulla controls the basic rhythm by stimulating the phrenic nerves to the diaphragm and the intercostal nerves to the external intercostal muscles. These stimuli occur spontaneously in a rhythmic fashion, each lasting about 2 seconds. The expiratory center in the medulla appears to function primarily when forced expiration is required because normal quiet expiration is a cessation of activity following each inspiration. Additional centers in the pons play a role in coordinating inspiration, expiration, and the intervals for each.
The rate and depth of breathing set by the medullary center can be modified by a number of factors. Any depression of central nervous system activity, for example, by drugs (such as morphine), can lead to slow, shallow breathing. Other factors include activity of the hypothalamus, perhaps in response to emotions; or the stretch receptors in the lungs or the Hering-Breuer reflex, which prevents excessive lung expansion; or voluntary control, as required when singing. However, voluntary control is limited by the levels of carbon dioxide in the blood. When the concentration or partial pressure of carbon dioxide (PaCO2) in the blood rises, breathing resumes automatically. For this reason, a child who intentionally holds his or her breath will eventually have to breathe spontaneously.
Chemical factors are most important in respiratory control. Chemoreceptors sense changes in the levels of carbon dioxide, hydrogen ions, and oxygen in blood or cerebrospinal fluid (Fig. 13-4).
Normal oxygen levels provide a substantial reserve of oxygen in the venous blood. A marked decrease in oxygen (from approximately 105 to 60 mmHg) is necessary before the chemoreceptors respond to hypoxemia. This control mechanism can be important when individuals with chronic lung disease adapt to a sustained elevation in PCO2 and move to a hypoxic drive. Such individuals are dependent on low oxygen levels rather than the normal slight elevation in carbon dioxide to stimulate inspiration. Therefore it is important for these patients always to remain slightly hypoxic and not be given excessive amounts of oxygen at any time.
When carbon dioxide levels in the blood increase (hypercapnia), the gas easily diffuses into the cerebrospinal fluid, lowering pH and stimulating the respiratory center, resulting in an increased rate and depth of respirations (hyperventilation). Hypercapnia causes respiratory acidosis, and acidosis depresses the nervous system. Hypocapnia, or low PCO2, may be caused by hyperventilation after excessive amounts of carbon dioxide have been expired. Hypocapnia causes respiratory alkalosis. To review the conditions of respiratory acidosis and alkalosis and the role of arterial blood gases, refer to Chapter 2.

Gas Exchange
Gas exchange, or external respiration, is the flow of gases between the alveolar air and the blood in the pulmonary circulation. Diffusion of oxygen and carbon dioxide in the lungs depends on the relative concentrations or partial pressures of the gases, and movement of each gas always occurs from a high-pressure area to a low-pressure area. It is customary to refer to the concentration of a gas such as oxygen in a mixture as the partial pressure of that gas, for example, PO2. When the measurement refers specifically to the partial pressure of oxygen in arterial blood, it is expressed as PaO2.
Each gas in a mixture moves or diffuses according to its own partial pressure gradient and independent of other gases (Dalton’s law). For example, oxygen diffuses from alveolar air, an area with a high concentration of oxygen, to the blood in the pulmonary capillary, which has a low concentration of oxygen, until the concentrations become equal (Fig. 13-5). Meanwhile, carbon dioxide diffuses out of the pulmonary capillary into the alveolar air depending on its relative concentrations. Atmospheric air contains oxygen, carbon dioxide, nitrogen, and water. Because the air is not totally expired from the alveoli during expiration and has been humidified during its passage into the lungs, alveolar air has different concentrations of gases than either atmospheric air or blood. The residual air in the alveoli allows continuing gas exchange between expiration and inspiration because blood continually flows through the pulmonary circulation.
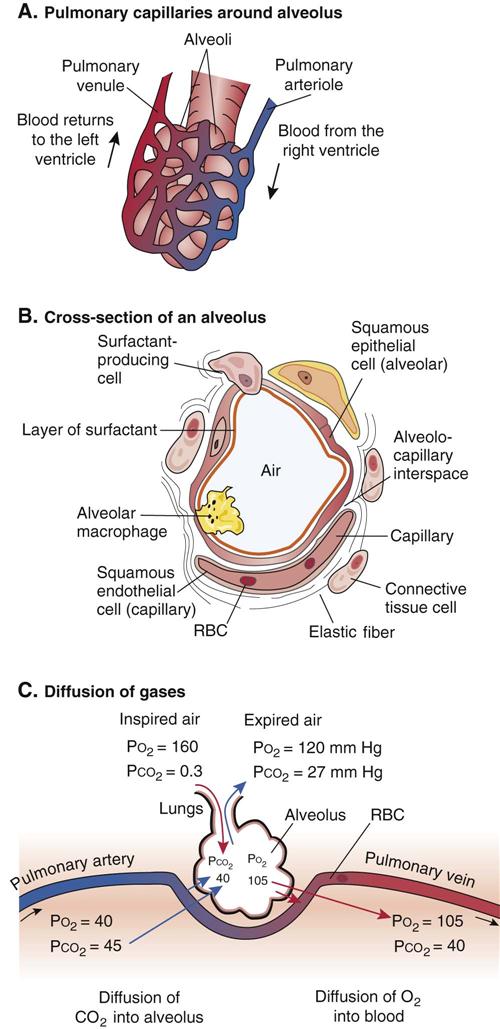
The pulmonary circulation is composed of the pulmonary arteries, which bring venous blood (dark blue-red in color) from the right ventricle of the heart to be oxygenated; the pulmonary capillaries, in which diffusion or gas exchange occurs; and the pulmonary veins, which return the oxygenated blood (bright red) to the left atrium of the heart. The oxygenated blood moves from the left ventricle of the heart, which pumps the blood into the aorta, and the systemic circulation starts.
Factors Affecting Diffusion of Gases
In addition to the partial pressure gradient, diffusion can be altered by other factors such as the thickness of the respiratory membrane. When fluid accumulates in the alveoli or interstitial tissue, diffusion, particularly of oxygen, is greatly impaired. Normally the pressure in the pulmonary circulation is very low, reducing the risk of excessive fluid in the interstitial space and alveoli. The presence of extra fluid may also impede blood flow through the pulmonary capillaries and increase surface tension in the alveoli, restricting expansion of the lung.
Other major factors in gas exchange are the total surface area available for diffusion and the thickness of the alveolar membranes. The alveoli are the only structures that provide such a surface area, and both ventilation and perfusion must be adequate for diffusion to occur (see Fig. 13-20). If part of the alveolar wall is destroyed, as in emphysema, or fibrosis occurs in the lungs, the surface area is greatly reduced. If airflow into the alveoli is obstructed or the capillaries are damaged, the involved surface area becomes nonfunctional.
This imbalance is measured by the ventilation-perfusion ratio ( ). An autoregulatory mechanism in the lungs can adjust ventilation and blood flow in an attempt to produce a good match. For example, if PO2 is low because of poor ventilation in an area, vasoconstriction occurs in the pulmonary arterioles, shunting the blood to other areas of the lungs where ventilation may be better. If airflow is good, the pulmonary arterioles dilate to maximize gas exchange.
). An autoregulatory mechanism in the lungs can adjust ventilation and blood flow in an attempt to produce a good match. For example, if PO2 is low because of poor ventilation in an area, vasoconstriction occurs in the pulmonary arterioles, shunting the blood to other areas of the lungs where ventilation may be better. If airflow is good, the pulmonary arterioles dilate to maximize gas exchange.
Transport of Oxygen and Carbon Dioxide
Only about 1% of total oxygen is dissolved in plasma because oxygen is relatively insoluble in water. This factor also limits the ease with which oxygen can diffuse. The dissolved form of the gas is that which diffuses from the alveolar air into the blood in the pulmonary capillaries and also diffuses into the interstitial fluid and the cells during the process of internal respiration. Most oxygen is transported reversibly bound to hemoglobin by the iron molecules and is called oxyhemoglobin (see Fig. 10-16A for a diagram of hemoglobin and attachments). When all four heme molecules in hemoglobin have taken up oxygen, the hemoglobin is termed fully saturated (measurement expressed as SaO2).
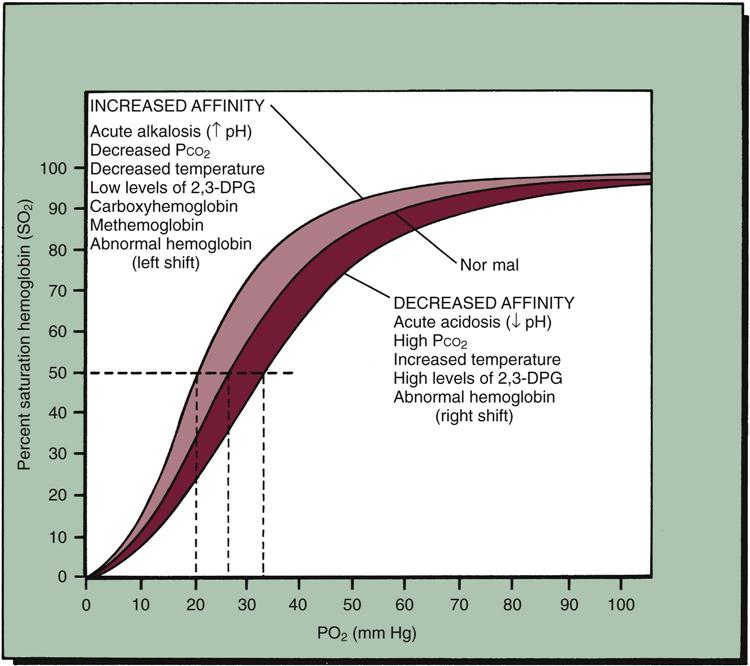
As oxygen diffuses out of the blood into the interstitial fluid and the cells, hemoglobin releases oxygen to replace it, so dissolved oxygen is always available in the plasma, ready to diffuse into the cells. The rate at which hemoglobin binds or releases oxygen depends on factors such as PO2 (the partial pressure of dissolved oxygen), PCO2 temperature, and plasma pH (Fig. 13-6). Normally approximately 25% of the bound oxygen is released to the cells for metabolism during an erythrocyte’s trip through the systemic circulation, leaving 75% of the hemoglobin in the venous blood still saturated with oxygen. This provides a good safety margin of oxygen that is available to meet increased cell demands.
Carbon dioxide, a waste product from cell metabolism, is transported in several forms. Approximately 7% is dissolved in the plasma and can easily diffuse across membranes. Roughly 20% is loosely and reversibly bound to hemoglobin, attached to an amino group on the globin portion (not the heme). This is termed carbaminoglobin. The majority of carbon dioxide resulting from cell metabolism diffuses into the red blood cells (RBCs), where, under the influence of the enzyme carbonic anhydrase, it transitions very briefly as carbonic acid, then is immediately converted into bicarbonate ions (see the following equation). These bicarbonate ions can then diffuse back into the plasma to function in the buffer pair (see Chapter 2).
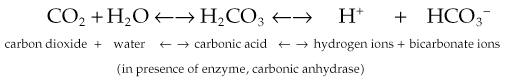
A ratio of 20 parts bicarbonate ion to 1 part carbonic acid maintains blood pH at 7.35. Thus, carbon dioxide plays a major role in control of blood pH through this buffer system.
Diagnostic Tests
General Manifestations of Respiratory Disease
2. Coughing may result from irritation caused by a nasal discharge dripping into the oropharynx, or from inflammation or foreign material in the lower respiratory tract, or from inhaled irritants such as tobacco smoke. An occasional cough is considered a normal event in a healthy person, but a persistent cough may be evidence of a respiratory disease or chronic irritation. Aspiration of food or fluid may cause a spasm of coughing.
The cough reflex is controlled by a center in the medulla and consists of coordinated actions that inspire air and then close the glottis and vocal cords. This is followed by forceful expiration in which the glottis is opened and the unwanted material is blown upward and out of the mouth. In some cases, the product of a cough is swallowed. The effectiveness of the cough depends on the strength of the muscle action during both inspiration and expiration.
A constant dry or unproductive cough is fatiguing because it interferes with sleep, and the respiratory muscles are used excessively. In such cases, a cough-suppressant medication (e.g., codeine or dextromethorphan) may be used at night. A productive cough usually occurs when secretions or inflammatory exudate accumulate in the lungs, and removal of such fluids from the airways is beneficial. Excess secretions may become infected and tend to obstruct the airways. It is helpful in such cases to increase fluid intake to keep the secretions thin and easy to remove. An expectorant medication (e.g., guaifenesin) or the use of a humidifier also may assist in removing secretions. Thick or sticky mucus is particularly difficult to raise from the lungs, especially in elderly or debilitated patients.
3. Sputum or mucoid discharge from the respiratory tract may have significant characteristics depending on the abnormality causing it. Normal secretions are relatively thin, clear, and colorless or cream color.
a. Yellowish-green, cloudy, thick mucus is often an indication of a bacterial infection.
b. Rusty or dark-colored sputum is usually a sign of pneumococcal pneumonia.
4. Breathing patterns and characteristics may be altered with respiratory disease (Fig. 13-7). The normal rate (eupnea) is 10 to 18 inspirations per minute, and the normal pattern is regular and effortless. Changes in the rate, rhythm, depth, and effort of ventilation are significant.
c. Wheezing or whistling sounds indicate obstruction in the small airways.
d. Stridor, a high-pitched crowing noise, usually indicates upper airway obstruction.
5. Breath sounds may be abnormal or absent in respiratory disorders. Rales and rhonchi are abnormal sounds resulting from air mixing with excessive secretions in the lungs.
a. Rales are light bubbly or crackling sounds associated with serous secretions.
b. Rhonchi are deeper and harsher sounds resulting from thicker mucus.
c. Absence of breath sounds indicates nonaeration or collapse of a lung (atelectasis).
6. Dyspnea is a subjective feeling of discomfort that occurs when a person feels unable to inhale enough air. It may be manifested as breathlessness or shortness of breath, either with exertion or at rest.
c. Paroxysmal nocturnal dyspnea is a sudden acute type of dyspnea common in patients with left-sided congestive heart failure. During sleep the body fluid is redistributed, leading to pulmonary edema, and the individual wakes up gasping for air and coughing (see Chapter 12).
11. Changes in arterial blood gases (ABGs): Hypoxemia refers to inadequate oxygen in the blood (PaO2). Hypoxia, or inadequate oxygen supply to the cells, may have many causes:
a. A deficit of RBCs or hemoglobin levels that are too low for adequate oxygen transport
Hypoxia affects cell metabolism, reducing cell function and leading to anaerobic metabolism and the development of metabolic acidosis. The brain is most susceptible to an oxygen deficit because it has little storage capacity for oxygen and yet has a constant demand. Cerebral hypoxia initially stimulates the sympathetic nervous system. Decreased cell function is indicated by fatigue, lethargy or stupor, and muscle weakness. Extreme or prolonged hypoxia can result in cell death.
Compensation mechanisms for hypoxia due to respiratory impairment include increased cardiovascular activity such as tachycardia and increased blood pressure. In people with chronic hypoxia due to respiratory or circulatory impairment, erythropoietin secretion is increased, stimulating the bone marrow to produce additional red blood cells (secondary polycythemia).
Acid-base imbalance may develop from respiratory disorders (see Chapter 2). Respiratory acidosis due to excess carbon dioxide (increased carbonic acid) is more common and results from impaired expiration. Arterial blood gases in this situation indicate high PCO2 and low serum pH. Respiratory alkalosis occurs when the respiratory rate is increased, usually because of acute anxiety or excessive intake of aspirin.
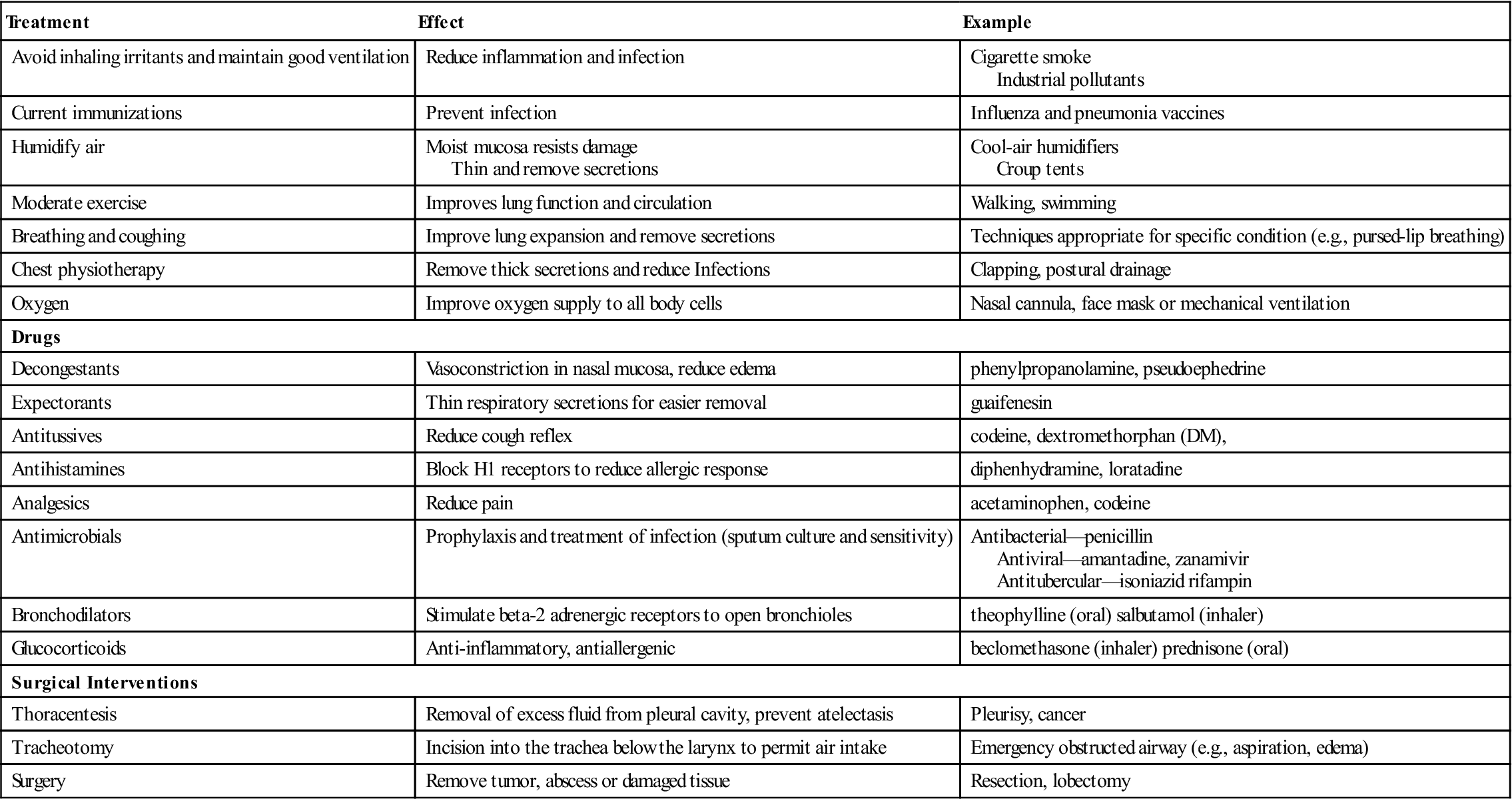
Common Treatment Measures for Respiratory Disorders
A number of treatment modalities are recommended for many respiratory diseases. A few examples are summarized in Table 13-2.
TABLE 13-2
Basic Therapies for Respiratory Disorders
| Treatment | Effect | Example |
| Avoid inhaling irritants and maintain good ventilation | Reduce inflammation and infection | Cigarette smoke Industrial pollutants |
| Current immunizations | Prevent infection | Influenza and pneumonia vaccines |
| Humidify air | Moist mucosa resists damage Thin and remove secretions | Cool-air humidifiers Croup tents |
| Moderate exercise | Improves lung function and circulation | Walking, swimming |
| Breathing and coughing | Improve lung expansion and remove secretions | Techniques appropriate for specific condition (e.g., pursed-lip breathing) |
| Chest physiotherapy | Remove thick secretions and reduce Infections | Clapping, postural drainage |
| Oxygen | Improve oxygen supply to all body cells | Nasal cannula, face mask or mechanical ventilation |
| Drugs | ||
| Decongestants | Vasoconstriction in nasal mucosa, reduce edema | phenylpropanolamine, pseudoephedrine |
| Expectorants | Thin respiratory secretions for easier removal | guaifenesin |
| Antitussives | Reduce cough reflex | codeine, dextromethorphan (DM), |
| Antihistamines | Block H1 receptors to reduce allergic response | diphenhydramine, loratadine |
| Analgesics | Reduce pain | acetaminophen, codeine |
| Antimicrobials | Prophylaxis and treatment of infection (sputum culture and sensitivity) | Antibacterial—penicillin Antiviral—amantadine, zanamivir Antitubercular—isoniazid rifampin |
| Bronchodilators | Stimulate beta-2 adrenergic receptors to open bronchioles | theophylline (oral) salbutamol (inhaler) |
| Glucocorticoids | Anti-inflammatory, antiallergenic | beclomethasone (inhaler) prednisone (oral) |
| Surgical Interventions | ||
| Thoracentesis | Removal of excess fluid from pleural cavity, prevent atelectasis | Pleurisy, cancer |
| Tracheotomy | Incision into the trachea below the larynx to permit air intake | Emergency obstructed airway (e.g., aspiration, edema) |
| Surgery | Remove tumor, abscess or damaged tissue | Resection, lobectomy |
Infectious Diseases
Upper Respiratory Tract Infections
Common Cold (Infectious Rhinitis)
The common cold is caused by a viral infection of the upper respiratory tract. The most common pathogen is a rhinovirus, but it may also be an adenovirus, parainfluenza virus, or coronavirus. There are more than 200 possible causative organisms, so it is difficult for an individual to develop sufficient immunity to avoid all colds. Children do acquire more colds than adults, usually as a brief, self-limiting infection, unless a secondary bacterial infection develops. The common cold is spread through respiratory droplets, which either are directly inhaled or are spread by secretions on hands or contaminated objects such as facial tissue. The infection is highly contagious because the virus is shed in large numbers from the infected nasal mucosa during the first few days of the infection and can survive for several hours outside the body.
Initially the mucous membranes of the nose and pharynx are red and swollen, with increased secretions. The signs of a cold include nasal congestion and copious watery discharge (rhinorrhea, sneezing, and sometimes watery eyes). Mouth breathing is common, and a change in the tone of voice is noticeable. There may be sore throat, headache, slight fever, and malaise. Cough may develop from the irritation of the secretions dripping into the pharynx. Sometimes the feeling of stuffiness and irritation persists as the secretions become more viscous for a few days after the acute period has passed. The infection and inflammation may spread to cause pharyngitis, laryngitis, or acute bronchitis.
Treatment is symptomatic, consisting of acetaminophen for fever and headache and decongestants (vasoconstrictors) to reduce the edema and congestion in the respiratory passages. A cold is a self-limiting infection. Antihistamines reduce secretions but may cause excessive drying of tissues and cough. Humidifiers aid in keeping the secretions liquid and easily drained. The role of vitamin C in prevention and therapy remains controversial. Antibiotics do not cure viral infections and are usually reserved for secondary bacterial infections such as sinusitis, otitis media (see Chapter 15), or tracheitis, or for prophylactic use in high-risk patients (such as those with chronic illnesses). Proper handwashing and disposal of tissues as well as avoidance of crowded areas reduce the risk of transmission to others.
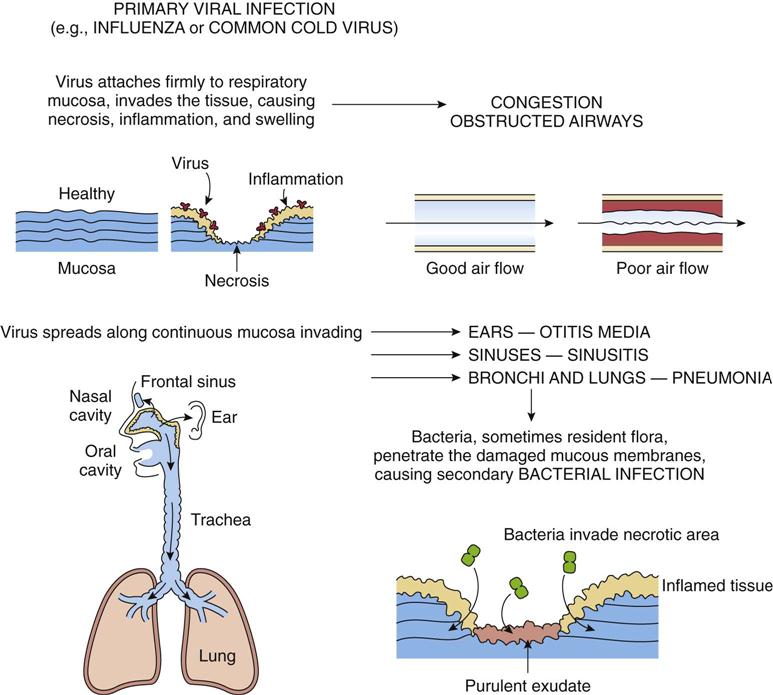
Secondary bacterial infections, for example, pharyngitis or “strep throat,” are usually caused by streptococcus invading inflamed and necrotic mucous membranes (Fig. 13-8). A purulent exudate forms and systemic signs such as fever develop. These bacteria should be identified by culture and treated quickly with antimicrobial drugs to reduce the risk of rheumatic fever or acute glomerulonephritis arising from group A beta-hemolytic Streptococcus pneumoniae.
Sinusitis
Sinusitis is usually a bacterial infection secondary to a cold or an allergy that has obstructed the drainage of one or more of the paranasal sinuses into the nasal cavity (see Fig. 13-1). Common causative organisms include pneumococci, streptococci, or Haemophilus influenzae. As the exudate accumulates, pressure builds up inside the sinus cavity, causing severe pain in the facial bone. The pain may be confused with headache (ethmoid sinus) or toothache (maxillary sinus). Other signs, such as nasal congestion, fever, or sore throat, may already be present. Diagnosis may be confirmed by radiograph or transillumination. Decongestants and analgesics are recommended until the sinuses are draining well, and a course of antibiotics is often required to eradicate the infection totally.
Laryngotracheobronchitis (Croup)
Laryngotracheobronchitis is a common viral infection, particularly in children between 1 and 2 years of age, although adults may also contract laryngitis, tracheitis, or bronchitis. Common causative organisms are parainfluenza viruses and adenoviruses (Table 13-3). The infection begins as an upper respiratory condition with nasal congestion and cough. In the young child, the larynx and subglottic area become inflamed with swelling and exudate, leading to obstruction and a characteristic barking cough (croup), hoarse voice, and inspiratory stridor. The condition often becomes more severe at night. Cool, moisturized air from a humidifier or shower or croup tent often relieves the obstruction. The infection is usually self-limited, and full recovery occurs in several days. In some children with allergic tendencies, smooth muscle spasm may exacerbate the obstruction, requiring additional medical treatment.
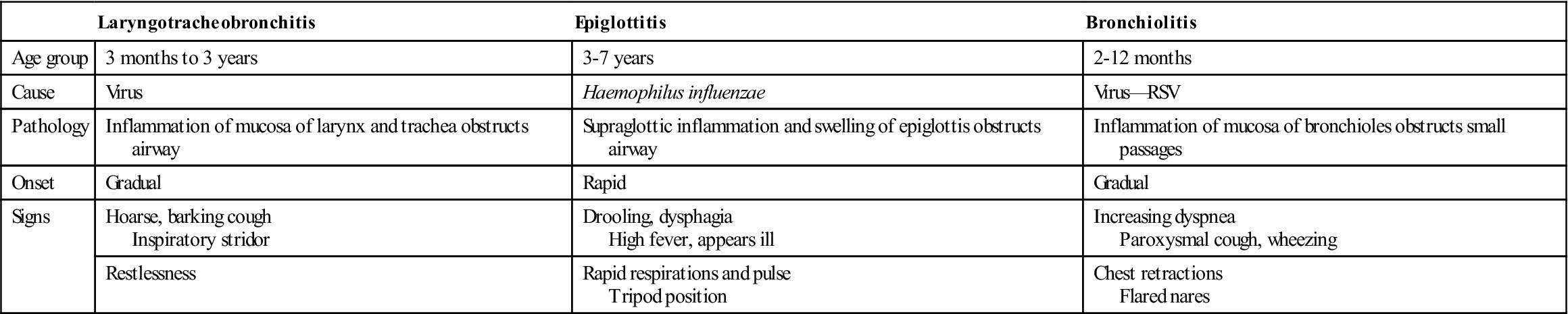
TABLE 13-3
General Comparison of Respiratory Infections in Children
| Laryngotracheobronchitis | Epiglottitis | Bronchiolitis | |
| Age group | 3 months to 3 years | 3-7 years | 2-12 months |
| Cause | Virus | Haemophilus influenzae | Virus—RSV |
| Pathology | Inflammation of mucosa of larynx and trachea obstructs airway | Supraglottic inflammation and swelling of epiglottis obstructs airway | Inflammation of mucosa of bronchioles obstructs small passages |
| Onset | Gradual | Rapid | Gradual |
| Signs | Hoarse, barking cough Inspiratory stridor | Drooling, dysphagia High fever, appears ill | Increasing dyspnea Paroxysmal cough, wheezing |
| Restlessness | Rapid respirations and pulse Tripod position | Chest retractions Flared nares |
Epiglottitis
Epiglottitis is an acute infection usually caused by the bacterial organism, H. influenzae type B. It is common in children in the 3- to 7-year-old group, although the incidence has been increasing in adults. The infection causes swelling of the larynx, supraglottic area, and epiglottis, which appears as a round, red ball obstructing the airway. Onset is rapid, fever and sore throat develop, and the child refuses to swallow. Drooling of saliva is apparent, and inspiratory stridor is heard. The child appears anxious and pale and assumes a sitting position (tripod position) with the mouth open, struggling to breathe. Caution is required during laryngeal examination to prevent reflex spasm and total obstruction of the airway. Treatment consists of oxygen and antimicrobial therapy, with intubation or tracheotomy if necessary.
Influenza (Flu)
Influenza is a viral infection that may affect both the upper and the lower respiratory tracts. As indicated in the discussion of this topic at the end of Chapter 6 (influenza is presented as an example of infection), there are three groups of the influenza virus—type A, the most prevalent pathogen, and types B and C. These viruses mutate constantly, preventing effective immune defense for prolonged time periods.
Flu differs from a common cold in that it usually has a sudden, acute onset with fever, marked fatigue, and aching pains in the body. It may also cause a viral pneumonia. Similarly to the common cold, a mild case of influenza can be complicated by secondary problems such as bacterial pneumonia. Most deaths during flu epidemics result from pneumonia.
Treatment is symptomatic and supportive unless bacterial infection occurs. Antiviral drugs, such as amantadine (Symmetrel, Endantadine), zanamivir (Relenza inhaler), or oseltamivir (Tamiflu) taken by adults in the first 2 days, may reduce the symptoms and duration as well as reduce the risk of infecting others. These drugs are useful in the control of flu outbreaks in hospitals or nursing homes. The incubation period for the virus is 1 to 4 days, with an average of 2, but the individual can pass the virus on a day before symptoms develop and for up to 5 days after.
Prevention of influenza by vaccination is highly recommended for all individuals. If flu does develop following immunization, it is a mild infection. A period of 2 to 3 weeks after vaccination is required before immunity develops.
Scarlet Fever
An upper respiratory infection caused by group A β-hemolytic streptococcus (Streptococcus pyogenes). Incubation period is generally 1 to 2 days. Symptoms usually begin with a fever and sore throat; chills, vomiting, abdominal pain, and malaise may occur as well. The typical “strawberry” tongue (Fig. 13-9) is caused by the exotoxin produced by the bacteria. A fine rash on the chest, neck, groin, and thighs are characteristic also. Once a serious childhood disease, upper respiratory infection is now generally treatable with antibiotics.
Lower Respiratory Tract Infections
Bronchiolitis (Respiratory Syncytial Virus Infection)
Bronchiolitis is a common infection in young children 2 to 12 months of age and is caused by the respiratory syncytial virus (RSV), a myxovirus. It is transmitted directly by oral droplet and occurs more frequently in the winter months. Predisposing factors include a familial history of asthma and the presence of cigarette smoke. Bronchiolitis varies in severity. The virus causes necrosis and inflammation in the small bronchi and bronchioles, with edema, increased secretions, and reflex bronchospasm leading to obstruction of the small airways. Signs include wheezing and dyspnea; rapid, shallow respirations; cough; rales; chest retractions; fever; and malaise. There may be areas of hyperinflation with air trapping due to partial obstruction (see Fig. 13-19C) or areas of atelectasis or nonaeration resulting from total obstruction (see Fig. 13-24). Treatment is supportive and symptomatic, with monitoring of blood gases in severe cases to ensure that oxygen levels are adequate. Respiratory syncytial virus-immunoglobulin serum or palivizumab, an RSV monoclonal antibody, may be administered to reduce the severity of infection, particularly in premature infants.
Pneumonia
Pneumonia may develop as a primary acute infection in the lungs or it may be secondary to another respiratory or systemic condition in which tissue resistance is reduced. Pneumonia is a risk following any aspiration or inflammation in the lung, when fluids pool or defense mechanisms such as cilia are reduced. In most cases the organisms enter the lungs directly, by inhalation (virus), resident bacteria spreading along the mucosa, or aspiration in secretions. Occasionally the infection is blood-borne.
Classification of the Pneumonias
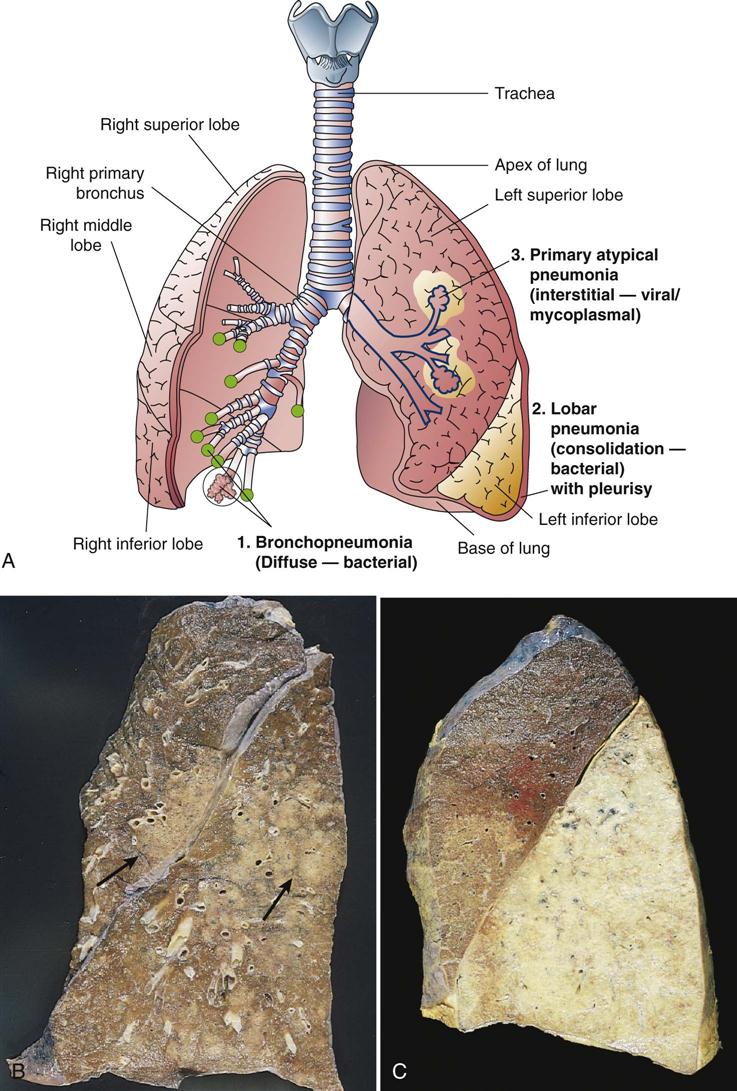
Numerous methods are available for classifying pneumonias. Categories may be based on the causative agent, anatomic location of the infection, pathophysiologic changes, or epidemiologic data.
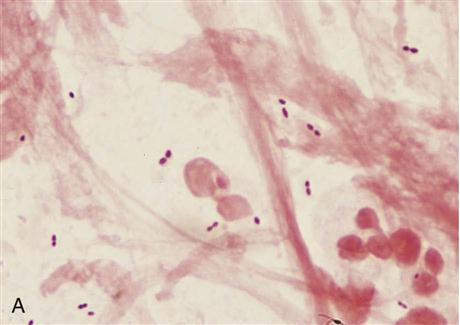
For example, the causative agent may be a virus, bacterium, or fungus. Pneumonia may involve multiple microbes following aspiration. Usually lobar pneumonia is bacterial, the most common agent being a pneumococcus, but other causative organisms include Staphylococcus aureus and Legionella (Legionnaire’s disease). Severe pneumococcal pneumonia is less common now because antibacterial medications are quickly administered, but it remains a major threat to those with chronic disease. A vaccine that provides protection against the seven most common agents of pneumonia is available for those with chronic respiratory or cardiovascular disease as well as clients greater than 65 years of age. Re-immunization does not appear to be necessary, but may be done without risk. In immune-suppressed individuals, other organisms such as Candida (fungus) or Pneumocystis carinii may cause pneumonia.
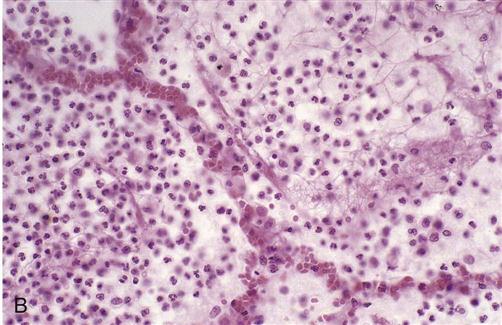
Anatomic distribution of lesions may be diffuse and patchy throughout both lungs or lobar, meaning consolidated in one lobe (Fig. 13-10). In some pneumonias, such as viral, pathophysiologic changes occur primarily in the interstitial tissue or alveolar septae. In other types, such as pneumococcal, the alveoli are inflamed and filled with exudate, resulting in a solid mass in a lobe.
Epidemiologic categories refer to nosocomial (hospital-acquired) pneumonia, which affects those with less resistance, the elderly, the debilitated, the malnourished, or the immune suppressed. In these cases, infection often results from gram-negative organisms such as Klebsiella pneumoniae or Pseudomonas aeruginosa. Community-acquired pneumonia may be viral or bacterial. It can affect healthy persons, such as following influenza, as well as persons with underlying cardiovascular or respiratory disease. Aspiration pneumonia may be nosocomial or community acquired. It frequently involves aspiration of vomitus, which is irritating to tissues, or nasopharyngeal secretions. Mixed bacteria are usually isolated from the resultant infection. When periodontal disease is marked, aspiration pneumonia results from infection by gram-negative microbes.
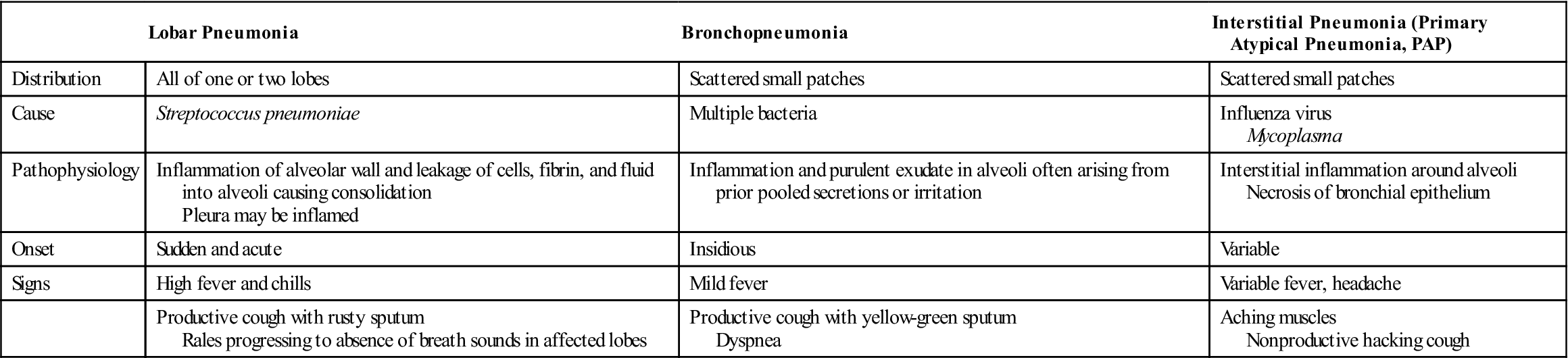
A brief comparison of common types of pneumonia is found in Table 13-4.
TABLE 13-4
| Lobar Pneumonia | Bronchopneumonia | Interstitial Pneumonia (Primary Atypical Pneumonia, PAP) | |
| Distribution | All of one or two lobes | Scattered small patches | Scattered small patches |
| Cause | Streptococcus pneumoniae | Multiple bacteria | Influenza virus Mycoplasma |
| Pathophysiology | Inflammation of alveolar wall and leakage of cells, fibrin, and fluid into alveoli causing consolidation Pleura may be inflamed | Inflammation and purulent exudate in alveoli often arising from prior pooled secretions or irritation | Interstitial inflammation around alveoli Necrosis of bronchial epithelium |
| Onset | Sudden and acute | Insidious | Variable |
| Signs | High fever and chills | Mild fever | Variable fever, headache |
| Productive cough with rusty sputum Rales progressing to absence of breath sounds in affected lobes | Productive cough with yellow-green sputum Dyspnea | Aching muscles Nonproductive hacking cough |
Lobar Pneumonia
Lobar pneumonia (pneumococcal pneumonia) is usually caused by Streptococcus pneumoniae (pneumococcus), and the infection is localized in one or more lobes (Fig. 13-11). This microbe sometimes colonizes the nasopharynx without producing symptoms. The first stage in its development is congestion, in which inflammation and vascular congestion develop in the alveolar wall, and exudate forms in the alveoli. This change interferes greatly with oxygen diffusion. Next, neutrophils, RBCs, and fibrin accumulate in the alveolar exudate, forming a solid mass in the lobe, called consolidation. The presence of these RBCs in the exudate produces the typical rusty sputum associated with lobar pneumonia. Eventually the RBCs break down, and as the infection resolves, macrophages break down the exudate to allow it to be expectorated or resorbed. Because a complete lobe is usually involved in the inflammatory process, the adjacent pleurae are frequently involved, producing pleuritic pain at the affected site (pleurisy or pleuritis). As well, infection may spread into the pleural cavity, causing empyema. If not resolved quickly, empyema can cause adhesions between the pleural membranes, restricting ventilation. Chest x-rays confirm the typical distribution of the infection, and a sputum culture identifies the organism.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree