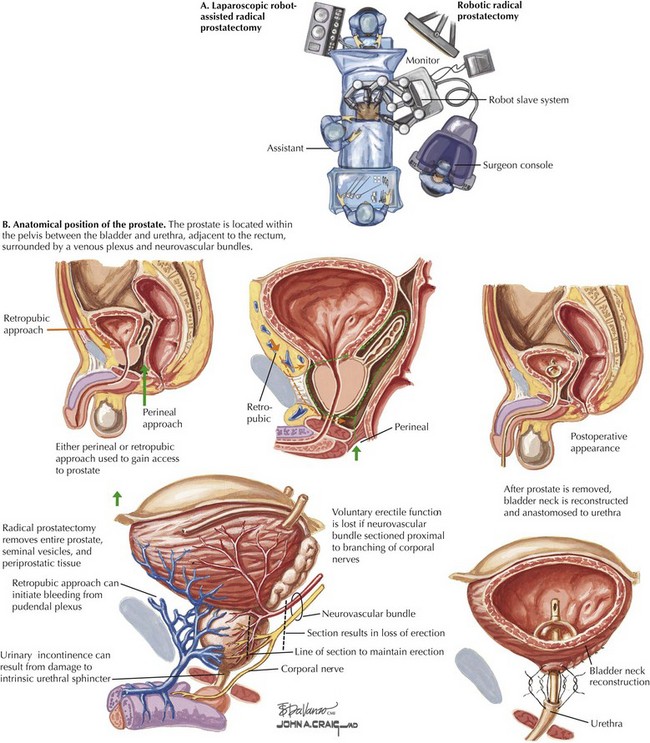
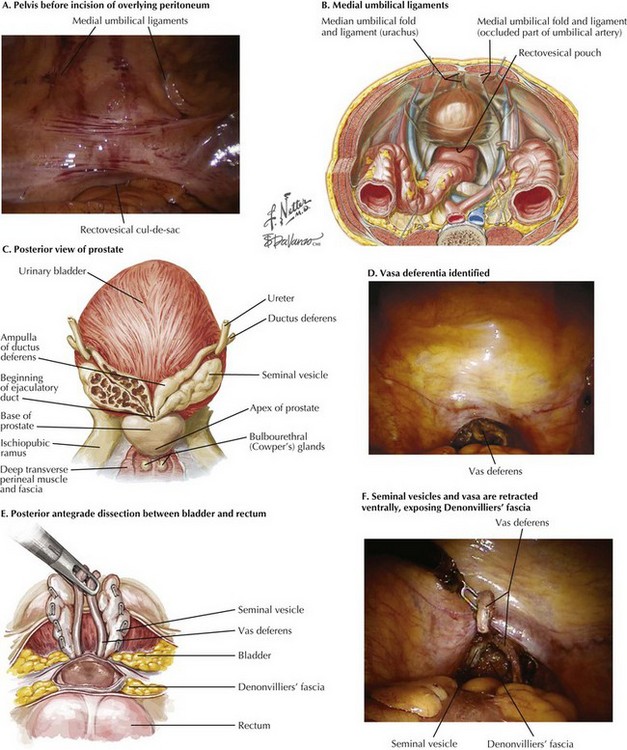
Chapter 54 Traditionally, radical prostatectomy has been performed in the open retropubic or perineal approach. In the last decade, however, use of minimally invasive approaches has dramatically increased, particularly laparoscopic robot-assisted radical prostatectomy (Fig. 54-1, A). This approach has gained popularity because of its greater technical ease for the surgeon, especially with laparoscopic suturing, which allows for more precise suture placement during the vesicourethral anastomosis. The variation in prostate size and shape, as well as its location deep in the pelvis between the bladder and urethra and adjacent to the rectum, make surgical extirpation challenging (Fig. 54-1, B). Additionally, the prostate is surrounded by a venous plexus, and the neurovascular bundles responsible for erection run alongside the prostate. Therefore the surgical dissection required during radical prostatectomy should be performed meticulously by a surgeon with detailed knowledge of the anatomic relationships of the prostate. Posterior Prostatic Dissection Initial inspection of the pelvis is performed to identify the relevant landmarks: the medial umbilical ligaments and the vasa deferentia. The rectovesical cul-de-sac (pouch of Douglas) is approached, and the courses of the vasa are identified through the peritoneal layer (Fig. 54-2, A-D). The seminal vesicles and vasa are retracted ventrally, exposing Denonvilliers’ fascia (Fig. 54-2, E and F). This fascia is incised sharply just dorsal to the base of the prostate. This approach allows entry into a plane containing perirectal fat, and the surgeon can then carefully dissect the prostate off of the rectum in an antegrade direction to the prostatic apex.
Radical Prostatectomy
Introduction
Prostate Cancer: Therapeutic Principles
Surgical Approach
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Basicmedical Key
Fastest Basicmedical Insight Engine