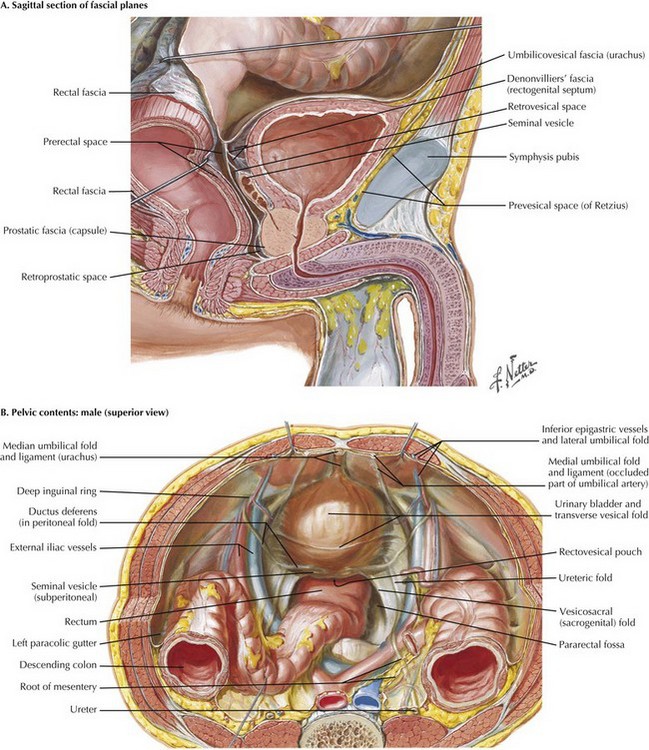
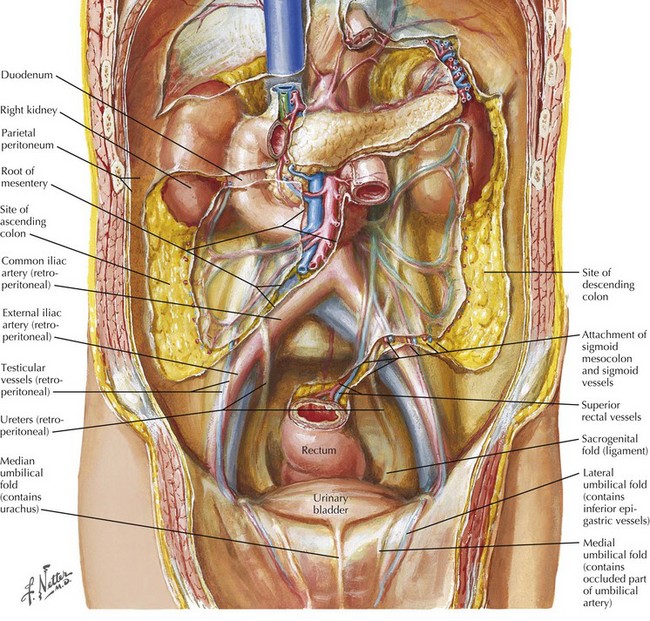
Chapter 55 With the medial umbilical ligaments traced inferiorly and the space of Retzius open, a self-retaining retractor can be placed to facilitate exposure. Extra care is taken when applying traction on the most inferior aspect of the wound; injury to the femoral and genitofemoral nerves can result from prolonged stretch or compression. The symphysis should be visible with the retractor in place (Fig. 55-1, A). The peritoneal wings previously left in place by developing the space of Retzius and opening the peritoneum from the umbilicus to the inguinal ring are easily seen and divided with electrocautery to the level of the vas deferens in the male patient. The vas deferens is divided with the understanding that vascular structures are associated with both vasa. The authors prefer to use ties to allow later identification of the seminal vesicles (Fig. 55-1, B). The left ureter is identified posterior to the sigmoid colon, in a position often more medial than expected. The retroperitoneal space behind the sigmoid colon at the level of the sacral promontory is opened to allow the ureter to be passed to the other side after its division. The right ureter is found by dividing the visible peritoneal fold overlying it (Fig. 55-2).
Radical Cystectomy
Surgical Approach
Bladder Mobilization
Dissection of Ureters
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Basicmedical Key
Fastest Basicmedical Insight Engine