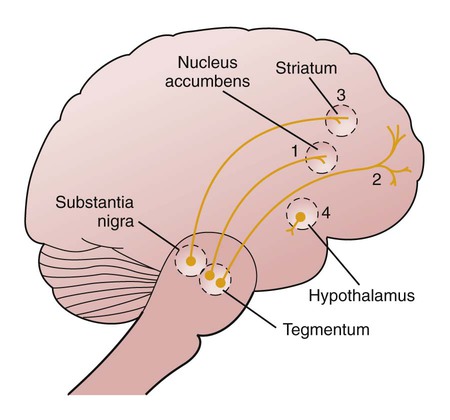
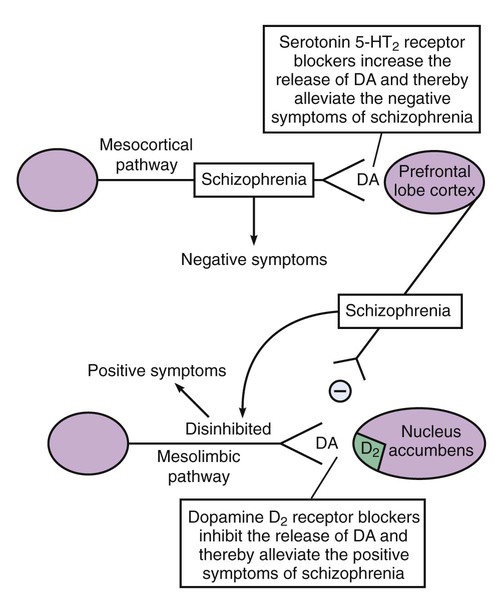
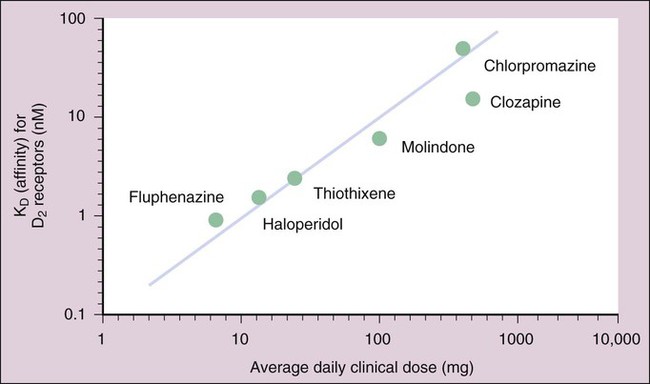
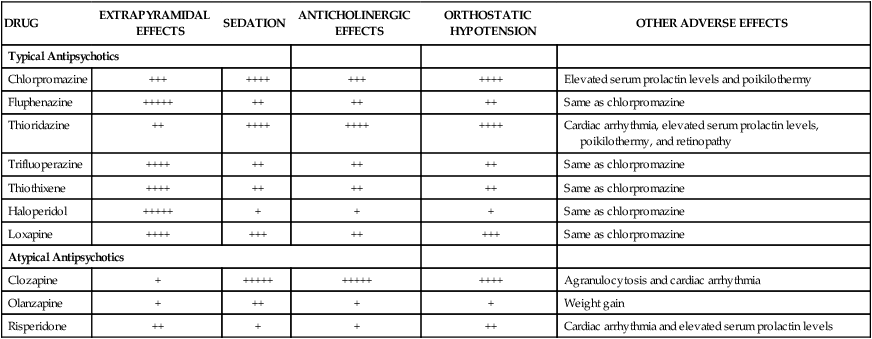
As shown in Box 22-1, the symptoms of schizophrenia can be divided into two groups. The positive symptoms, which include delusions and hallucinations, probably result from excessive neuronal activity in mesolimbic neuronal pathways. These symptoms are usually the primary manifestations of acute psychotic episodes. The negative symptoms, which include apathy, withdrawal, and lack of motivation and pleasure, probably result from insufficient activity in mesocortical neuronal pathways. The negative symptoms generally are more difficult to treat, often persist after positive symptoms resolve, and are associated with a poor prognosis. Many hypotheses exist regarding the biologic basis of schizophrenia. According to the dopamine hypothesis, schizophrenia results from abnormalities in dopamine neurotransmission in mesolimbic and mesocortical neuronal pathways (Box 22-2). Much of the evidence supporting this hypothesis is based on the clinical effects of agents that alter dopaminergic transmission. Dopamine turnover in the brain, which reflects the neuronal release of dopamine, can be studied by measuring the concentration of the principal metabolite of dopamine, homovanillic acid, in the cerebrospinal fluid. Although elevated levels of homovanillic acid are not found in patients with chronic schizophrenia, they are found in some schizophrenic patients having acute psychotic episodes. Evidence also exists for a dopamine receptor defect in schizophrenic patients. Positive emission tomography scanning using D2 receptor ligands has revealed that schizophrenic patients have decreased D2 receptor densities in the prefrontal lobe cortex (but increased D2 receptor densities in the caudate nucleus). These findings lend overall support to the dopamine hypothesis, although it is clear from the clinical effectiveness of atypical antipsychotics that 5-hydroxytryptamine (5-HT2) and other types of dopamine receptors may be involved (Box 22-3). The antipsychotic drugs interact with multiple neurotransmitter systems. Whereas the therapeutic effects of these drugs are believed to result from competitive blockade of dopamine receptors and serotonin (5-HT) receptors, the adverse effects are attributed to the blockade of a variety of receptors (Table 22-1). TABLE 22-1 Mechanisms Responsible for the Therapeutic and Adverse Effects of Antipsychotic Drugs *Sedation may be considered a therapeutic effect with a typical antipsychotic administered for acute psychosis. Typical antipsychotic drugs have an equal or greater affinity for D2 receptors than for 5-HT2 receptors. As shown in Figure 22-1, an excellent correlation exists between the clinical potency of these drugs and their in vitro affinity for D2 receptors. Whereas antagonism of D2 receptors in mesolimbic pathways is thought to repress the positive symptoms of schizophrenia, blockade of D2 receptors in the basal ganglia is believed to be responsible for the parkinsonian and other EPSs that sometimes occur in patients taking antipsychotic drugs. In the peripheral autonomic nervous system, antipsychotic drugs also block muscarinic receptors and α1-adrenoceptors, thereby causing the adverse effects described in Tables 22-1 and 22-2. Antagonism at α1-adrenoceptors produces dizziness, orthostatic hypotension, and reflex tachycardia. Muscarinic receptor antagonism produces blurred vision, dry mouth, constipation, and urinary retention. Antagonism of brain H1 receptors produces drowsiness and weight gain. TABLE 22-2 Adverse Effects of Selected Antipsychotic Drugs* *Ratings range from extremely low (+) to extremely high (+++++). Neuroleptic malignant syndrome is a severe form of drug toxicity that occurs in 0.5% to 1% of patients treated with antipsychotic drugs. It is a life-threatening condition characterized by muscle rigidity, elevated temperature (>38° C), altered consciousness, and autonomic dysfunction (tachycardia, diaphoresis, tachypnea, and urinary and fecal incontinence). The syndrome resembles malignant hyperthermia triggered by halogenated anesthetics in its rapid onset and mortality rate. Neuroleptic malignant syndrome is managed by immediately discontinuing treatment with the offending antipsychotic drug, administering dantrolene to prevent further muscle abnormality (see Chapter 21), and providing supportive care. If future antipsychotic therapy is required in patients who have experienced this syndrome, an atypical drug should be used because the atypical drugs are associated with a lower incidence of neuroleptic malignant syndrome. Antipsychotic agents are primarily used to treat schizophrenia and other forms of psychosis, including drug-induced psychosis and psychosis associated with the manic phase of bipolar disorder. They are also used to treat severely agitated patients, including those with dementia and severe mental retardation. Because the phenothiazines have antiemetic activity, some of them are used in the management of nausea and vomiting (see Chapter 28). Numerous typical antipsychotics are available for the treatment of schizophrenia and related conditions. The four representative examples discussed in detail here are chlorpromazine, fluphenazine, thioridazine, and haloperidol. These drugs have similar therapeutic effects but differ in their relative potency (Table 22-3) and in their side effect profiles (see Table 22-2). TABLE 22-3 Pharmacologic Properties of Selected Antipsychotic Drugs* *Values shown are the mean of values reported in the literature. †Low, 50-2000 mg/day; medium, 20-250 mg/day; and high, 1-100 mg/day. The typical antipsychotics are adequately absorbed from the gut after oral administration. Several agents are also administered parenterally, including long-acting depot preparations for intramuscular injection. These agents are extensively metabolized to a large number of active and inactive metabolites before they are excreted in the urine, and they have elimination half-lives ranging from 20 to 30 hours (see Table 22-3).
Psychotherapeutic Drugs
Schizophrenia
Clinical Findings
Dopamine Hypothesis
Drug Properties
Mechanism of Action
MECHANISM
THERAPEUTIC EFFECTS
ADVERSE EFFECTS
Blockade of α1-adrenoceptors
—
Dizziness, orthostatic hypotension, and reflex tachycardia
Blockade of dopamine D2 receptors
Alleviation of positive symptoms of schizophrenia
Extrapyramidal effects (akathisia, dystonia, and pseudoparkinsonism) and elevated serum prolactin levels
Blockade of dopamine D4 receptors
Alleviation of negative symptoms of schizophrenia and decrease in the incidence of extrapyramidal side effects
—
Blockade of histamine H1 receptors
—
(Sedation)*
Drowsiness and increase in appetite and weight
Blockade of muscarinic receptors
—
Blurred vision, constipation, dry mouth, and urinary retention
Blockade of serotonin 5-HT2 receptors
Alleviation of negative symptoms of schizophrenia and decrease in the incidence of extrapyramidal side effects
Anxiety and insomnia
Adverse Effects
DRUG
EXTRAPYRAMIDAL EFFECTS
SEDATION
ANTICHOLINERGIC EFFECTS
ORTHOSTATIC HYPOTENSION
OTHER ADVERSE EFFECTS
Typical Antipsychotics
Chlorpromazine
+++
++++
+++
++++
Elevated serum prolactin levels and poikilothermy
Fluphenazine
+++++
++
++
++
Same as chlorpromazine
Thioridazine
++
++++
++++
++++
Cardiac arrhythmia, elevated serum prolactin levels, poikilothermy, and retinopathy
Trifluoperazine
++++
++
++
++
Same as chlorpromazine
Thiothixene
++++
++
++
++
Same as chlorpromazine
Haloperidol
+++++
+
+
+
Same as chlorpromazine
Loxapine
++++
+++
++
+++
Same as chlorpromazine
Atypical Antipsychotics
Clozapine
+
+++++
+++++
++++
Agranulocytosis and cardiac arrhythmia
Olanzapine
+
++
+
+
Weight gain
Risperidone
++
+
+
++
Cardiac arrhythmia and elevated serum prolactin levels
Indications
Drug Classification
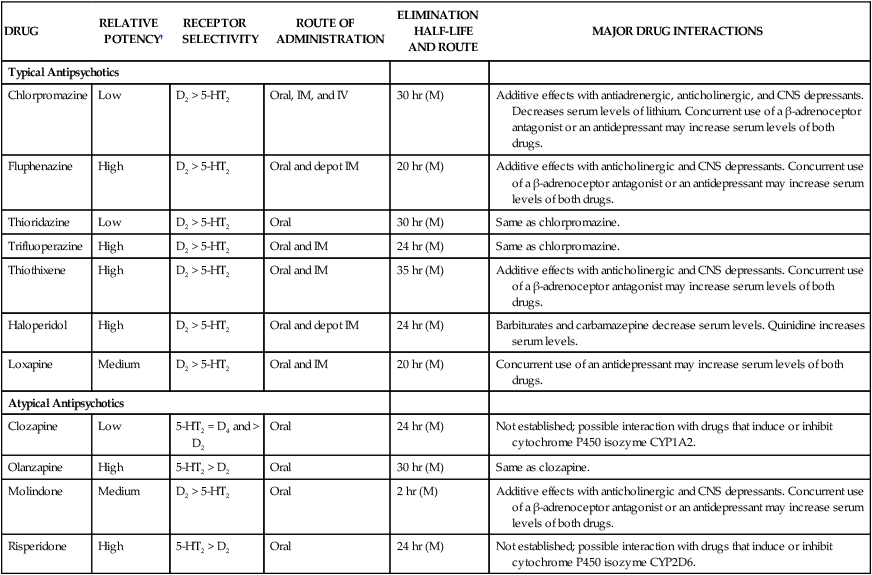
Typical Antipsychotic Agents
DRUG
RELATIVE POTENCY†
RECEPTOR SELECTIVITY
ROUTE OF ADMINISTRATION
ELIMINATION HALF-LIFE AND ROUTE
MAJOR DRUG INTERACTIONS
Typical Antipsychotics
Chlorpromazine
Low
D2 > 5-HT2
Oral, IM, and IV
30 hr (M)
Additive effects with antiadrenergic, anticholinergic, and CNS depressants. Decreases serum levels of lithium. Concurrent use of a β-adrenoceptor antagonist or an antidepressant may increase serum levels of both drugs.
Fluphenazine
High
D2 > 5-HT2
Oral and depot IM
20 hr (M)
Additive effects with anticholinergic and CNS depressants. Concurrent use of a β-adrenoceptor antagonist or an antidepressant may increase serum levels of both drugs.
Thioridazine
Low
D2 > 5-HT2
Oral
30 hr (M)
Same as chlorpromazine.
Trifluoperazine
High
D2 > 5-HT2
Oral and IM
24 hr (M)
Same as chlorpromazine.
Thiothixene
High
D2 > 5-HT2
Oral and IM
35 hr (M)
Additive effects with anticholinergic and CNS depressants. Concurrent use of a β-adrenoceptor antagonist may increase serum levels of both drugs.
Haloperidol
High
D2 > 5-HT2
Oral and depot IM
24 hr (M)
Barbiturates and carbamazepine decrease serum levels. Quinidine increases serum levels.
Loxapine
Medium
D2 > 5-HT2
Oral and IM
20 hr (M)
Concurrent use of an antidepressant may increase serum levels of both drugs.
Atypical Antipsychotics
Clozapine
Low
5-HT2 = D4 and > D2
Oral
24 hr (M)
Not established; possible interaction with drugs that induce or inhibit cytochrome P450 isozyme CYP1A2.
Olanzapine
High
5-HT2 > D2
Oral
30 hr (M)
Same as clozapine.
Molindone
Medium
D2 > 5-HT2
Oral
2 hr (M)
Additive effects with anticholinergic and CNS depressants. Concurrent use of a β-adrenoceptor antagonist or an antidepressant may increase serum levels of both drugs.
Risperidone
High
5-HT2 > D2
Oral
24 hr (M)
Not established; possible interaction with drugs that induce or inhibit cytochrome P450 isozyme CYP2D6.
Pharmacokinetics
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Psychotherapeutic Drugs
Only gold members can continue reading. Log In or Register to continue