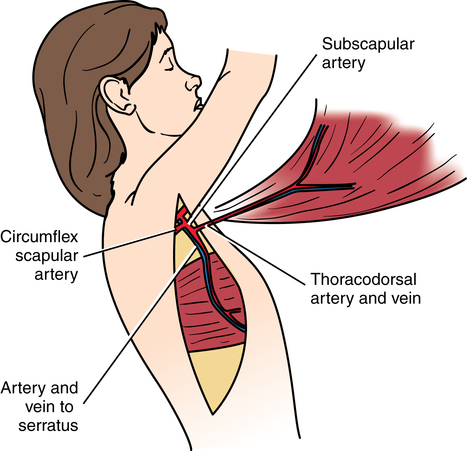
Chapter 40 After studying this chapter, the learner will be able to: • Identify pertinent anatomy of the integumentary system. • List four primary reasons for plastic surgery. • Differentiate autografts, allografts, and xenografts. • Describe the techniques of skin and tissue grafting. • Discuss the importance of fluid balance in the burn patient. Plastic surgery has been called the “surgery of millimeters” because of the critical margin between good and poor cosmetic results. Each millimeter lack or excess of tissue can have a psychologic impact on the patient. If the patient thinks his or her appearance has improved, the patient’s personality and self-image may improve, and others may respond more positively to him or her. The term plastic means “to mold or give form.” Replacement tissues or other structural substances come from several sources as follows: • Autograft: Use tissue from self • Isograft: Use tissue from genetically identical person • Allograft: Use tissue from same species • Xenograft: Use tissue from different species • Bioengineered graft: Graft source from combined biologic and synthetic materials 1. Pressure points are protected during prolonged procedures. Microvascular plastic and reconstructive surgical procedures may take several hours to complete. The patient should be positioned on a gel pad mattress. Bony prominences should be well padded to prevent tissue necrosis. 2. Sterile dye, such as methylene blue, indigo carmine, gentian violet, Bonney’s blue, or brilliant green, is often used to outline areas for incision. This can be done with a sterile marking pen or stylus before or after the skin is prepped. Some surgeons will use intravenous fluorescent dye and a black light (Wood’s lamp) to confirm vascularity of a flap. 3. Exposure of both sides for comparison is usually required for surgical procedures on the breast, face, ears, and neck. Photography is commonly used preoperatively, intraoperatively, and postoperatively. Equalization of tissue manipulation and excision is matched to preoperative measurements written on a full-size image of the body part undergoing the surgical procedure. Figure 40-1 depicts the areas marked for facial procedures. The nose is measured in comparison to the distance between the zygomatic arches (Fig. 40-2). Contemporary surgeons are using terrain mapping for procedures such as facial allogenous transplantations (Fig. 40-3). 4. Draping often exposes much skin surface, which is unavoidable. A fenestrated sheet frequently cannot be used. The opening does not give adequate exposure, especially for skin grafting. Use towels, self-adhering plastic sheeting, and minor and medium sheets under and around the areas, according to need, to drape as much of the patient as possible. Drapes can be secured with nonpiercing towel clips, skin staples, or sutures. 5. Local anesthesia is used for many surgical procedures on adults. Epinephrine may be added to help localize the agent, prolong the anesthetic action, and provide hemostasis by vasoconstriction. Care is taken not to use epinephrine in digits, ears, or other areas of terminal blood supply. Short 26- or 30-gauge needles are used for injection. a. The surgeon may administer a digital nerve block for procedures of the finger. The patient’s hand is placed palm down and a hypodermic needle is inserted through the webspace closest to the affected digit. The surgeon will aspirate to check clearance of all vessels. Then lidocaine 1% or 0.05% without epinephrine, 1 mL, is injected in the volar space (the region of the palmer surface). As the needle is withdrawn, 1 mL is injected at the level of the dorsal space (the region closest to the dorsum of the hand). 6. Nos. 15 and 11 scalpel blades are routinely used to cut small structures. Smaller blades, such as Beaver style, may be used. 7. An electrosurgical unit (ESU) pencil may be used to cut or coagulate during incision. Small, handheld battery-operated units are useful for tiny bleeders. Overuse of the ESU can cause devitalization of tissue and delay healing. 8. Instruments must be small for handling delicate tissues. Iris scissors, mosquito hemostats, fine-tipped tissue forceps, and other small-scale cutting, holding, clamping, and exposing instruments are part of the routine plastic surgery setup. Microinstruments are needed for microsurgical techniques. 9. Nerve stimulation may be used to help identify nerves, especially in craniofacial, neck, and hand reconstruction procedures. 10. Bone, cartilage, or skin grafts may be needed. Grafts and tissues can be used from several different sources for surface and subsurface modifications. Graft materials should not be allowed to dry out. Place in a basin with a few drops of saline. Do not place in a folded moist sponge because this could be discarded from the field to the sponge bucket by accident. 11. Prosthetic implants may be used in plastic surgery to reconstruct subsurface soft tissue and cartilage defects. They cannot be used unless there is adequate soft tissue coverage. They cannot be used in an infected area. 12. Suture sizes range from 2-0 through 7-0, depending on the location and tissue, with sizes 8-0 through 11-0 sutures for microsurgery. The material used varies according to the personal preference of the surgeon. Synthetic nonabsorbable and absorbable polymers are used more commonly than are natural materials because they cause less tissue reaction. 13. Atraumatic swaged-on needles of small diameter with sharp cutting edges minimize trauma to superficial tissues. A needle holder with an appropriately fine tip is used with these delicate, curved needles. 14. Skin staples may be used to close skin or to secure skin grafts. 15. Wound closure strips may be used as skin dressings with sutures or to supplement closure with skin staples. 16. Closed-wound suction drainage is frequently used to drain flaps to prevent seroma and hematoma formation. 17. Fine mesh gauze may be used for the contact dressing. This may be impregnated with petrolatum or an oil emulsion, with or without medication, to cover denuded areas. Several types of sterile nonadherent dressings are commercially available. Dry gauze is not used on a denuded area because it adheres and acts as a foreign body, causing granulomas. 18. Pressure dressings may be used after extensive surgical procedures to splint soft tissues and prevent contractures. Even pressure keeps fluid formation in tissues or under a skin graft to a minimum. Commercial compression garments or dressings for various body areas are preferred by some plastic surgeons. Some dressings may be sutured into place. Donor graft sites require bulkier dressings because they have multiple pinpoint bleeders that ooze freely. 19. Stent fixation is a method of obtaining pressure when it is impossible to bandage an area snugly, such as the face or neck. A form-fitting mold may be taped over the nose like a splint. Long suture ends can be tied crisscrossed over a dressing to immobilize it and exert gentle, even pressure. Adults who are dissatisfied with their body image may believe that a change in personal appearance will solve their social, marital, sexual, or business problems.3 The plastic surgeon assesses the patient’s psychologic status, motivations, and expectations before scheduling a surgical procedure. Realistic, attainable outcomes are identified. The patient should be emotionally stable and aware of the potential outcomes. The surgeon should carefully obtain informed consent. Psychologic assessment and preparation are advisable preoperatively and are essential before surgical procedures that may result in disfigurement.3 Extensive reconstruction for severe congenital deformities is done in stages, often over months or years. These patients require prolonged psychologic support and encouragement.3 Four main categories of problems are treated by plastic surgeons: 1. Congenital anomalies, especially in the structure of the face and hands. Other disciplines may surgically treat genitourinary or orthopedic deformities. 2. Aesthetic appearance, especially of the body surface and subsurface, particularly the face and breasts. 3. Benign and malignant neoplasms, especially those leaving large soft tissue defects. Resection of extensive tumors other than those involving the skin or head and neck is not usually within the province of the plastic surgeon initially, but the patient may be referred for reconstructive surgery and rehabilitation. Frequently, reconstructive procedures are done in conjunction with another specialty surgeon at the time of tumor resection. 4. Traumatically acquired disfigurements, especially facial lacerations, hand injuries, and burns. The objective of the plastic surgeon is to restore function as well as body image. Denuded areas of the body are resurfaced by transplanting or transferring segments of skin and other tissues from an uninjured area (donor site) to the injured area (recipient site). The plastic surgeon prefers to transfer tissues of compatible color, texture, thickness, and hair-bearing characteristics. Soft tissue autografts are used whenever possible. They are classified as follows according to the source of their vascular supply (which is essential for viability)16,20: • Free graft: Tissue is detached from the donor site and transplanted into the recipient site. It derives its vascular supply from the capillary ingrowth from the recipient site. Figure 40-4 depicts regions of the body suitable for autologous graft procurement. • Pedicle flap: Tissue remains attached at one or both ends of the donor site during transfer to the recipient site. The vascular supply is maintained from the vessels preserved in the pedicle of the donor site. Advancement flaps, rotational flaps, rhomboid flaps, transverse rectus abdominis myocutaneous (TRAM) flaps, and latissimus dorsi flaps (Fig. 40-5) are forms of pedicle flaps. • Free flap: Tissue, including its vascular bundle, is detached from the donor site and transferred to the recipient site. Composite free flaps may include muscle, bone, and skin. Microvascular anastomoses between arteries and veins in the flap or autograft and recipient site establish the vascularity necessary for viability (Fig. 40-6). Grafting from one area of the body to another requires a process referred to as “take.” The recipient site has to accept the donor tissue for the graft to take or remain as a permanently viable tissue replacement. The skin graft take occurs in three steps. During the first 48 hours, plasma accumulates at the contact area of the graft. This keeps the tissue vitalized before circulation is established.20 The second phase is the start of capillary ingrowth. And the last step is the anastomosis of vascular channels. If the graft does not take, it sloughs off and necroses. A dermatome is a cutting instrument designed to excise split-thickness skin grafts. The thickness of the graft can be calibrated by adjusting the depth gauge. The width of the graft is determined by the width of the cutting blade. Blades are detachable and disposable, which always ensures a sharp new blade for every patient. The cutting depth should always be reset at zero after changing blades. The length, width, and depth of the graft may be limited by the type of dermatome used and the surface from which the graft is procured (Fig. 40-7). Freehand knife dermatomes are used when the surface can be stabilized for precision cutting. The depth of the cut is determined by the setting on the blade gauge and adjusted by turning screws on the handle. Most styles have disposable blades. American surgeons Vilray Blair (1871-1955) and James Barrett Brown (1899-1971) developed a freehand knife that was modified by later plastic surgeons. The original style was designed like a straight razor but was later modified to include a roller for more accurate depth measurement (see Fig. 40-7, C, D). Padgett and Reese dermatomes consist of one half of a metal drum, which is one half of a circle (see Fig. 40-7, B). A metal handle through the center of the drum has an arm on each end. These arms hold the bar that carries the blade. The bar swings around the drum to cut the graft. The size of the graft is limited by the width and length of the drum. An adhesive is placed on both the skin surface and the drum to keep the skin in contact with the drum. The knife blade is moved from side to side as slight tension is exerted on the skin by rotating the drum. The drum-type dermatome is used on flat, open areas because it is bulky. Its use is limited by the body contour and the amount of suitable skin on the donor site. Oscillating blade-type dermatomes may be electric or air powered with compressed nitrogen or air. The length of the graft is limited only by the donor site. The surgeon checks the adjustable-depth gauge before cutting the graft (see Fig. 40-7, A). The oscillating blade, free of vibrations, takes an accurate graft from donor sites that overlie firm structures, such as bone. The oscillating blade-type dermatome generally is not used on the abdominal wall, where underlying support is not firm. The epidermis, including the basal layer of the dermis that generates new skin, is transplanted from a donor site to a recipient site, in which it becomes a part of living tissue in that area. Adherence to healthy underlying tissue and adequate vascularity are necessary for graft take (survival). A fibrin layer forms to bind the graft to the recipient site and to provide nourishment until vascularization is established in the graft. The depth of the graft (Fig. 40-8) varies according to its purpose20: • Split-thickness graft: The epidermis and half of the dermis to a depth of 0.010 to 0.035 inch (0.3 to 1 mm) are removed. The donor site heals uneventfully unless it becomes infected. Split-thickness grafts are widely used to cover large denuded areas on the back, trunk, and legs and can be meshed to cover larger areas. The donor site can be reused in 2 to 3 weeks after healing. • Full-thickness graft: The epidermis, dermis, and occasionally subcutaneous fat at a depth greater than 0.035 inch (1 mm) are removed or elevated. Full-thickness grafts inhibit wound contraction better than do split-thickness grafts and generally are preferred on the face, neck, hands, elbows, axillae, knees, and feet. The donor site is either grafted or closed by primary intention. The donor site cannot be used again in the future. • Composite graft: This graft includes epidermis, dermis, fat, and other structures such as bone, cartilage, nerve, or tendon. A mesh graft makes it possible to obtain a greater area of coverage from a split-thickness skin graft. After removal with a dermatome, the graft is placed on a plastic derma carrier, cut side down. This is a rigid base to keep the graft spread out flat while it is put through a mesh dermatome. This instrument cuts small parallel slits in the graft. When expanded, the slits become diamond-shaped openings (Fig. 40-9). This permits expansion of the graft to cover an area three times as large as the original graft obtained from the donor site. Creation of a pedicle flap may be the procedure of choice to reconstruct deformities of soft tissue loss that will create or that have created an obvious aesthetic or functional disability for the patient. The pedicle, which is the attachment of elevated tissue to the donor site, must contain a vascular bundle to maintain blood supply to the tissue.16,20 Pedicle flaps are constructed from several types of tissues and sources of vascular bundles. Nasal reconstruction is commonly done this way (Fig. 40-10). • Axial vasculature from axial vessels that supply a fairly definite area of skin and subcutaneous tissue: A direct cutaneous artery flows through the length of the flap. • Random or local vasculature from a subdermal plexus: Random flaps do not have a specific blood vessel within the flap. These are usually small flaps created around the head or neck. • Both axial and random vasculature: A deltopectoral flap, for example, has axial vessels from the sternal region and random vessels in the deltoid area. The surface of the dermal-epidermal layer can be increased by implanting a tissue expansion device subcutaneously, close to the defect (Fig. 40-11). Available in many sizes and shapes, the device has a soft, pliable silicone pouch connected by tubing to a self-sealing inflation reservoir. After insertion under a designated area for creation of the skin flap, the pouch is filled with saline by injecting small amounts into the reservoir. Rapid expansion may be achieved immediately in the head or neck area or gradually over a period of weeks to months in other areas. Natural physiologic skin expansion occurs. The dermis stretches and thins while the epidermis duplicates itself without changing thickness. Tissue will increase to about 1½ times the width of the device. A myocutaneous flap incorporates the muscle with its overlying fascia, subcutaneous tissue, and skin. It receives a vigorous blood supply from the vascular pedicle that supplies the underlying muscle (see Fig. 40-6). It may include a neurovascular bundle with nerve fibers to innervate the muscle in the flap. Usually done as a one-stage procedure, myocutaneous flaps can be created from the following and other muscles: Vascularized autografts of bone are superior in strength and are less prone to deossification and structural weakness than are conventional bone grafts. Anastomosis of the vascular bundle with a free rib, for example, may increase the chance of survival of the donor bone graft in a poorly vascularized recipient site (Fig. 40-12).11
Plastic and reconstructive surgery
Special features of plastic and reconstructive surgery
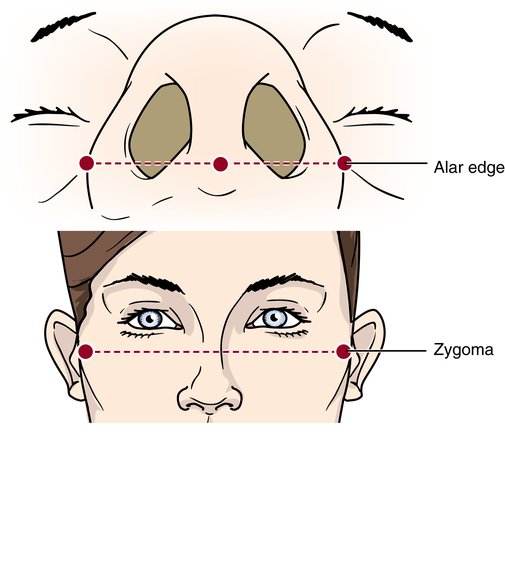
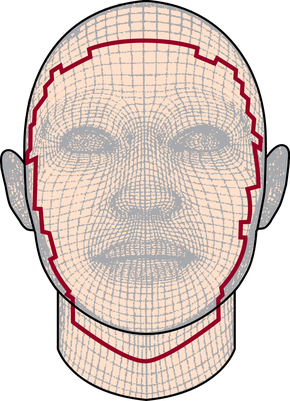
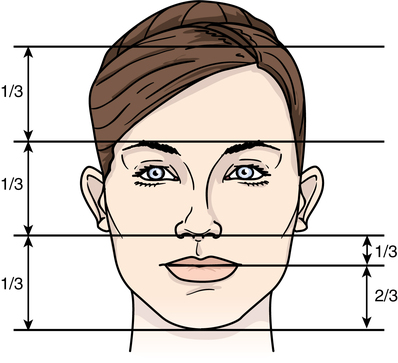
General considerations in plastic surgery
Psychological support for patients undergoing plastic and reconstructive surgery
Categories of plastic and reconstructive surgery
Skin and tissue grafting
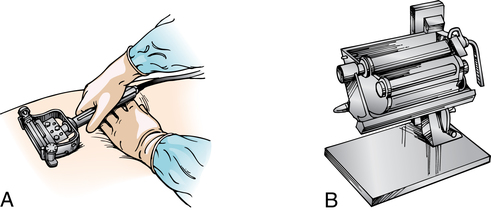
Skin graft knives and dermatomes
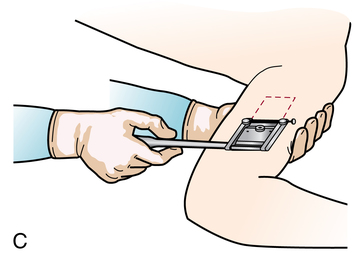
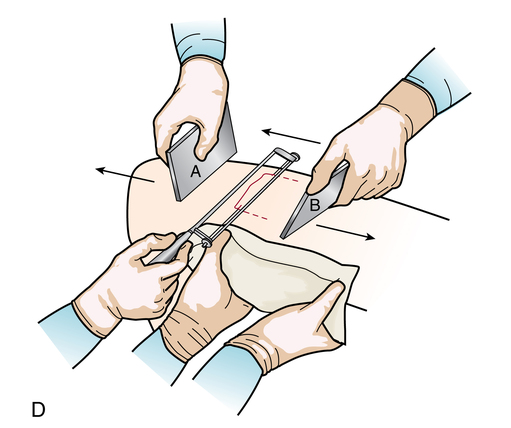
Freehand skin graft knives and dermatomes
Drum-style skin graft dermatomes
Powered skin graft dermatomes
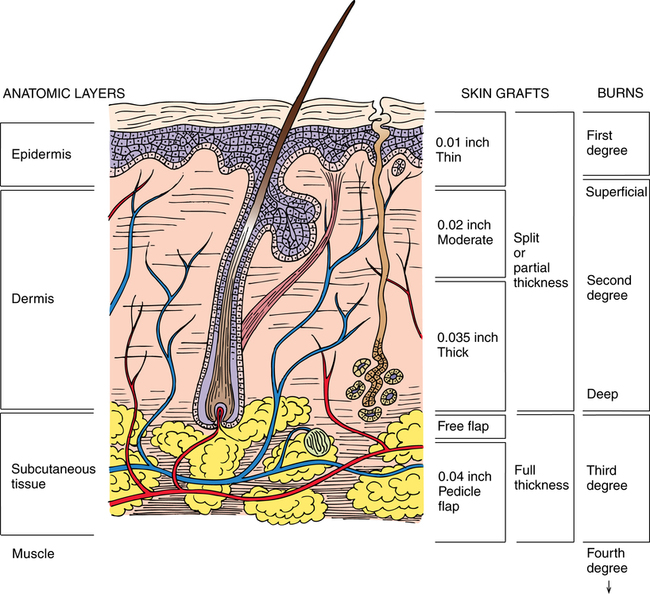
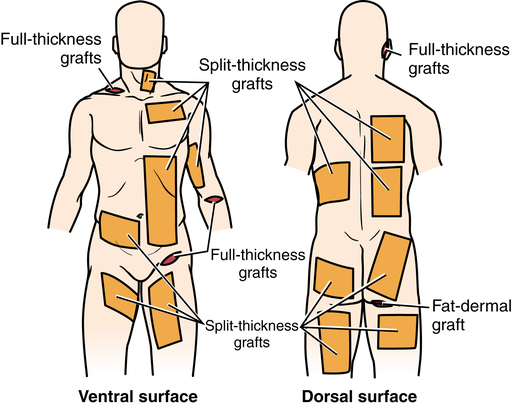
Types of skin and tissue grafts
Skin grafts
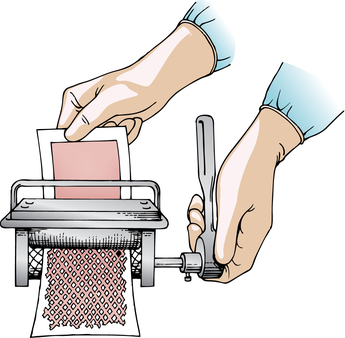
Split-thickness mesh graft.
Pedicle flaps
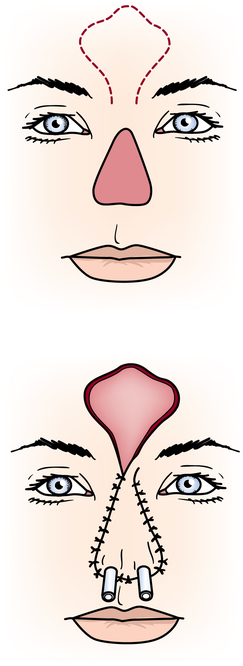
Arterialized tissue flap.
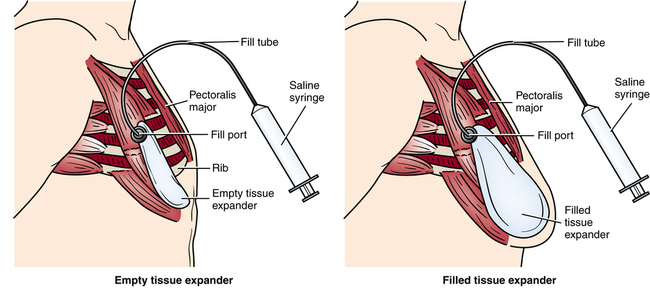
Tissue expansion flap.
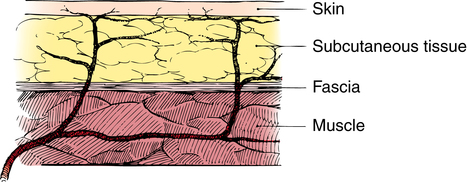
Myocutaneous flap.
Microsurgical free-flap transfer
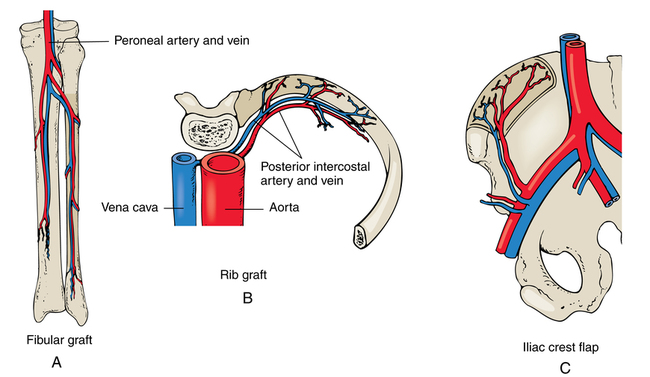
Free autologous bone graft.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 Website
Website