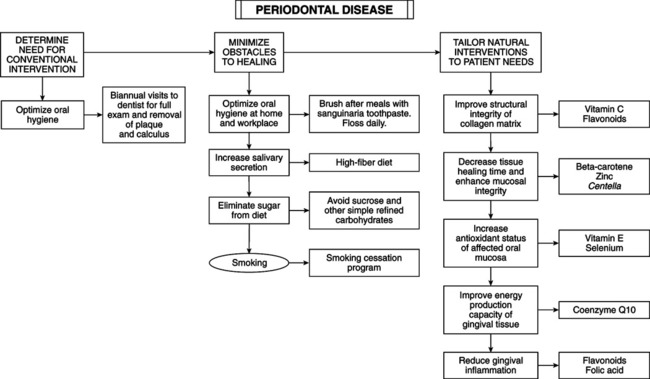
• Alveolar bone loss may be noninflammatory; definition of periodontal disease excludes processes causing only tooth loss (mainly from osteoporosis or endocrine imbalances). These conditions reflect systemic disease. • Focus on the underlying condition rather than PD. Noninflammatory alveolar bone loss is a separate entity that involves a different etiology (see the chapter on osteoporasis). • Focus of this chapter is nutrition and lifestyle improvement as adjuncts to the control and prevention of causes of inflammatory PD. • Best treated with combined expertise of a dentist or periodontist and nutritionally minded physician. Oral hygiene is paramount but insufficient in many cases; host defense must be normalized; nutritional status determines status of host defense factors. Factors involved in host resistance include: • Gingival sulcus: V-shaped crevice that surrounds each tooth, bounded by tooth on one side and epithelium lining free margin of gingiva on the other. Sulcus is ideal for bacteria; it is resistant to the cleaning action of saliva. Gingival fluid (sulcular fluid) is a rich nutrient source for microorganisms. Depth of gingival sulcus is a diagnostic parameter. Patients with PD should be monitored biannually by a dentist. • Bacterial factors: bacterial plaque is the etiologic agent in PD. Bacteria secrete compounds detrimental to host defenses: endotoxins and exotoxins, free radicals and collagen-destroying enzymes, leukotoxins, bacterial antigens, waste products, and toxic compounds. • Polymorphonuclear leukocytes: neutrophils (PMNs) are the first line of defense against microbes. PMN functional defects are catastrophic to the periodontium. PMNs are depressed in the elderly and those with diabetes, Crohn’s disease, Chédiak-Higashi syndrome, Down’s syndrome, and juvenile periodontitis—establishing an extremely high risk for rapidly progressing periodontal disease. Transient neutropenia and PMN function defects may cause alternating quiescence and exacerbation in PD. PMNs release numerous free radicals, collagenases, hyaluronidases, inflammatory mediators, and an osteoclast stimulator. • Macrophages and monocytes: increased numbers in PD. They phagocytize bacteria and debris. They are the primary source of prostaglandins in diseased gingiva, and they release abundant enzymes involved in collagen destruction. • Lymphocytes: produce lymphokines. Their role is overshadowed by other immune components. They promote PMN and monocyte chemotaxis, fibroblast destruction, and osteoclast activation. • Complement system: 22 proteins (>10% of total serum globulin) whose activation initiates cascade (classic or alternative pathway) triggering immunologic and nonspecific resistance to infection and pathogenesis of tissue injury. Products of complement activation regulate the release of mediators from mast cells; pro-motion of smooth muscle contraction; chemotaxis of PMNs, monocytes, and eosinophils; and phagocytosis by immune adherence. Net effect is increased gingival permeability, increased penetration of bacteria and byproducts, and initiation of positive feedback cycle. Other effects include solubilization of immune complexes, cell membrane lysis, neutralization of viruses, and killing of bacteria. In PD, activation of complement by an alternative pathway in the periodontal pocket is a major factor in tissue destruction. • Mast cells and immunoglobulin (Ig) E: mast cell degranulation releases inflammatory mediators (histamine, prostaglandins, leukotrienes, kinins, serotonin, heparin, serine proteases). It is initiated by IgE complexes, complement components, mechanical trauma, endotoxins, and free radicals. Increased IgE in gingiva of PD patients suggests allergic factor in progression of PD in some patients. • Amalgam restorations: faulty dental restorations and prostheses are common causes of gingival inflammation and periodontal destruction. Overhanging margins are ideal for plaque and bacteria. Silver amalgam decreases activities of antioxidant enzymes. Mercury accumulation depletes free radical–scavenging enzymes, glutathione peroxidase, superoxide dismutase, and catalase. Proteoglycans and glycosaminoglycans (GAGs) of collagen are sensitive to free radicals. • Miscellaneous local factors: food impaction, unreplaced missing teeth, malocclusion, tongue thrusting, bruxism, toothbrush trauma, mouth breathing, tobacco. • Tobacco: smoking is linked to increased susceptibility to severe PD and tooth loss. The harmful effects are free radical damage to epithelial cells. Smoking greatly reduces ascorbate, potentiating damaging effects. Carotenes and flavonoids greatly reduce toxic effects of smoking. • Structure and integrity of collagen matrix: collagen of periodontal membrane serves as periosteum to alveolar bone. This allows dissipation of tremendous pressure exerted during mastication. Collagen matrix of periodontium (specifically extracellular proteoglycans of gingival epithelium) determines rate of diffusion and permeability of inflammatory mediators, bacteria and byproducts, and destructive enzymes. Because of the high rate of protein turnover in periodontal collagen, integrity of collagen is vulnerable to atrophy when cofactors needed for collagen synthesis (protein; vitamins C, B6, and A; zinc and copper) are absent or deficient. Collagen of periodontium is rich in GAGs: heparin sulfate, dermatan sulfate, and chondroitin 4-sulfate. Stabilizing collagen is the major treatment goal.
Periodontal Disease
GENERAL CONSIDERATIONS
Pathophysiology
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Periodontal Disease
